Treatment effects and adherence of van
Beek activator during the first year
comparing two wear-time prescriptions
assessed by microsensors: a randomized
clinical trial
Sofia Myllenberg
Sandra Wither
Supervisor:
Mikael Sonesson, Lecturer, Department of Orthodontics,
Faculty of Odontology, Malmö University
Master Thesis in Odontology (30 ECTS)
Malmö University
ABSTRACT
Aim: The aim of this study was to evaluate the adherence and the changes in overjet among
patients treated with the van Beek activator during the first year, comparing two wear-time prescriptions; 8 hours and 12 hours.
Materials and methods: The study sample consisted of 20 patients, 9 girls and 11 boys, with
a mean age of 10.0 years. All patients were diagnosed with a class II malocclusion and were treated with the van Beek activator. The patients were randomized into two groups with different wear-time prescriptions; 8 hours and 12 hours. The level of adherence was measured with the aid of TheraMon®, a microsensor embedded in the activator. The adherence, overjet
and overbite were recorded after 3, 6, 9 and 12 months of treatment.
Results: In both groups, a reduction of both overjet and overbite was observed. There was no
significant difference between the 8- and 12-hour group for overjet and overbite reduction. The adherence, on the other hand, was better in the 8-hour group during the whole 12-month period.
Conclusions: A wear-time prescription of 8 hours per day displayed a higher level of
adherence than 12 hours in the present trial. No clinically significant differences in treatment effects were detected between an 8-hour and 12-hour wear-time prescription. The level of adherence is higher during the first 6 months of a treatment and is then reduced between 6-12 months
Keywords: adherence, class II malocclusion, overjet reduction, TheraMon, van Beek activator
SAMMANFATTNING
Syfte: Syftet med denna studie var att utvärdera följsamheten och förändringen i det
horisontella överbettet hos patienter som behandlas med en van Beek-aktivator, under det första behandlingsåret, genom att jämföra två rekommenderade användningstider; 8 timmar och 12 timmar.
Material och metod: Totalt 20 patienter, 9 flickor och 11 pojkar, med en medelålder på 10,0
år, ingick i undersökningsmaterialet. Samtliga patienter diagnosticerades med en Angle Class II-bettavvikelse, och behandlades med en van Beek-aktivator. Patienterna delades
slumpmässigt in i två grupper med olika rekommenderade användningstider; 8 timmar och 12 timmar. Följsamhetsnivån mättes med hjälp av TheraMon®, en mikrosensor, inbäddad i
aktivatorn. Följsamheten, det horisontella och det vertikala överbettet registrerades efter 3, 6, 9 och 12 månader.
Resultat: I båda grupperna observerades en minskning av både det horisontella och vertikala
överbettet. Det fanns ingen signifikant skillnad mellan 8- och 12-timmarsgruppen för
reduktion av överbetten. Följsamheten var däremot bättre i 8-timmarsgruppen under hela 12-månadersperioden.
Slutsatser: En rekommenderad användningstid på 8 timmar per dag visade en högre nivå av
följsamhet än 12 timmar, i den aktuella studien. Ingen klinisk signifikant skillnad i behandlingseffekt upptäcktes mellan 8-timmars och 12-timmars rekommenderad
användningstid. Följsamhetsnivån är högre under de första 6 månaderna av en behandling och minskar sedan mellan 6-12 månader.
Nyckelord: adherence, class II malocclusion, overjet reduction, TheraMon, van Beek activator
CONTENTS
INTRODUCTION ... 1
Malocclusions... 1
Angle Class II malocclusion ... 1
Etiology ... 2
Treatment indications ... 2
Early treatment in the mixed dentition ... 3
Treatment alternatives ... 4
Van Beek activator ... 4
Wear-time... 6
TheraMon® ... 6
Compliance and adherence ... 8
The Hawthorne effect ... 8
Aim ... 9
Hypothesis... 9
MATERIALS AND METHODS ... 9
Data evaluation ... 10
Ethical approval ... 11
Clinical importance of the study ... 11
RESULTS ... 11
Participation ... 11
Demographics at baseline ... 12
Loss of data ... 12
Treatment results ... 12
Wear-time and adherence ... 13
DISCUSSION ... 14
Wear-time and adherence ... 14
Wear-time related to gender and age ... 15
Ethical considerations ... 15
Strengths and limitations ... 15
Suggestions for future studies ... 17
INTRODUCTION
Malocclusions
An occlusion is classified by assessing the relationship between the jaws in the sagittal, vertical and transversal plane. There are three types of sagittal occlusions: Angle Class I, II and III, which Edward H. Angle introduced in the beginning of the 1900’s. Angle Class I, normal occlusion, is defined as the mesiobuccal cusp of the maxillary upper first molar should occlude in the buccal groove of the mandibular first molar. Discrepancies up to half a cusp width in either mesial or distal direction are acknowledged as normal (1). It was not until these definitions were established by Angle that dentists began to correct the relationship between the jaws, the occlusion, instead of only aligning irregular teeth (2). The opposite condition to normal occlusion is malocclusion. Malocclusions are not regarded as diseases, but rather varieties from the norm in society, which can lead to functional complications or concerns about one’s appearance. However, a divergence from normal occlusion does not automatically mean that the patient is required to undergo orthodontic treatment. Skeletal deviations can be involved in sagittal, vertical and transversal malocclusions, in combination with dental variations (1). If a malocclusion occurs in the primary dentition, it can often be spontaneously corrected since the occlusion is subjected to changes with jaw growth, dental attrition, mesial drift and increased sagittal mandibular growth. For instance, it is normal for younger children to have a more prognated maxilla with an overjet around 4 mm, but this is usually naturally corrected during growth if there are no oral habits that can interfere (3,4) The primary dentition serves as a guideline for the permanent dentition and thus it is possible to anticipate whether the malocclusion will remain or not. In these cases, it can be valuable to treat the malocclusion in the mixed dentition (3). Large overjets, spacing and crowding is often classified in millimeters, which means that normal occlusions can have small alterations within a spectrum. An overjet up to 5 mm can be considered normal and not an indication for treatment. The treatment need is estimated with the aid of both short- and long-term risk assessment, oral health problems, function, esthetics, and the patient’s subjective desires (1).
