Comparing lavage treatment with
local anesthetics of painful jaw
movements at disc displacement
without reduction
- A 3-year prospective study
! "#$% & ! '( %(
) * ''
Abstract
The aim of this prospective and longitudinal study was to compare three-year outcomes of local anesthetics compared to anesthetics, arthrocentesis and lavage on patients suffering from painful jaw locking in the TMJ
The study was performed from 2003 until 2007 and 45 patients were selected from
altogether 55 eligible patients referred for the treatment for TMD to the Department of Stomatognathic Physiology, Faculty of Odontology, Malmö University, Sweden. History questionnaire and clinical examination according toResearch Diagnostic
Criteria, panoramic radiographs and Magnetic Resonance Imaging were completed at
baseline. A questionnaire was sent three years after treatment to 37 patients. Pain intensity, physical functioning, emotional functioning and global improvement were evaluated.
Twenty-five patients were randomised to group anesthetics and 20 patients were randomised to group anesthetics, arthrocentesis and lavage. Thirty-four patients
answered the questionnaire at the 3-year follow-up. In an intention-to-treat analysis
the primary outcome, showing a 30% pain relief, was reported by 28 of 45(62%)
patients at the follow-up. No significant differences in improvement were found
between group local anesthetics and group anesthetics, arthrocentesis and lavage
regarding pain relief, physical functioning, emotional functioning, and global improvement. Significant improvements(P<0.05) were found within both groups regarding pain intensity, physical functioning, emotional functioning and global changes at the follow-up compared to baseline.
Since no differences were found between local anesthetics, arthrocentesis and lavage compared to local anesthetics alone of the TMJ three years after treatment of painful disc displacement without reduction, the use of arthrocentesis and lavage can be questioned.
Keywords: Arthrocentesis, lavage, pain, jaw function, temporomandibular joint disorders
Sammanfattning
Syftet med denna studie var att jämföra tre års resultat av enbart lokalanestesi jämfört mot lokalanestesi ochspolning i käkledenpå patienter som lider av smärtande diskdisplacering utan reduktion
Studien utfördes från 2003 till 2007 och 45 patienter valdes från sammanlagt 55 utvalda patienter för behandling av TMD till avdelningen för Klinisk bettfysiologi, Odontologiska fakulteten, Malmö högskola, Sverige.Frågeformulär och klinisk
undersökning enligt Research Diagnostic Criteria(RDC/TMD), panorama
röntgenbilder och magnetisk resonanstomografi utfördes vid start av studien. Tre år efter behandling, sändes ett frågeformulär till 37 patienter.Intensiteten av smärta, fysisk funktion, känslomässig funktion och global förbättring utvärderades.
Tjugofyra patienter randomiserades till behandling med lokalanestesi och tjugo patienter randomiserades till behandling med lokalanestesi och spolning. Trettiofyra patienter besvarade enkäten vid 3-års uppföljningen. I en intention-to-treat analys visade det huvudsakliga resultatet att 28/45(62%) hade fått 30% smärtlindring vid uppföljningen. Inga signifikanta skillnader fanns mellan grupperna lokalanestesi och lokalanestesi och spolning avseende smärtlindring, fysisk funktion, känslomässig funktion och global förbättring. Det fanns signifikanta förbättringar (P< 0.05) inom båda grupperna avseendesmärtintensitet, fysisk funktion och emotionell funktion och global förändring vid uppföljning jämfört med start av studien.
Eftersom det inte fanns någon skillnader mellan grupperna lokalanestesi och spolningoch enbart lokalanestesii käkleden tre år efter behandling av smärtsam diskdisplacering utan återgång, kan spolning av käkleden ifrågasätts.
Introduction
Temporomandibular disorder (TMD) is a collective term embracing, pain from the temporomandibular joint (TMJ) and/or the masticatory muscles and dysfunctions such as limitations and deviations of the mandibular range of motion and/or TMJ noises during mandibular function(1). TMD pain is the most common reason for patients to seek treatment. As much as 10% of the adult population seeks treatment for TMD pain(2).
Discdisplacement with reduction(DDwR) of the TMJ is found among 30% of the population and 40-53%of these seek care for discdisplacement(3,4). Discdisplacement without reduction(DDwoR) has been reported by 2-4% of patients(4).Pain is often accompanied to the limited jaw functions especially in the early phase of DDwoR. Painful DDwoR has an impact on daily life with consequences on activities in work, school, social and family life(5-7).
In diagnosing Research Diagnostic Criteria for TMD
(RDC/TMD)(1)discdisplacement have been divided into:
• Discdisplacement with reduction.
• Discdisplacement without reduction with limited jaw opening. • Discdisplacement without reduction without limited jaw opening.