Angle Class II malocclusion
In Angle Class II, also called postnormal occlusion, the mandibular first molar has a distal position compared to normal occlusion (1). In both the mixed and permanent dentition, a distal molar position combined with an increased overjet is a common malocclusion (3). The usual patient with an Angle Class II malocclusion has an increased overjet, incomplete lip closure, convex profile, mandibular retrognathism and a deep bite, possibly in combination with gingival impingement. In approximately 90% of Angle Class II occlusions, the maxillary incisors are proclined, Angle Class II division 1, and in approximately 10% the maxillary incisors are retroclined, Angle Class II division 2. In Angle Class II division 1, the overjet is often extended. If it is over 6 mm the overjet is considered great, and over 9 mm it is
considered extreme (1). With an increased overjet there is a higher risk to develop an incomplete lip closure, where the lower lip rests behind the maxillary incisors. This in turn can lead to a further increase of the overjet. An increased overjet can also lead to a
development of a deep bite, which is more common in the permanent dentition. The deep bite is caused by an excessive eruption of the incisors because of a lack of normal contact in the front (3). With a prevalence of 14-18%, Angle Class II is a common malocclusion (1). However, other studies have reported that the prevalence can reach up to 25%, depending on the age of the patient (5).
Etiology
The head and facial structures develop early during the embryogenesis and this continues throughout the growth and, accordingly, the proportions between jaws and head are constantly changing. In other words, the growth is regulated genetically but can be influenced by
epigenetic and environmental factors (3). A class II malocclusion can originate from dental or skeletal deviations, or a combination of both (5). The causes are multifactorial, and it is not uncommon for a skeletal Angle Class II malocclusion to originate from a genetic factor (3). Moreover, the malocclusion can be affected by biting and sucking habits (4,6), mouth breathing, atypical swallowing (3,7), diseases, or conditions such as juvenile idiopathic arthritis in the jaw joint (8). Other reasons for class II malocclusion are mesial migration of
permanent molars in the upper jaw due to an early extraction of the primary second molar (3). However, one of the most common etiological local factors for malocclusions are
non-nutritive sucking habits, where the most common one is digit sucking (3,9), which can lead to proclined incisors (3). Children who use pacifiers tend to quit spontaneously at about three years of age due to new interests and curiosity for other activities. On the contrary, digit sucking tends to be more difficult for children to quit, provided that the habit continues up to the ages of seven to eight. This is partly due to the digit being attached to the body, and partly because the habit is strongly associated with emotional anxiety, primarily in children of older age. There are numerous studies that show that digit sucking habits increase among infants in situations such as tiredness, boredom, exhilaration, and physical and emotional stress. In conclusion, habits that can negatively affect the development of the occlusion, should be observed early to avoid consequences like posterior cross bite, anterior open bite, and Angle Class II malocclusion (9).
Treatment indications
There are several indications for a treatment of Angle Class II malocclusions, such as
improvement of function, decreased risk of trauma, and improvement of quality of life. Most commonly it is a combination of several factors that leads to treatment (1,2,10). The treatment indications for Angle Class II can be viewed from both the clinician’s and the patient’s point of view. The objective treatment indications are those diagnosed clinically while the
subjective indications are the patient’s own concerns. It is important to take all indications into consideration while planning orthodontic treatment (2).
For the patient, an Angle Class II malocclusion may not only implicate unfavorable esthetics due to incomplete lip closure and a convex profile (1), but can also result in an impaired jaw function (2) and gingivitis. It has been observed that patients who mouth breathe or have an incomplete lip closure are subject to chronic gingivitis. Mouth breathing can cause recurrent dehydration of the gingiva anteriorly, which in turn leads to vasoconstriction and a reduced host defense, causing gingivitis (3). Additionally, an Angle Class II malocclusion is very commonly combined with a deep bite which is characterized by a disproportionate vertical overlap of the incisors. Overbite reduction and treatment of deep bite can be done by intrusion of maxillary incisors and protrusion of mandibular incisors, extrusion of the molars, or a combination of both. If an overbite is so extreme that it causes gingival impingement, it is particularly crucial to treat the deep bite. A deep bite in combination with Angle Class II malocclusion can conveniently be treated in the mixed dentition with a functional appliance (1).
Trauma
At the end of the 1970’s, a correlation between large overjets and trauma in the upper incisor region was observed. Most injuries occur between 8 and 11 years of age, which has
emphasized the question as to when it is appropriate to correct large overjets (11). There is a significant relationship between large overjet (5 mm or more), incomplete lip closure and injuries on maxillary incisors (1,11), and the trauma prevalence has been reported between 10-30%. The larger the overjet, the more presence of trauma has been seen and the extent of the overjet influences the severity of the injuries (11). To summarize, there is an increased trauma risk for these children and adolescents due to inadequate protection from the upper lip (1). Accordingly, this indicates the importance of early orthodontic treatment with a
functional appliance to obtain a statistical significant reduction of teeth injuries (5,11,12).
Quality of life
According to the WHO, oral health is important for both general health and quality of life. Good oral health indicates the absence of diseases or conditions that can limit one’s ability to bite, chew, smile, or talk, or negatively affect psychosocial well-being (13). One of the most common oral conditions is malocclusions with a prevalence between 39-93% (10). It has been reported that malocclusions in the esthetic zone have negative effects on oral health related quality of life (OHRQoL), especially in the aspects of social and emotional well-being (14). According to Kallunki et al, children with an increased overjet reported a significantly lower OHRQoL than children with crossbite or normal occlusion. This was studied by letting nine-year-olds fill out a questionnaire with questions about oral symptoms, functional limitations, emotional and social well-being, along with questions about pain in the jaws and face (10). Another recent study on adolescents in Brazil, showed that students who reported negative repercussions after bullying were three times more likely to have a bad OHRQoL than students who had not experienced bullying. It has been shown that an early treatment
increases the patient’s self-esteem and reduces negative social experiences. Even though the clinician generally considers oral health and function as the main indications for orthodontic treatment, psychological and social aspects can often be the major reasons for the patient’s treatment motivation (15). Therefore, it is important to treat every case individually based on the patient’s needs and wishes (5).