According to Diagnostic Criteria for(DC/TMD)(8) one more diagnosis is added(8):
However, the Swedish National Board of Health(SNBH) have used other subdiagnoses as follows(9):
• Symptomatic discdisplacement without reduction. • Symptomatic discdisplacement with reduction.
• Disabling symptomatic discdisplacement without reduction not eased after reversible treatment.
• Disabling symptomatic discdisplacement with reduction that is not eased after reversible treatment.
Different kinds of treatments have been suggested for DDwoR; discectomy was recommended 4 of 10 points and arthroscopy was highly recommended (3 0f 10 points) by the expert group at SNBH. The expert group found that arthroscopy was as cost efficient as arthrocentesis. They concluded that efficiency of arthroscopy is equal to discectomy regarding pain, jaw functions and maximal mouth opening capacity(9). The scientific evidence was low and the conclusion was based on three RCTs including 91 patients with follow-up period of one to five years(6, 10, 11).
Arthrocentesis and lavage is another suggested treatment for DDwoR. The SNBH recommended 4 of 10 points and found it more cost effective than discectomy. Arthrocentesis and lavage is a minimal invasive surgery where the joint is punctured by a needle and flushed. The efficiency of arthrocentesis is equal to arthroscopy regarding pain, however less efficient regarding maximal mouth opening capacity. As regards to jaw functions, the SNBH have used expert assessment concluding that
scientific evidence consisted of two RCTs follow-up 12 months and 26 months that
have compared the effect of arthrocentesis with arthroscopic treatment(12,13).
Besides invasive treatments, reversible treatments should be taken into consideration in patients with DDwoR such as stretching, stabilization appliance,
occlusal correction, transcutaneous electrical nerve stimulation,
sodiumhyaluronat intra-articularly, and glucocorticoid combined with local
anesthetics applied by iontophoresis(Table 1). However, in some patients non-surgical treatment is unsuccessful and discectomy must be seen as an option. (14,15).
Seven reviews have concluded that there is a need of more evidence regarding treatment for DDwoR(Table 2). In the meta-analysis by List and Axelsson(16) it was found that arthroscopic surgery and arthrocentesis had a high rate of success in pain relief and mandibular functioning. However, as many of these studies were of low quality scores the effect of maxillofacial surgery on TMD pain is still unclear.
There are many studies performed in this topic, but only three randomised controlled trials(RCTs)(Table 3). In the study by Schiffman et al(6) the patients were randomised to four different strategies and they were followed in 60 months. The four strategies did not differ in magnitude regarding improved function or pain relief. They concluded that TMJ closed lock should consist of medical management or rehabilitation to avoid unnecessary surgery. Lately a single-blind RCT, Sahlström et
al(17) found that the use of lavage to supplement extra-articular local anaesthetic
treatment of painful jaw movements at non-reducing discs does not appear to improve TMD pain and mouth opening capacity in the short-term(17).
There is a need of long-term follow-ups to test the sustainability in effects of arthrocentesis and lavage.
The aim of this prospective and longitudinal study was to compare three-year outcomes of local anesthetics (A)compared to local anesthetics, arthrocentesis and lavage (AL) on patients suffering from painful jaw locking in the TMJ.
The first hypothesis was that patients treated with arthrocentesis and lavage would experience a greater reduction on TMD pain than those treated with anesthetics alone. The second hypothesis was that three years after treatment the patients in group AL were experiencing less intense TMD pain, better physical functioning, better emotional functioning and had a better global improvement compared to group A.