Early treatment in the mixed dentition
An early treatment with removable appliances is done in the mixed dentition. The mixed dentition begins when the first permanent mandibular incisors and molars erupt and ends when the last primary tooth is shed. In cases when there is an unfavorable habit involved, it is recommended to use a functional appliance in the mixed dentition to prevent the child from maintaining the habit, namely, interceptive treatment (3). Overjet reduction treatment is often done in two phases; firstly, the interrelationship of the jaws is corrected using an activator apparatus. Secondly, fixed orthodontics can be used to obtain an optimal class I occlusion (1). It has not yet been established whether overjet reduction treatment in two steps is more advantageous regarding cost effectiveness and treatment results. However, one of the benefits of an early treatment is to create better conditions for the skeletal growth pattern (16) even if a second treatment period is necessary (2). Regardless, using removable appliances early in the mixed dentition is beneficial considering it is easy to execute, it is possible to take advantage of the natural growth (5) and pubertal peak (17), and has less impact on teeth and soft tissue (5). Other benefits with early treatment are to avoid trauma of the upper incisors, especially
for children engaged in contact sports, prevent possible extractions of permanent teeth, and also reduce the risk of being bullied because of one’s appearance (16).
Treatment alternatives
There are several different activators to correct a class II malocclusion. Multiple studies have compared the activators to gain a better understanding of treatment alternatives. Altenburger and Ingervall studied the Herren activator, the van Beek activator, and an activator-headgear combination, they concluded that the van Beek activator is an effective alternative when treating class II malocclusion. Although the skeletal effects were the same regardless of the apparatus, there are some advantages with the van Beek, considering the controlled elongation of posterior teeth and satisfactory correction of retroclined lower incisors and proclined upper incisors (18).
Van Beek activator
The van Beek activator is a removable functional appliance used for overjet treatment in the mixed dentition. The activator consists of an acrylic part, two external stainless-steel arms embedded in the acrylate (Figure 1), and a head gear that constitutes the extra-oral high pull (1,7,19). The activator places the mandible in a protruded position. The acrylate covers the entire buccal surfaces of the maxillary incisors but only a quarter of the buccal surfaces of the mandibular incisors (Figure 2), this is in order to inhibit further growth of the maxilla (1,5,7) and stimulate growth of the mandible (2,5). However, the activator mainly contributes dentoalveolar and soft tissue changes (17). The two external stainless-steel arms are
constructed to prevent irritation of the skin by the corners of the mouth. The headgear should be placed in such a way that the force goes through the center of resistance of the maxilla with a force around 300 g per side (7). In cases when the patient has a deep bite, in addition to Angle Class II malocclusion, the apparatus can also raise the bite by allowing an elongation of the lower jaw’s premolars and molars by a reduction of the acrylate occlusally. A correction of the proclined incisors in the upper jaw and retroclined incisors in the lower jaw can also be done (1,19). The treatment period consists of an active phase when the actual correction is done, and a retention phase when the stabilization is achieved to avoid relapse. Studies have shown that treatment with a van Beek activator has resulted in overjet and overbite reduction, an improved positioning of the molars, retroclination of the maxillary incisors, and some proclination of the mandibular incisors. Treatment with a van Beek activator causes some skeletal effects, but the overjet reduction is primarily due to dentoalveolar modifications (19). Rizell et al found that 61,5% of patients who were treated with functional appliances like the van Beek activator, had a successful treatment outcome. The most common reasons for inadequate results were interrupted treatments, or lack of patient compliance (20).
Figure 1. van Beek activator
Fig 1. van Beek activator. Photo: Philipp Scaglia
Figure 2. van Beek activator
Wear-time
The current prescribed wear-time is 12 hours per day, which means that the patient has to use the activator for a few hours during the evening and during the entire night (7). During the night, the pituitary gland secretes more growth hormones than during the day (21). Wang et al. found in a rat study that a combination of functional appliance and growth hormones stimulated mandibular and condylar cartilage growth. Therefore, it is favorable for patients to use a functional appliance during the night (22). It is important to give clear information about possible discomfort during the first days, and that it is normal that the teeth can feel mobile. The patient will be coming for regular follow ups during the treatment period, but still has to be observant of any mucosal irritations. In this case, alterations of the activator should be done (7).
TheraMon
®
TheraMon® is a microsensor which has been shown to be a very effective aid for measuring the level of compliance during orthodontic treatment by controlling the actual time of use (23–25). Studies have shown that in comparison with another microsensor, TheraMon® is more accurate and trustworthy when measuring wear-time of removable appliances (25). The sensor measures 13x9x4,5 mm (Figure 3), and is embedded in the acrylate of the van Beek activator (Figure 4), by the dental technician. When the patient places the activator in the mouth, it is activated by body heat and begins to collect data every 15 minutes and stores it in the integrated memory (23). To send and receive data, the microsensor is equipped with technology that enables the sensor to transfer data to the reading station through magnetic fields. The antenna in the sensor can only be activated if placed within 2-3 cm from the reading station. Inside the patient’s mouth, the antenna is not activated and can thereby not emit any radiation (24). On any occasion during the treatment period, the wear-time graph can be accessed. Reading of the sensor can be done quickly during follow up appointments, which means that the data is obtainable immediately. It appears that recording of wear-time is well accepted among patients, and even serves as a motivation to use the appliance (26).
Furthermore, the small size of the microsensor makes it uncomplicated to incorporate into the activator, and the majority of patients do not experience discomfort due to the sensor itself (27). The success of treatments with removable appliances is dependent on consistent wearing during the entire treatment period (25,26). Therefore, the adherence of the patient is one of many important factors to take in consideration if the treatment result is unfulfilled. However, it is difficult to determine which factor affects the result, it not only depends on the adherence of the patient, but also on biological factors, improper manufacturing of the appliance, or the treatment plan itself. The consequences of not knowing the cause can lead to a longer
treatment period with increased treatment costs, whereupon a microsensor can be used for better monitoring the usage (27). Using a microsensor like TheraMon® can help both the patient and the dentist, since it can raise awareness of possible lack of success in the
treatment. If that is the case, the dentist can either provide additional motivation to improve adherence, or perhaps choose to modify the treatment (26).