Material and methods
Patients and study design
In this longitudinal study 45 patients were selected three years after treatment. These
patients belonged to a RCT performed from June2003 until November 2007 at Malmö
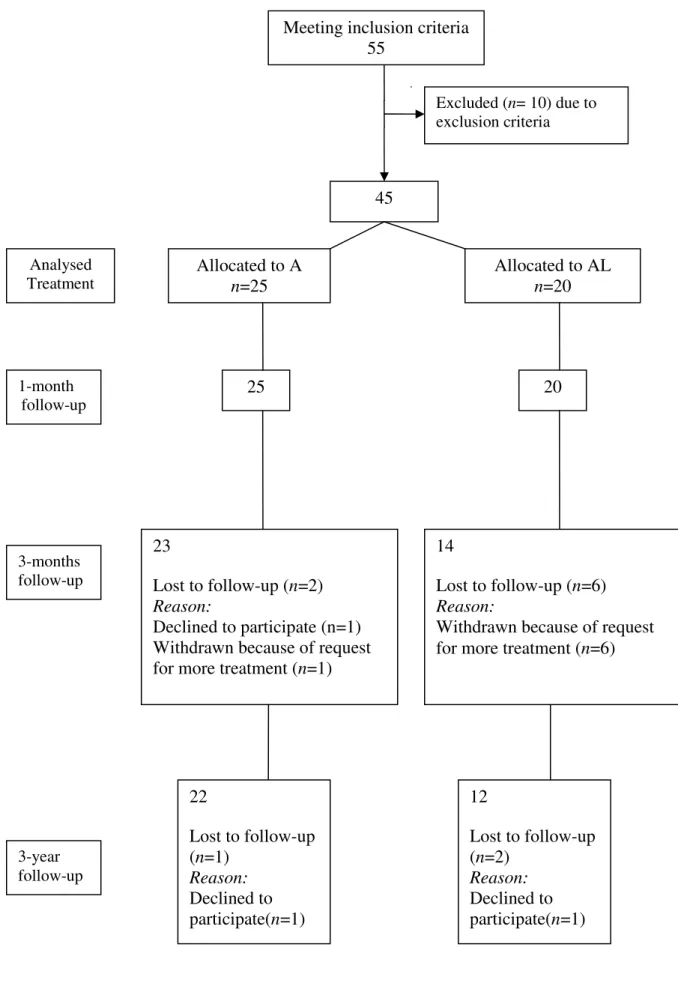
University, Sweden. Forty-five patients (Figure1) with the diagnoses DDwoR and arthralgia according to RDC/ TMD were selected from altogether 55 eligible patients referred for the treatment for TMD to the Department of Stomatognathic Physiology, Faculty of Odontology, Malmö University, Sweden(17).
The inclusion criteria were as follows: 18 years.
Increased pain on chewing or during maximal mouth opening. Pain duration of at least 3 months.
Rate at least 3 on a 0-10 numeric rating scale(NRS) for TMD pain. 0 = no pain and 10 = worst pain imaginable.
MRI verification of disc displacement without reduction.
A RDC/TMD diagnosis of disc displacement without reduction and arthralgia.
The exclusion criteria were as follows: Pregnancy.
Diagnosed systemic muscular or joint disease(ex. Rheumatoid arthritis, fibromyalgia).
Difficulties with the Swedish language. Dental causes for the pain.
Disturbed coagulation ability. Tumours of the TMJ.
Pacemaker or other contraindications for MRI. Whiplash-associated disorder.
Randomization
Patients were randomised to one of two treatment groups: group A - local anesthetics, or group AL - local anesthetics, arthrocentesis and lavage. Assignment to treatment option occurred thus: Five large “block” envelopes, each containing 10 opaque, sealed
“treatment” envelopes, were assembled. More detailed information is described in the short-term RCT(17).
Treatment
In both groups of patients the TMJ was scrubbed with 70% alcohol and 2.5 ml Xylocaine-adrenaline 20 mg ml was injected for auriculotemporalis block. In group AL a needle was injected in the posterior part of the upper joint cavity. A
second, wider needle was injected in the same cavity.The TMJ was then rinsed with
50 ml of saline.
Outcome measures
History questionnaire and clinical examination according to RDC/TMD, panoramic radiographs and Magnetic Resonance Imaging(MRI) were completed at baseline. The clinical diagnosis DDwoR was confirmed by MRI. Three years after treatment, a questionnaire was sent to patients participating in the 3-months follow-up(Figure 1).
A reminder was sent to 10 patients. The follow-up questionnaire was designed
after recommendations from Initiative on Method, Measurement, and Pain Assessment in Clinical Trials(IMMPACT) formed by Dworkin et al(18). According to these recommendations following parameters were studied: Pain, Physical
functioning, Emotional functioning, Global improvement, Symptoms and Adverse
events and Participant disposition (Table 4).
Responders to treatment were patients obtaining a pain relief during jaw movement of at least 30% on the VAS(19).
Improvement in physical functioning was judged as having a decreased mean value on Jaw Functions Limitation Scale (JFLS) and decreased scores on Graded Chronic Pain Severity(GCPS). In emotional functioning improvement was judged when severe and moderate scores at baseline decreased at the follow-up.
Intention – to – treat (ITT) was analyzed for the outcome pain relief of at least 30% on the VAS, improvement in physical functioning, emotional functioning and as well as global improvement.
Statistical analysis
Sample size calculation was determined in a pilot study that compared arthrocentesis with no treatment. A mean ± SD difference of 3.3 ± 3.6 in pain intensity between the groups were found. A group size of 13 patients in each group would yield slightly more than 80% power, with a two-tailed test at the 5% level.
Chi-square test was used to compare the distribution of categorical variables in improvements between groups. Mann-Whitney U-test was used between groups for comparisons for ordinal variables.
For within-group comparisons, the Wilcoxon signed ranks test was used for ordinal variables and McNemartest was for categorical variables.