Figure 3. TheraMon® microsensor
Fig 3. The size of the TheraMon® microsensor in relation to an orthodontic ruler (0,5 mm grading).
Photo: Philipp Scaglia
Figure 4. van Beek activator with embedded TheraMon® microsensor
Fig 4. TheraMon® microsensorembedded in the acrylic part of the van Beek activator. Photo: Hans Herrlander
Compliance and adherence
It is important to distinguish the terms “compliance” and “adherence”. The word compliance comes from the Latin word “complire”, implying to fill up, in other words, complete an action and fulfill a promise. Adherence, on the other hand, comes from the Latin word “adhaerere”, which means to keep close, or remain constant (28). Compliance is described as how much a patient’s behavior is correlated with the caregiver’s instructions or advice. The term has however been criticized, since it implies that the prescriber determines which treatment is appropriate, and the patient is expected to abide by the instructions, no questions asked. Instead, adherence has recently been used more frequently to better reflect the clinician-patient relationship. Adherence is a process where the suitable therapy is settled after a legitimate dialogue with the patient (29).
The success of orthodontic treatment, using removable appliances, is dependent on many aspects (30). It is important to be clear with the patient and describe the function of the apparatus, the matter of usage and routine follow ups at the clinic, along with the importance of oral hygiene. Furthermore, the patient's parents should be included in all the steps of the treatment, to assure a higher level of compliance. Altogether, a patient’s compliance is the most fundamental aspect of a successful treatment result (31) and inadequate usage will not result in anticipated tooth movement and causes a higher risk of relapse (30). Compliance during orthodontic treatment has a tendency to decline over time, regardless of the initial level (31), and it is often challenging to maintain and increase the patient’s compliance during a treatment. Several techniques have been suggested with the purpose to increase compliance such as gifts, treatment diaries, sticker reminders and hypnosis (30,32). It has been researched how the compliance can be affected depending on the patient’s age, sex, maturity, motivation, personality type and type of apparatus. Studies have shown that prepubertal children
cooperate more than teenagers, and girls in general have shown to be more diligent than boys. However, it does not appear that the type of apparatus is correlated to the compliance of the patient, and there is no statistical significance between intraoral and extraoral apparatuses. Regardless, there is a difference between the actual usage, self-reported usage and prescribed usage. Patients are inclined to report approximately 5 hours longer usage each day than the objective time, and 3 hours longer than prescribed. In two studies a slight increase of
compliance with headgear was observed when the patient was informed that the treatment was supervised (23,30). According to Arreghini et al, patients who believe their malocclusion is unattractive and psychologically troubling are more motivated for treatment. Furthermore, socially extroverted children with high confidence are more involved in their treatment than children who are introverted and hostile. Even though these factors can influence the
treatment result, it is important to remember that they cannot be used as indicators for a bad treatment outcome (23).
All things considered; it can be difficult to determine the reason for a potential lack of
desirable treatment results. Hence, by using an incorporated microsensor, it is possible to gain quantitative data on the usage time and thereby give individual feedback and motivation to the patients (33). It is essential to include the patient from the beginning and make them
interested in the treatment, and by doing so the adherence will increase (27).
The Hawthorne effect
form and being questioned about one’s behavior during evaluation can encourage the patient’s motivation, which can lead to enhanced compliance. Practically all research about people’s behavior is dependent on the participants’ compliance (35). Other examples of behavioral changes are the Novelty effect and the Pygmalion effect. However, the Hawthorne effect is the most discussed phenomena as it can lead to biased results of RCTs in both the medical and dental fields. According to Abdulraheem et al, 3,4% of RCTs mentioned the Hawthorne effect of patients, while no researchers mentioned how the Hawthorne effect can affect the
researchers themselves. It was found that in studies where the patients were aware of an incorporated sensor in a removable appliance, the compliance level was higher than when patients where not monitored with the aid of a sensor (34). Moreover, according to
McCambridge et al, the Hawthorne effect usually disappears after six months of a study (36). To decrease the Hawthorne effect as much as possible for both patients and therapists, it is advised to have a longer observation period than six months (34).
It is not clear whether the prescribed time today is the most efficient for beneficial treatment results (33). For children and adolescents today, there are societal demands on performing well in school along with having extracurricular activities. In addition, there is pressure to fit in and have an appealing appearance from a young age. Consequently, it is realistic to accept that young patients do not have time to use their removable appliances for the prescribed time (23). With this in mind, it is highly relevant to investigate the required wear-time of the van Beek to gain a more evidence based treatment plan (33).
Aim
The aim of this study was to evaluate the adherence and the changes in overjet among patients treated with the van Beek activator during the first year, comparing two wear-time
prescriptions; 8 hours and 12 hours.
Hypothesis
The hypothesis was that there is no clinically significant difference in either treatment progress or adherence between the two groups.
MATERIALS AND METHODS
The present trial is part of a larger multi-center RCT at the Department of Orthodontics at the Faculty of Odontology, Malmö University, and the Department of Orthodontics Center for Specialist Dental Care in Örebro. Initially, the number of participants required for a power set to 90%, was calculated to be 69 patients. The present report is a follow-up of a previous study (37) and displays data from a group of 20 patients who received treatment in Malmö. The trial started in 2015 and is planned to end in 2021.
Patients treated at the Department of Orthodontics, Malmö University with Angle Class II malocclusion were asked to participate in the study, see Table 1 for eligibility criteria. The patients were evaluated by an orthodontist who determined whether they were suitable for treatment with removable appliances. Written and oral information was given to the parents by the researchers, and those who wished to participate signed a form of consent. Information was given that participation was highly optional, personal information would be handled confidentially and only by the team involved in this study, and that the patients at any point
during the study could discontinue their participation. The treatment was executed by teachers and/or students according to standardized protocol for van Beek treatment.
The patients were randomized with the aid of a computer program into two groups: - Group 1: Only night usage, 8 hours/day
- Group 2: Evening and night usage, 12 hours/day
Table 1. Eligibility criteria
Inclusion criteria Exclusion criteria
Children in the mixed dentition and dental stage DS2M1 (i.e. incisors and first molars fully erupted)
Patients with diseases that influence the somatic and/or craniofacial growth Class II malocclusion with an overjet ≥5mm Patients with medication that influence
respiration and/or the craniofacial growth Incomplete lip closure Patients with inadequate language
apprehension upon which an interpreter is required
Possible crowding not exceeding 4mm per
jaw Patients with known agenesis for primary or permanent incisors Patients with earlier extracted primary or permanent teeth
Patients with a diagnosed anterior open bite over -2mm
Patients who had previously been treated with removable appliances
The patients received a removable appliance, a van Beek activator with headgear exerting a force of between 230 and 260 g. The activator was equipped with a sensor, TheraMon®. The patients were informed about which groups they had been randomized into, in other words, how many hours a day they were required to use the appliance. Instructions on how to use and care for the appliance was given, and also information about how the microsensor works, and possible discomfort during the first days of the treatment. The treatment was followed up at the clinic by teachers and/or students every six to eight weeks whereupon the sensor was read, and the data registered in “TheraMon® Cloud”. The overjet and overbite were measured clinically with an orthodontic ruler at every appointment, and the patients were informed about the treatment progress. Potential adjustments of the appliance were made, such as grinding and/or changing the battery in the sensor.
Data evaluation
Evaluation of the treatment result was done with the aid of the patients’ records, plaster models of the jaws and standardized extra- and intraoral photographs. The plaster models were measured by two assessors who were calibrated. The assessors measured five models each, and then compared and discussed the values to reach an agreement. All models were then measured in the same way, and if discrepancies occurred, the measurements were made again, together. Data from baseline, after 3, 6, 9 and 12 months (T1-T4) was analyzed. All data collected has been kept anonymous and confidential. Only the personnel involved has
treatment were registered. These measurements were divided into three-month periods and a mean value was calculated for each period. The mean value for each group was then
calculated. In cases with more than 10 days of loss of data during a three-month period, the weakest value of the group was used for the missing period.
Ethical approval
The project was approved by the Ethical Committee in Uppsala [Dnr 2014-196]. Information about this was given both verbally and in written form to the patients and their parents.
Clinical importance of the study
The aim of the treatment is that the patient should receive a complete lip closure, that the overjet is corrected and that the sagittal relationship is neutral. Outcome measure will be related to time of use, which has been registered by the incorporated sensor, TheraMon®. Results from the study will indicate if a nightly use, eight hours, of a van Beek-activator is sufficient to achieve a satisfactory treatment result. A shorter usage time will hopefully lead to increased adherence which in turn leads to a higher success rate of the treatment.
RESULTS
Participation
A total of 26 patients accepted participation in the study, and 6 patients discontinued their participation for various reasons. Data from 20 patients has been collected in the study, 8 patients in the 8-hour group and 12 patients in the 12-hour group (Figure 5). From 19 patients there is data from the first 12 months of treatment, and from one patient there is only data from the first 6 months.
Figure 5. Flowchart of participation
Fig 5. Flowchart of the sample between May 2015 and May 2019
*One patient obtained an adequate treatment result after only x months. Therefore, this patient could not
Demographics at baseline
No significant difference was observed between the two study groups regarding gender, age, overjet and overbite. The mean age in the 8-hour group was 10.2, and in the 12-hour group it was 9.9. In the 12-hour group there were an equal number of girls and boys, and in the 8-hour group there were two fewer girls than boys, but this was not considered significant (Table 2).
Table 2. Demographics in age and gender at the start of treatment
8h 12h Total Participants (n) 8 12 20
Gender (n) ♀ 3 ♂ 5 ♀ 6 ♂ 6 20
Mean age (years) 10.2 9.9 10.0
SD 0.6 0.9 0.8
min 9.6 8.1 8.1
max 11.1 11.2 11.2
SD: standard deviation, min: age of youngest participant, max: age of oldest participant
Loss of data
Data from every patient has been downloaded in four different periods (3, 6, 9, 12 months). In the 8-hour group, three patients had four complete periods. Of the total 32 periods, 7 of these periods had data loss of more than 10 days. In these cases, the weakest value of the period in question, has been used. In the 12-hour group there were 48 periods in total, and in 22 of these periods there was a data loss of more than 10 days. For two of these patients, there is not a single complete period, and in these cases the weakest values have been used in all of their periods. Only two patients in the 12-hour group had four complete periods.
Treatment results
In the beginning of the treatment, 14 out of 20 patients had an incomplete lip closure, five of them were in the 8-hour group, and nine of them were in the 12-hour group. 18 patients had a deep bite, whereof 16 also had gingival impingement. All patients in the 12-hour group had a deep bite, and only two of them did not have gingival impingement in combination with the deep bite. After one year of treatment, none of the patients suffered from these conditions anymore. In the 8-hour group, the overjet had a mean reduction of 50%, and the overbite a mean reduction of 38%. In the 12-hour group, the equivalent values were 53% and 33%. See Table 3 for clinical measurements in both groups of overjet and overbite from baseline, 3, 6, 9 and 12 months. See Table 4 for study model measurements in both groups of overjet and overbite from baseline and after 12 months.