All inferential statistical tests were two-tailed with a significance level of P 5%. Statistical analyses were done with the Statistical Package for the Social Sciences (SPSS, ver.13.0 for Windows; SPSS Inc., Chicago, IL, USA).
Results
The questionnaire was completed by 34 patients making a response rate of 76%. Thirty-one women and 3 men with the mean age of 35.8 years participated in the study. Before start of the short-term follow-up all patients reported a 49.1±12.8 (±SEM) month duration of pain. Out of the 45 patients, 25 patients were randomized to group A and 20 patients were randomized to group AL (Figure 1).
At the three-year follow-up the responders to the questionnaire did not differ from the non-responders regarding gender, age, CPI and JFLS at baseline. Thus the respondents can be considered to be representative of the initial sample.
Demographic data such as ethnic origin, marital status and highest level of education have been presented earlier and showed no differences between group A and group AL (17).
Between groups
In an ITT analysis the primary outcome showing a 30% pain relief was reported by
28 of 45(62%) patients at the follow-up. No significant improvement was found
between groups A and AL regarding pain relief, physical functioning, emotional functioning, and global improvement (Table 5).
Pain
Average CPI decreased significantly at the 3-years follow up within both groups (group A: P=0.000, group AL: P=0.003), without any difference between groups (Table 6).
Physical functioning
A significant improvement was found in JFLS within both groups (group A: P=0.000, group AL: P= 0.003). A low rate of functional limitation was found at the 3-years follow-up(Table 6).
No difference (P>0.05) was found in number of patients consuming analgesics within groups (Table 6).
GCPS decreased significantly within group A (P= 0.000), but not in group AL (P=0.061). At the follow-up 23 patients scored no or low disability and low pain intensity compared to 5 patients at baseline (Table 6).
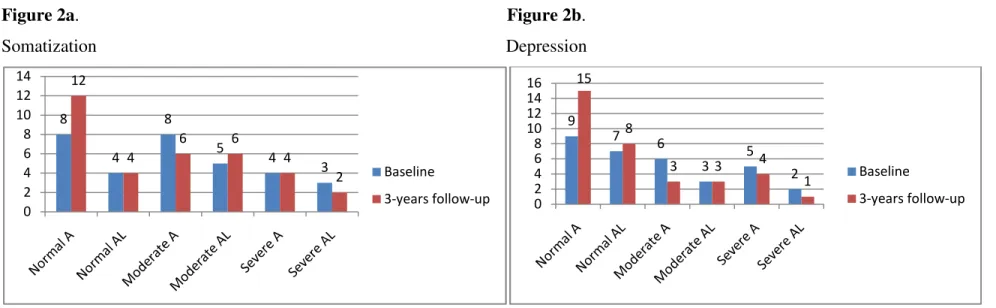
Emotional functioning
Significant improvements were found within both groups for somatization (group A: P=0.000, group AL: P= 0.012) and depression (group A: P= 0.000, group AL: P= 0.004) (Figures 2a and 2b). No differences in improvement were found between group A and group AL for somatization (P=0.389) and for depression (P=0.913) at the follow-up.
Global improvement
Much better or complete improvement with the treatment was found in 24 patients(54%) at the follow-up, with no difference between groups (P= 0.086) (Table 5).
Symptoms and adverse events
An improvement (slightly better to much better) in general health was reported by 11 patients in group A, and by 6 patients in group AL at the follow-up, without difference between groups (P=0.683). At baseline 6 patients reported their general health to pretty poor or poor.
Five patients (group A= 3 patients, group AL= 2 patients) of 34 patients reported additional treatments over time at the 3 year follow-up, with no difference between groups (P= 0.086). The different additional treatments received, were occlusal appliance, occlusal adjustment, physical therapy and one patient in group AL received TMJ surgery
Participant disposition
Discussion
The first and second hypotheses had to be rejected since no differences were found between local anesthetics, arthrocentesis and lavage compared to local anesthetics alone of the TMJ regardingpain intensity, physical functioning, emotional functioning and global improvement three years after treatment of painful DDwoR.
Arthrocentesis and lavage have been widely used since it was first described in 1991 by Nitzan(20). It is a common used technique and several studies have been performed(6, 12, 13, 17, 20-30). The literature on the subject is often clinical studies without control groups or are studies testing the pressure or testing the ideal volume of lavage(22-28, 30, 31). We used 50ml, but according to Kaneyama et al(29) a volume between 300-400ml is the ideal volume for washing out bradykinin, interleukin-6 and proteins from the TMJ. This could be an explanation to not having found a difference in results between groups in our study. Most studies have reported a positive effect of arthrocentesis and lavage. However, none of these studies were RCTs, making the results to be of lower evidence. Recently, one RCT has been published showing no superior effect on painful DDwoR by TMJ lavage and local anesthesia compared to local anesthesia (17).In that study the authors questioned to use lavage to treat patients with DDwoR. Their results are in line with the results from our prospective longitudinal study. Systematic reviews have concluded that arthrocentesis is no better than arthroscopic surgery or not efficient to treat DDwoR (32, 33, 35).