Table 3. Measurements, clinical T0 T1 T2 T3 T4 8h 12h 8h 12h 8h 12h 8h 12h 8h 12h Overjet (mm) mean 7.0 7.5 6.0 6.5 5.0 4.0 4.0 3.5 3.5 3.5 SD 1.9 1.9 2.5 1.5 2.5 1.6 1.9 1.5 1.5 1.3 min 5.0 5.0 2.5 4.5 2.5 2.0 2.0 1.5 2.0 1.5 max 11.0 12.0 10.0 8.5 9.0 7.0 8.0 6.0 6.5 5.5 Overbite (mm) mean 4.0 4.5 3.5 4.0 3.5 3.5 3.5 3.0 2.5 3.0 SD 2.7 1.0 2.5 1.0 1.3 1.2 1.1 1.3 1.1 1.3 min -2.0 3.0 -2.0 2.6 2.0 0.0 2.0 1.0 1.0 1.0 max 7.0 6.0 6.5 6.0 5.5 5.0 5.0 5.0 4.0 5.0
Table 4. Measurements, study models
T0 T4 8h 12h 8h 12h Overjet (mm) mean 7.0 7.5 4.5 3.5 SD 2.7 1.3 2.3 1.3 min 4.0 4.5 2.5 2.0 max 12.0 9.0 7.5 6.0 Overbite (mm) mean 3.5 4.5 3.1 3.0 SD 1.8 0.6 1.4 0.8 min -1.0 3.0 1.0 1.5 max 4.0 5.0 4.0 4.0
Wear-time and adherence
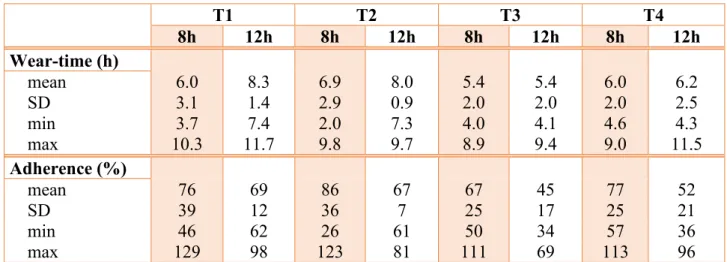
In the 8-hour group, five patients used the appliance for 8 hours or more during at least one period. In the 12-hour group, no patients achieved a 12-hour usage, but 8 patients used the appliance for 8 hours or more during at least one period. In other words, the percentage of patients who used the appliance for at least 8 hours, was practically the same in both groups (62% in the 8-hour group, 66% in the 12-hour group). In both groups, there was a better adherence during the first six months of the treatment. Between T2 and T3 there was a radical reduction in level of adherence, but between T3 and T4 an increase in adherence could be observed. 50% of the patients in both groups, managed to achieve at least 8 hours wear-time during the second period (Table 5). In the 8-hour group, the girls had a total mean adherence of 78% and the boys 75%. In the 12-hour group, both the girls and the boys had a total mean adherence of 58%.
Table 5. Wear-time and adherence T1 T2 T3 T4 8h 12h 8h 12h 8h 12h 8h 12h Wear-time (h) mean 6.0 8.3 6.9 8.0 5.4 5.4 6.0 6.2 SD 3.1 1.4 2.9 0.9 2.0 2.0 2.0 2.5 min 3.7 7.4 2.0 7.3 4.0 4.1 4.6 4.3 max 10.3 11.7 9.8 9.7 8.9 9.4 9.0 11.5 Adherence (%) mean 76 69 86 67 67 45 77 52 SD 39 12 36 7 25 17 25 21 min 46 62 26 61 50 34 57 36 max 129 98 123 81 111 69 113 96
DISCUSSION
In both groups, a reduction of both overjet and overbite was observed. There was no significant difference between the 8- and 12-hour group for overjet and overbite reduction. The adherence, on the other hand, was better in the 8-hour group during the whole 12-month period.
Wear-time and adherence
The adherence in the 8-hour group was slightly higher than in the 12-hour group. More than half of the patients in the 8-hour group achieved at least 8 hours wear-time during at least one three-month period. In the 12-hour group, none of the patients reached the prescribed wear-time of 12 hours. Noticeably, it was more challenging to use the appliance for 12 hours, i.e. evening and night wear, compared to the shorter time, 8 hours, i.e. only night wear.
The age of a child often determines the bedtime and subsequently how many hours of sleep the child acquires. The younger the child, the earlier the bedtime and thus the more hours of sleep. According to Garmy et al, the median sleeping time for ten-year-old children is 9,5 hours on weeknights (38). This could be an explanation for why an 8-hour wear-time prescription seems to be less difficult to reach than a 12-hour wear-time. Moreover, many children participate in extracurricular activities after school hours. According to a German study from 2016, 76% of boys and 59% of girls aged 7-14, participated in a sports club, and almost 50% of the children attended some type of extracurricular activity 1-2 times a week (39). If a child engages in extracurricular activities in the afternoons or evenings, there is not much time left between dinner and bedtime to wear an appliance. This could provide an additional explanation why it is difficult to attain a longer wear-time prescription.
It is arguable whether the patients in the 8-hour group were affected by positive affirmations from the dentists and/or students when reaching a wear-time of 8 hours, while the patients in the 12-hour group might have been told that they could do better, even if they reached more than 8 hours. Validation and a positive attitude could be important to get a better adherence from the patient. It is possible that a patient who does not get enough endorsement, simply
activities, personal preferences, opinions regarding the treatment results in personal variations requiring individualizing of the wear-time. If the orthodontist was able to customize the treatment after an analysis of the expected adherence, this would lead to less frustration, shorter treatment periods and lower costs. It is essential to include the patients from the beginning and to involve them in the design of the treatment plan. By doing so, the adherence will increase (27). Which can be observed in Table 5, the adherence clearly decreases in the third period, T3, between 6-9 months, to later increase again in T4, between 9-12 months. Possible explanations for this could be that the patients were affected by the Hawthorne effect during the first six months of the study, to later on forget about the monitoring and use the appliance less and less. At the appointment, during the third period, the reading presumably led to negative feedback and information about that the wear-time needs to increase. This could explain the slight increase seen in T4. Another explanation could be that a vacation or change of routine appears during this period, whereupon the appliance often is left unworn. Regardless of the possible reasons for a decreased wear-time, an incorporated TheraMon sensor is a simple and cost-effective aid for the dentist to better gain understanding about the patients’ usage.
Wear-time related to gender and age
Previous studies have observed a higher level of adherence in younger children, and also a higher level of adherence in girls compared to boys (23,30). However, these statements have not been proved in the present study, since no significant differences in adherence could be observed. As mentioned earlier, in cases with data loss of more than 10 days in a three-month period, the weakest value in each group, regardless of gender, was given to these patients. Subsequently, the wear-times of the boys and girls could be misleading if the weakest value in a group was a boy’s and given to a girl with data loss, and vice versa. Nevertheless, the
present study included too few subjects to be able to draw any conclusions about neither gender nor age.