lies in that there is a lack of scientific basis and that the effect does not affect the main problem. However, of all the irreversible treatments arthrocentesis and lavage is the least invasive. The SNBH gave arthrocentesis and lavage a 4 on a 10 point scale when treating DDwoR and found it more cost effective than discectomy. Since the result of this long-term follow-up showed a sustainable positive treatment outcome compared to the short term evaluation and with no difference between groups of treatments at the short and long-term follow-ups, the low score of 4 of 10 by the SNBH for arthrocentesis and lavage in patients with painful DDwoR could be questioned.
Except for patient´s satisfaction with treatment and adverse events, we have followed the guidelines of the CONSORT statement and the IMMPACT recommendations(18). It is a shortcoming to neither have used satisfaction with treatment nor adverse events as such assessments provide information about the clinical importance of safety and tolerability outcomes. These guidelines of IMMPACT show important indicators of a patient’s health. The IMMPACT recommendations are mainly appropriate in RCTs that tries to verify the effectiveness or usefulness of treatments for chronic pain(18). Following guidelines gives these kinds of studies more reliability and stability, because evidence is based on accurate measures. It also gives the skillfulness to evaluate changes over time and to distinguish between treatments, especially between a placebo and an active treatment(18). This study has followed the IMMPACT recommendations by using almost all core outcome measures except patient´s satisfaction with treatment(18).
The outcome at 3-years showed that the same result was achieved regardless of intervention improved regarding TMD-pain intensity, physical functioning, emotional functioning and global improvement.
Patients obtaining a pain relief during jaw movement of at least 30% on the VAS represent a clinically relevant result(19). Therefore IMMPACT has recommended using this outcome as responders to treatment in studies with chronic pain patients(18). Using pain relief as a primary outcome on VAS or NRS show superior responsiveness in detecting improvement associated with pain management (IMMPACT)(18).In this long-term follow-up, the success rate of intervention in patients with painful jaw locking was 62%, and no difference was found between groups of treatments. Improved pain intensity showed that CPI decreased significantly at the 3-years follow up, and showed a lower value than inclusion criteria of 3 on NRS.Our results regarding pain are in accordance with other long term follow-up studies (6, 12, 23, 27, 36). These studies have used pain as their primary outcome measure and the overall success varies from 87% to 98%. In the 5-years follow-up by Alpaslan et al it was concluded that arthrocentesis is a valuable treatment modality for DDwR and DDwoR(27). However, in their retrospective study a questionnaire was sent to patients previously treated with arthrocentesis making the conclusion to be of lower scientific value(27).
Chronic pain interferes with activities of daily living and it has been assumed that
relief of pain is accompanied by improvement in function(18).Our study is based on a
questionnaire and no clinical examination has been performed. Patients with painful DDwoR often also have an impaired opening capacity. In the present study JFLS has been used, and this instrument is described as comprising all movements related to preparing food for swallowing(37). The instrument includes functions such as opening wide enough to bite from a whole apple and chew tough. These and other functions are often impaired in patients with painful DDwoR. In this study JFLS
showed high disability and low limiting physical functioning at baseline, and a significant improvement was found in the long run. Other long-term follow-up studies have measured mouth opening capacity and pain, but not evaluated other jaw functions such as JFLS (6, 12, 22, 23, 27). Five long-term follow-up studies showed overall success 87-100% concerning pain and mouth opening (6, 12, 22, 23, 27). In the RCT by Goudot et al, an increased mouth opening capacity was specifically found amongst 69% of the patients one year after baseline (12). One explanation to an improvement in jaw function over time could be a result of pain relief, but also be related to the course of the disorder(38).
Consequences to chronic pain can be seen in psychological distress and psychiatric disorders, such as depression, anger and anxiety(18). Emotional functioning parameter showed significant differences within-group for somatization and depression at the follow-up in our study. This parameter was measured with SCL-90R subscales for depression and somatization. This result is contrary with the results from the short-term RCT (17). In the short-term study there was no significant improvement for depression and somatisation within groups. One explanation to the difference in results between the short- and long term follow-ups could be that emotional functioning shows consequences to chronic pain and a longer period of improvement may be needed for the patient to get an improvement in emotional functioning. Only one follow-up study has measured emotional functioning, showing that the patients have registered depression as 1.8 and somatization as 2.0 at baseline(6).This is in accordance to our study, where 34 patients rated depression as 1.7 and somatization as 1.8 at baseline. These results show that painful DDwoR have a high impact on emotional functioning among these patients.To the authors
knowledge no other studies have evaluated the long-term follow-up effect on emotional functioning in patients with painful DDwoR. Therefore, more studies are needed to confirm our result concerning emotional functioning parameter.
Participant rating of global improvement showed that slightly better or complete improvement with the treatment was found in 54% of the patients. None long-term follow-up have measured global improvement making it difficult to compare our results with others.
In several systematic reviews, RCTs are called for to be able to make conclusions of higher levels of evidence(32-35, 39, 40).In a long-term follow-up intervention study it is of interest to follow and test if the short-term outcomes are sustainable. In this study we found good effects in the long run indicating a good prognosis for patients with painful DDwoR. However, one should be aware of that the three-year result may have also been influenced by other aspects such as spontaneous remission and placebo. Regression to the mean is another influencing factor as patients are referred when they have the most severe pain and the evaluation tend to be closer to the mean at the second evaluation and especially in fluctuating disorders as TMD(41).
Another factor important for a positive treatment outcome in a long-term perspective is additional treatments after the first intervention. However, in this study only five patients reported additional treatments, making this factor of minor importance for the result of this study. This is in line with the long-term RCT by Schiffman et al where two patients required surgery and in another long-term study by Goudot et al, where four patients referred to a specialized “pain consultation team” for treatment with a multidisciplinary approach (12).
Drop-outs are common in clinical long-term follow-ups. However, only three patients did not respond to the questionnaire in the present study. One shortcoming of this study was that the questionnaire was not sent to the randomised 45 patients. However, as improvement in pain, physical functioning, emotional functioning and rating global improvement were analysed as ITT this may not have affected the results.
Conclusion
Since no differences were found between local anesthetics, arthrocentesis and lavage compared to local anesthetics alone of the TMJ regarding pain intensity, physical functioning, emotional functioning and global improvement three years after treatment of painful DDwoR, the use of arthrocentesis and lavage can be questioned.
Acknowledgements
The authors extend warm thanks to DDS Lotta Englesson-Sahlström, who performed the treatments and Professor Lars Eriksson who initiated the study.
17.
Table 1.
Different kinds of reversible treatments recommended for disc displacement without reduction (DDwoR) according to the Swedish National Board of Health(9) from grade 3-10.
DDwoR Grade
Stretching 4
Stabilisation appliance 6
Occlusal correction 8
Transcutaneous electrical nerve stimulation 9
Sodiumhyaluronat intra-articular 10
Glucocorticoid combined with local anesthetics applied by iontophoresis
Table 2.
Systematic reviews including evaluation of arthrocentesis and lavage in patients with painful DDwoR.
Study Study
published
Contents Typeofstudy Conclusion
best>less
Kropmans et al.(32) 1999 Treatmentofdiscdisplacement Systematic review Arthroscopic surgery = arthrocentesis = physical therapy on MMO and pain intensity.
Methodological outcome studies are needed.
Reston et al. (39) 2003 Surgical treatments vs nonsurgical therapies for treatment of TMD Meta-analys Surgical treatments > nonsurgical therapies. Better designed trials are needed.
Nitzan et al.(33) 2006 Arthrocentes- indications Litterature overview Arthrocentesis is not efficient to treat DDwoR, DDwR and fibrous adhesions.
Al-Belasyet al.(34) 2007 Arthrocentes for the treatment of diskdisplacement without reduc Systematic review No good prospective RCTs have been performed Guo C et al.(35) 2009 Artrocentes for treatment of TMD Systematic review Arthroscopic surgery = arthrocentesis
More RCTs are needed. List T et al. (16) 2010 Treatment of TMD - supported by systematic reviews and
meta-analyzes
Systematic meta-analys
Evidence for surgery and arthrocentesis is insufficient “More well-designed primary studies with proper evidence-based standards are needed to identify the patients who are most suited for surgical
interventions”.
Tozogluet al.(42) 2011 A review of techniques of lysis and lavage of the TMJ. Systematic review Different techniques are required to treat the patient with less complications.
Mio - Maximum incisal opening, CLM- Contralateral movements, ROM- Mandibular range of motion, VAS- visual analog scale, TSO -Time since pain onset, CMI-Craniomandibular index, SSI-Symptom Severity Index, MMO-Maximal Mouth Opening
Table3.
Clinical studiesorrandomized controlled trials (RCTs) onarthrocentesis and lavage in patients with painful disc displacement without reduction.
Study
Study published
Contents
Evaluation Size Treatment Follow-up
Result(successrate%) Best>Less
Murakami et al.(21) 1995 Short-term evaluation of treatment for TMJ closed lock in a clinical controlled study
Pain(VAS) 63 20 25 1. Nonsurgical treatments 2. Arthrocentesis 3. Arthroscopic surgery 6-months 3>2>1 1:56% 2:70% 3:91% Dimitroulis.et al.(23) 1995 Arthrocentesis and lavage for the treatment
of diskdisplacment - an evaluation of a clinical study
Pain(VAS) MMO
46 Arthrocentesis 6 to 30 months 98% overall successrate
Hosaka(24) 1996 Results of treatmentwith arthrocentesis for diskdisplacement - 3-years evaluation of a clinical study
Pain(VAS) MMO 20 Arthrocentesis 6-months 3-years 70% at 6 months 78,9% at 3-years Fridrich(13) 1996 Prospective comparison of arthroscopy and arthrocentesis for
treating the TMD, a prospective, randomized study
Pain(VAS) MIO 8 11 1. Arthrocentesis 2 Arthroscopy 1 week 1, 3, 4, 12, and 26 months 1=2 1.82% 2. 75%
Nitzan et al.(36) 1997 Treatment with arthrocentesis diskdisplacement without
reduction in a clinical study
Pain(VAS) MMO,CLM
39 Arthrocentesis 6 to 37 months 95% overall succesrate Goudot, et al.(12) 2000 Treatment of pain in
the TMJ with atroskopy and arthrocentesis, a RCT
Pain(VAS) MMO 29 33 1. Arthrocentesis 2. Arthroscopy
1 year 1=2 for Pain(VAS) 1<2 for MMO Yura et al.(26) 2003 Arthrocentesis for the treatment
of discdisplacementwithoutreduction in a clinical study
Pain(VAS) MMO
6 Pressure at lavage1.High pressure 2. Low pressure
1 week 1 Month
1>2 Alpaslan et al.(27) 2003 5 years retrospective evaluation of treatment
with arthrocentesis in a clinical study
Pain(VAS) MMO
34 Arthrocentesis 22 Months 87% overall successrate
Kaneyama et al.(29) 2004 The ideal volume of the lavage to remove bradykinin, IL-6 and proteins from theTMJ with arthrocentesisin a clinical study
Pain(VAS) MMO
17 Ideal lavage volume: 1.50 ml, 2.100 ml, 3.200 ml 4.300 ml, 5.400 ml
3-months 5>4>3>2>1
88% overall successrate Emshoff et al.(28) 2005 Clinical factors that affect treatment with arthrocentesis in a
clinical study
Pain(VAS) TSO,ROM
64 Arthrocentesis 2-months 53%overallsuccessrate
Yura et al.(25) 2005 The relationship between arthrocentesis efficiency, pressure and TMJs statein a clinical study
pain(VAS) MMO
65 Arthrocentesis 1-month
2-months
97-98% overall successrate
Schiffman et al.(6) 2007 Four therapeutic strategies for discdisplacement without reductionsingelblind, RCT CMI SSI 10 6 1. Medical management. 3. Rehabilitation.
3. Arthroscopic surgery with post-operative rehabilitation(arthrocentesis)
4.Arthroplasty with post-operative rehabilitation
3, 6 , 12 , 18, 24, 60 months
1=2=3=4
Shinya et al.(30) 2011 The relationship between arthrocentesis efficiency, pressure and TMJs statein a clinical study
MMO Pain(VAS)
50 Arthrocentesis 8 weeks 90-94% overall success Sahlström et al.(17) 2013 Artrocentes in the treatment of diskdisplacement without
reduction RCT, dubbelblinded
45 1. Arthrocentesis and anesthetics 2. Anesthetics
1-month, 3-months
Table 4.
Recommended core outcome measures according to Initiative on Method, Measurement, and Pain Assessment in Clinical Trials, IMMPACT, formed by Dworkin et al for randomised controlled trials of chronic pain treatment.(18)
Outcome measures:
Pain intensity, physical functioning, emotional functioning, global improvement, symptoms and participant disposition.
Pain intensity Visual analogue scale (VAS) was used to describe the patients´ highest level of actual pain a 100 mm. Ranging from 0= “no pain” to 100 = “intolerable pain” The patients recorded in a pain diary once a day for 7 days. Chronic Pain Intensity (CPI) was used and calculated and is describing the mean value of the worst, present and average TMD-related pain for the duration of the last 6 months rated on a 0-10 Numeric Rating Scale (NRS) .On average measures calculated for the week at baseline and at the follow-up.
Physical functioning Jaw Functions Limitation Scale (JFLS) included 21items:chew hard bread, chew crackers, chew chicken, chew tough food, smile, talk, swallow, yawn, look angry, wrinkle eyebrows, kissing, looking happy, laughing, looking sad, singing, speaking, eat soft food and open wide enough to: drink from a cup, for biting an apple, a sandwich and to speak.