Ethical considerations
One may say that the constant monitoring of wear-time is an ethical dilemma that should be taken into consideration. The sensor is activated and registered in the patient’s name where every hour of wear-time can be analyzed. The sensor is read at every appointment, since it is not able to store data for more than 100 days. Therefore, it is required to connect the sensor to the patient's name and thereby not possible to keep the data anonymous throughout the
treatment period. It could be intimidating for the patient to be observed by an authority, and it might feel even worse before getting feedback on the wear-time if the patient knows that the prescribed wear-time has not been achieved. However, both patients and their parents were thoroughly informed about the sensor and how it works, and the purpose of monitoring the wear-time.
Strengths and limitations
One of the greatest strengths of the study is that it is a randomized controlled trial (RCT). RCTs are considered to give the highest level of evidence when evaluating effectiveness. The randomization of patients was done by a computer program and this minimizes the risk of bias. Moreover, an important strength of the study is its ability to generate the actual wear-time with the aid of TheraMon® microsensors. The Hawthorne effect was reduced because of a follow-up period of more than six months, which also generates a more reliable result (34,35).
It is important to take into consideration that this study has been performed at a Dental school clinic with multiple treaters, both dentists and students. The information that is given to the patient and parents, might differ from appointment to appointment. According to the patients’ medical records, the wear-time has sometimes been discussed with the patient, but sometimes the sensor has been read without updating the patient, perhaps due to shortage of time.
Additionally, only a few people at the clinic were qualified to operate the TheraMon® reading station and even fewer knew how to analyze the data. Moreover, some treaters might have taken the time to motivate the patient, while others did not. The results would have been more reliable if all of the appointments were performed by the same treater, with a standardized protocol. On the other hand, only one treater involved in the project could lead to a higher risk of bias due to trying to direct the result in one way, consciously or not.
When comparing the clinical measurements with the model measurements, divergences of up to 4 mm where encountered. As can be observed in table 3 and 4, the clinical and model mean overjet are the same, but the individual measurements differ. In a study by Jiménes-Gayosso et al, manual and digital measurements of overjet and overbite were compared, on 30 models. No statistically significant differences between the mean measurements were found, even though individual differences were encountered. In other words, despite individual variations between measurements, the mean values were not affected (40). However, the mentioned study, and the present study, both might be considered limited in size and thereby not completely reliable. Unfortunately, all models from after one year of treatment were not finished before the end of this trial, which means that the mean value of the model
measurements were calculated from 4/7 patients in the 8-hour group, and 8/12 patients in the 12-hour group. Therefore, one cannot be certain that the mean model values would have been the same if all the models of the patients were measured after one year.
The study model measurements were performed by two assessors who had been calibrated. However, some models were difficult to measure for reasons such as poorly made indexes and difficulties finding a stable occlusion. Correctly taken impressions and indexes are required for adequate models, and naturally there is no guarantee that the models were made correctly. The clinical measurements were performed by multiple students and/or dentists, and therefore might not be completely accurate. Difficulties may arise when measuring the overjet and overbite in a child, and it is important to supervise the child so that the occlusion is correct during the measurements.
Even though the use of microsensors for measuring wear-time is helpful, technical difficulties are quite common. A number of sensors stopped working or ran out of battery during the treatment, which resulted in the loss of data for several patients. In the 8-hour group a total of 3 periods were lost, and in the 12-hour group a total of 16 periods were lost due to these technical difficulties. As a result of personnel who were not informed about how the TheraMon® program worked, 3 sensors in each group were not activated at the start of the treatment. Additionally, over 20% of the patients who agreed to participate in the study initially, dropped out before the first year of treatment was done, which naturally aggravated the trial.
Suggestions for future studies
To be able to draw any conclusions about wear-time related to gender, age, and other factors, a larger study group is required. Furthermore, to reduce the possibility of misunderstandings, it is desirable that all people involved in executing the treatments are well informed about the study design.
Conclusions
- The level of adherence is higher during the first 6 months of a treatment and is then reduced between 6-12 months.
- A wear-time prescription of 8 hours per day displayed a higher level of adherence than 12 hours in the present trial.
- No clinically significant difference in treatment effect was detected between an 8-hour and 12-hour wear-time prescription.
- Considering the results of the present study, it is possible to recommend an 8-hour wear-time for patients who are to receive orthodontic treatment with a van Beek activator.
- Using a microsensor can help both the patient and the dentist to raise awareness of possible lack of success in the treatment, and thereby provide motivation or modify the treatment. The sensor could either be incorporated from start or as an addition in cases of treatment failure.
REFERENCES
1. Thilander B, Bjerklin E, Bondemark L. Essential Orthodontics. 1st ed. Chichester, West Sussex: Wiley Blackwell; 2018.
2. Proffit WR, Fields HW, Sarver DM. Contemporary Orthodontics. 5th ed. St. Louis, Missouri: Elsevier, Mosby; 2013.
3. Koch G, Poulsen S, Espelid I, Haubek D. Pediatric Dentistry A Clinical Approach. 3rd ed. Chichester, West Sussex: Wiley Blackwell; 2017.
4. Jyoti S, Pavanlakshmi G. Nutritive And Non-Nutritive Sucking Habits Effect On The Developing Oro-Facial Complex; A Review. Dentistry 2014; 4: 1–4.
5. Kallunki J, Bondemark L, Paulsson L. Outcomes of Early Class II Malocclusion Treatment - A Systematic Review. Dent Oral Heal Cosmesis 2018; 3: 1–7. 6. Ferreira JTL, Lima M do RF, Pizzolato LZ. Relation between Angle Class II
malocclusion and deleterious oral habits. Dental Press J Orthod 2012; 17: 111–7. 7. van Beek H. Overjet correction by a combined headgear and activator. Eur J Orthod
1982; 4: 279–90.
8. Kjellberg H, Fasth A, Kiliaridis S, Wenneberg B, Thilander B. Craniofacial structure in children with juvenile chronic arthritis (JCA) compared with healthy children with ideal or postnormal occlusion. Am J Orthod Dentofac Orthop 1995; 107: 67–78. 9. Machado S-C-S, Manzanares-Céspedes M-C, Ferreira-Moreira J, Ferreira-Pacheco J-J,
Rompante P-A-M-A, Ustrell-Torrent J-M. A sample of non-nutritive sucking habits (pacifier and digit) in portuguese children and its relation with the molar classes of angle. J Clin Exp Dent 2018; 10: e1161–6.