Analgesic use: the patients registered how many analgesic they consumed during 1 week before baseline and during 1 week before follow-up. Graded Chronic Pain Severity (GCPS): 7 questions about pain intensity, interference in daily activities, and disability days to yield a 0-4 score, was used. Grade 0 is defined as no pain, grade 1 as TMD-pain of low intensity, grade 2 as high-intensity pain, grade 3 and 4 reveal moderate to considerable pain related to psychosocial disability regardless of pain level.
Emotional functioning Somatization and depression (SCL-90-R) values was used and calculated.
Somatization was assessed using 12 items. Depression was assessed using 20 items.
Participant rating of global improvement and satisfaction with treatment
Global improvement was measured using a 0- 6-point rating scale(much worse, somewhat worse, unchanged, somewhat better, much better and complete improvement)
Symptoms and adverse events Symptoms and adverse events such as additional treatment over time and improvement of general health (Much better, slightly better, the same, slightly worse and much worse than a year ago) were measured.
Participant disposition Detailed information regarding participant recruitment and progress through the trail, including all information specified in the CONsolidated Standards of Reporting Trials (CONSORT) guidelines were followed.( Fig 1)
Table 5.
Distribution of number of patients with painful disc displacement without reduction showing improvement in pain intensity measured on visual analog scale (VAS), physical functioning by using jaw functioning limitation scale (JFLS) and graded chronic pain severity (GCPS), emotional functioning and global improvement three years after treatment.
Group A= local anesthetics, Group AL=local anesthetics, arthrocentesis and lavage
Improvement Group A n=25 Group AL n=20 P-value n % n % Pain relief >30% on (VAS) 18 72 10 50 0,543 Physical functioning JFLS GCPS 17 68 10 50 0,381 13 52 9 45 0,075 Emotional functioning Somatization Depression 6 24 4 25 0,066 7 28 3 15 0,702 Global improvement 16 64 8 40 0,801
Improvement in JFLS was measured as decreased mean value, and improvement in GCPS was judged when score decreased to a lower grade. In emotional functioning improvement was judged when severe and moderate scores at baseline decreased to a lower grade.
Table 6.
Distribution of mean value of characteristic pain index (CPI) and jaw functional limitation scale (JFLS), number of analgesic consumers due to TMD pain, and graded chronic pain severity (GCPS, number of patients grading as 0= no disability, 1= low disability and low intensity, 2= low disability and high intensity, 3= high disability with moderately limiting, 4= high disability with severely limiting) in patients with painful disc displacement without reduction at baseline and at 3 years follow-up.
A AL P-value CPI(±SD) Baseline Follow-up 6,11±0,3(n=21) 1,8±0,5 (n=20) 6,78±0,4 (n=12) 2,3±0,8 (n=12) 0,187 0,925 JFLS(±SD) Baseline Follow-up 2,7±0,3 (n=22) 0,6±0,2 (n=20) 3,6±0,5 (n=12) 1,4±0,6 (n=12) 0,102 0,673 Analgesic consumptions (patients)
Baseline Follow-up 9 (n=22) 5(n=22) 7 (n=12) 4 (n=12) 0,732 0,086 GCPS Baseline (n=20) (n=12) 0,477 0 0 0 1 4 1 2 14 9 3 2 2 4 0 0 Follow-up (n=20) (n=12) 0,803 0 6 5 1 9 3 2 4 4 3 1 0 4 0 0
Figure legends
Figure 1.Flow-chart of the selection of participants from the patients referred for treatment of painful discdisplacement without reduction.
Figure 2.Emotional functioning at baseline and at the 3-years follow-up in patients with painful disc displacement without reduction.
a. Somatization (n=32 at baseline, n=34 at 3-years follow-up). b. Depression (n=32 at baseline, n=34 at 3-years follow-up)
Two patients did not answer the questions about somatization and depression at baseline.
Figure 1. Excluded (n= 10) due to exclusion criteria Allocated to A n=25 Allocated to AL n=20 25 20 23 Lost to follow-up (n=2) Reason: Declined to participate (n=1) Withdrawn because of request for more treatment (n=1)
14
Lost to follow-up (n=6) Reason:
Withdrawn because of request for more treatment (n=6)
1-month follow-up 3-months follow-up 45 Analysed Treatment 3-year follow-up
Meeting inclusion criteria 55 22 Lost to follow-up (n=1) Reason: Declined to participate(n=1) 12 Lost to follow-up (n=2) Reason: Declined to participate(n=1)
Figure 2a. Figure 2b. Somatization Depression / 0 / -0 # ,+ 0 . . 0 + $ + 0 . / ,$ ,+ ,0 1 #23 2 4 5 . # -+ ,-/ # # 0 , $ + 0 . / ,$ ,+ ,0 ,. 1 #23 2