10. Kallunki J, Sollenius O, Paulsson L, Petrén S, Dimberg L, Bondemark L. Oral health-related quality of life among children with excessive overjet or unilateral posterior crossbite with functional shift compared to children with no or mild orthodontic treatment need. Eur J Orthod 2019; 41: 111–6.
11. Holm A-K, Axelsson S, Bondemark L, Brattström V, Hansen K, Lars-Åke M, et al. SBU • Statens beredning för medicinsk utvärdering The Swedish Council on Technology Assessment in Health Care. 2004.
12. Thiruvenkatachari B, Harrison JE, Worthington H V, O’Brien KD. Orthodontic
treatment for prominent upper front teeth (Class II malocclusion) in children. Cochrane Database Syst Rev 2013; 1–64.
13. WHO. Oral health [Internet]. 2018 [cited 2019 Oct 18]. Available from: https://www.who.int/news-room/fact-sheets/detail/oral-health
14. Dimberg L, Arnrup K, Bondemark L. The impact of malocclusion on the quality of life among children and adolescents: a systematic review of quantitative studies. Eur J Orthod 2015; 37: 238–47.
15. Gatto RCJ, Garbin AJÍ, Corrente JE, Garbin CAS. The relationship between oral health-related quality of life, the need for orthodontic treatment and bullying, among Brazilian teenagers. Dental Press J Orthod 2019; 24: 73–80.
16. Brierley CA, DiBiase A, Sandler PJ. Early Class II treatment. Aust Dent J 2017; 62: 4– 10.
17. Perinetti G, Primožič J, Franchi L, Contardo L. Treatment Effects of Removable Functional Appliances in Pre-Pubertal and Pubertal Class II Patients: A Systematic Review and Meta-Analysis of Controlled Studies. PLoS One 2015; 10: e0141198. 18. Altenburger E, Ingervall B. The initial effects of the treatment of Class II, division 1
malocclusions with the van Beek activator compared with the effects of the Herren activator and an activator-headgear combination. Eur J Orthod 1998; 20: 389–97. 19. Al-Kurwi ASA, Bos A, Kuitert RB. Overjet reduction in relation to wear time with the
van Beek activator combined with a microsensor. Am J Orthod Dentofac Orthop 2017; 151: 277–83.
20. Rizell S, Svensson B, Tengström C, Kjellberg H. Functional appliance treatment outcome and need for additional orthodontic treatment with fixed appliance. Swed Dent J 2006; 30: 61–8.
21. Hall JE. Guyton and Hall Textbook of Medical Physiology. 13th ed. Vol. 53. Philadelphia: W B Saunders Co Ltd; 2013.
22. Wang S, Ye L, Li M, Zhan H, Ye R, Li Y, et al. Effects of growth hormone and functional appliance on mandibular growth in an adolescent rat model. Angle Orthod 2018; 88: 624–31.
23. Arreghini A, Trigila S, Lombardo L, Siciliani G. Objective assessment of compliance with intra- and extraoral removable appliances. Angle Orthod 2017; 87: 88–95. 24. TheraMon® [Internet]. [cited 2019 Apr 1]. Available from:
https://www.thera-mon.com
25. Tsomos G, Ludwig B, Grossen J, Pazera P, Gkantidis N. Objective assessment of patient compliance with removable orthodontic appliances: A cross-sectional cohort study. Angle Orthod 2014; 84: 56–61.
26. Schott TC, Ludwig B. Microelectronic wear-time documentation of removable
orthodontic devices detects heterogeneous wear behavior and individualizes treatment planning. Am J Orthod Dentofac Orthop 2014; 146: 155–60.
27. Schäfer K, Ludwig B, Meyer-Gutknecht H, Schott TC. Quantifying patient adherence during active orthodontic treatment with removable appliances using microelectronic wear-time documentation. Eur J Orthod 2015; 37: 73–80.
28. Aronson JK. Compliance, concordance, adherence. Br J Clin Pharmacol 2007; 63: 383–4.
29. Chakrabarti S. What’s in a name? Compliance, adherence and concordance in chronic psychiatric disorders. World J Psychiatry 2014; 4: 30.
30. Al-Moghrabi D, Salazar FC, Pandis N, Fleming PS. Compliance with removable orthodontic appliances and adjuncts: A systematic review and meta-analysis. Am J Orthod Dentofac Orthop 2017; 152: 17–32.
31. Richter DD, Nanda RS, Sinha PK, Smith DW. Effect of behavior modification on patient compliance in orthodontics. Angle Orthod 1998; 68: 123–32.
32. Grady KE, Goodenow C, Borkin JR. The effect of reward on compliance with breast self-examination. J Behav Med 1988; 11: 43–57.
33. Ackerman MB, McRae MS, Longley WH. Microsensor technology to help monitor removable appliance wear. Am J Orthod Dentofac Orthop 2009; 135: 549–51.
34. Abdulraheem S, Bondemark L. Hawthorne effect reporting in orthodontic randomized controlled trials: truth or myth? Blessing or curse? Eur J Orthod 2018; 40: 475–9. 35. McCambridge J, Kypri K, Elbourne D. In randomization we trust? There are
overlooked problems in experimenting with people in behavioral intervention trials. J Clin Epidemiol 2014; 67: 247–53.
36. McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: New concepts are needed to study research participation effects. J Clin Epidemiol 2014; 67: 267–77.
37. Scaglia P, Zimdahl M. Treatment effects of van Beek activator comparing two wear-time prescriptions assessed by microsensors : a randomized clinical trial. [master’s thesis Internet] Malmö Malmö Univ 2019 [cited 2020 Feb 10] Available from https//muep.mau.se/handle/2043/29717.
38. Garmy P, Nyberg P, Jakobsson U. Sleep and Television and Computer Habits of Swedish School-Age Children. J Sch Nurs 2012; 28: 469–76.
39. Felfe C, Lechner M, Steinmayr A. Sports and Child Development. PLoS One 2016; 11: e0151729.
40. Jiménez-Gayosso SI, Lara-Carrillo E, López-González S, Medina-Solís CE, Scougall-Vilchis RJ, Hernández-Martínez CT, et al. Difference between manual and digital measurements of dental arches of orthodontic patients. Med (United States) 2018; 97: