Elsevier Editorial System(tm) for Australasian Emergency Nursing Journal Manuscript Draft
Manuscript Number: AENJ-D-11-00034R2
Title: Emergency nurses working with Manchester Triage - The impact of nursing experience on patient safety
Article Type: Original Research papers
Keywords: Triage, experience, patient safety, nursing, Sweden. Corresponding Author: Dr. Eric Dan Carlström, Ph.D.
Corresponding Author's Institution: Helath management First Author: Berit Forsman, BSC RN
Order of Authors: Berit Forsman, BSC RN; Susanne Forsgren, BSC RN; Eric Dan Carlström, Ph.D.
Abstract: Background: The article describes triage nurses perception of the impact experience and MTS have on patient safety during MTS triage assessment at emergency departments in Western Sweden. Methods: Data was collected from 74 triage nurses using a questionnaire containing 37 short form questions of Likert type, analyzed descriptively and measured the covariance. Data was also collected with two open questions by using the critical incident technique and content analysis.
Results: The results described that the combination of the MTS method, the nurses' experience and organizational factors accounted for 65% of patient safety. The study indicated that nurses' experience contributed to higher patient safety than the model itself. A standardized assessment model, like MTS, can rarely capture all possible symptoms, as it will always be constrained by a limited number of keywords and taxonomies. It cannot completely replace the skills an experienced nurse develops over many years in the profession.
Conclusions: The present study highlights the value of triage nurse's experience. The participants considered experience to contribute to patient safety in emergency departments. A standardized triage model should be considered as additional support to the skills an experienced nurse develops.
Suggested Reviewers: Opposed Reviewers:
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
Gothenburg, Sweden 17/1/2012
Australasian emergency nursing journal
Dear Editor
Attached please find a new version of our manuscript for publication in the
Australasian emergency nursing journal. This article focuses on triage assessment in
emergency departments in Western Sweden. The findings in the article indicated that
nurse´s experience contribute to higher patient security than the triage model itself.
Because of its empirical content and development of theory the article is interesting
for both researchers and practitioners. We are sending this article to Australasian
emergency nursing journal as the subject of triage assessment has been dealt with in
the journal previously.
This article has neither been published nor considered for publication in any other
journal.
Yours Sincerely,
Eric Carlström
Berit Forsman
Susanne Forsgren
Contact information:
Eric Carlström
Associate Professor
The Sahlgrenska Academy
University of Gothenburg
and University West, Trollhättan.
Adress: Department of Nursing, Health and Culture.
University West,
SE-461 86 Trollhättan, Sweden,
eric.carlstrom@hv.se
Tel. +46702738126
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
Nurses working with Manchester Triage
- The impact of experience on patient security
Berit Forsman, BSc, RN Susanne Forsgren, BSc, RN
Eric D. Carlström, PhD, MA, RN1
Susanne Forsgren, is a Lecturer in Emergency Nursing, Department of Nursing, Health and Culture, University West, Trollhättan, Sweden.
Berit Forsman, is a Lecturer in Emergency Nursing, Department of Nursing, Health and Culture, University West, Trollhättan, Sweden.
Eric Carlström is an Associate Professor and Director of Research in Health Management, Policy and Economics, Department of Nursing, Health and Culture, University West, Trollhättan, Sweden.
Keywords: Triage, experience, patient security, nursing, Sweden.
SF, BF and EC conceived and designed the study. SF and BF developed the study protocol. EC, SF and BF designed and tested the study instruments. EC supervised data collection. SF and BF analysed the data. BF, SF and EC prepared and approved the manuscript.
1 Corresponding author: Eric D. Carlström, Department of Nursing, Health and Culture. University West, SE-461 86 Trollhättan, Sweden, E-mail eric.carlstrom@hv.se Tel. +46702738126
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 Competing interests
There are neither competing interests nor conflicts of interest. *Provenance and Conflicts of Interest
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 Funding
No founding or research grants were provided. *Funding
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
Australiasian emergency nursing journal
(
AENJ) editors and reviewer’s
comments and answers
Title: Emergency nurses working with Manchester Triage - The impact of nursing experience
on patient safety (Ms. Ref. No.: AENJ-D-11-00034).
Dear Editors and anonymous reviewers. We, once again, really appreciate all detailed
comments to the paper.
Below you will find our response to the reviewer’s comments. The revised parts are marked
yellow in the paper.
Thank you for your patience still considering our work
Sincerely
The authors
Editors:
1.We hope to receive a revised manuscript from you by Jan 26,2012 if possible.
We will submit before Jan 26, 2012
2.Please review comments from the reviewer 3 listed below, in particular the issues
Please see below
Reviewer 3
1.Whilst experience is important, one of the flaws of reliance on experience alone or as a
supplement to a objective system is that is it not reproducible between individuals. Experience
can also have a negative effect if there has been no follow through or learning/reflection after
an event. This should be made clear.
Please see line 255. Text has been rewritten and marked yellow
2.What you describe is piloting rather than validation but it provides more detail.
Line 133, the word is changed to piloting
3.I am still not convinced of the need for a formal statistical calculation because you are not
seeking causality and you cannot generalize from the sample selected.
The formal statistical calculation was a part of the methodological proceeding. We have
however tuned down the causality and generalizability of the results somewhat under the
subheading, limitations. Please see new text line 318-322, marked yellow.
4.You state that triage is not a predictive tool-triage is a process of assessment, a tool such as
the MTS may be used to help identify priority. The process is not predictive. MTS or other
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
such tools are not designed to replace experience they are there to augement and support
decision making. This can be particularly useful with staff of less experience . However
experience does not always protect against poor judgement.
Please see line 247-249 and 255-256, Sentences changed and marked yellow.
5.The word commence is incorrect. I think you mean initial
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
Emergency nurses working with Manchester Triage
1
- The impact of nursing experience on patient safety
2
3
Abstract:
4
5
Background: The article describes triage nurses perception of the impact experience and MTS have on patient safety during MTS triage
6
assessment at emergency departments in Western Sweden.
7
Methods: Data was collected from 74 triage nurses using a questionnaire containing 37 short form questions of Likert type, analyzed
8
descriptively and measured the covariance. Data was also collected with two open questions by using the critical incident technique and
9
content analysis.
10
Results: The results described that the combination of the MTS method, the nurses’ experience and organizational factors accounted for 65%
11
of patient safety. The study indicated that nurses’ experience contributed to higher patient safety than the model itself. A standardized
12
assessment model, like MTS, can rarely capture all possible symptoms, as it will always be constrained by a limited number of keywords and
13
taxonomies. It cannot completely replace the skills an experienced nurse develops over many years in the profession.
14
Conclusions:The present study highlights the value of triage nurse’s experience. The participants considered experience to contribute to
15
patient safety in emergency departments. A standardized triage model should be considered as additional support to the skills an experienced
16
nurse develops.
17
18
Keywords: Triage, experience, patient safety, nursing, Sweden.
19
20
What is known about the topic?
21
In previous studies, the need for theoretical triage assessment training is regarded as central to improve patient safety. Alternative forms
22
of training such as practical case exercises can further increase the ability to identify severely ill patients. Nurse´s experience has been shown
23
to improve decision ability, but there is no evidence that triage nurse experience improves decision accuracy in computer based triage cases.
24
25
What this paper adds or contributes?
26
This study highlights the value of experience. Experience contributes to more patient safety than the studied triage model itself.
27
Extensive experience is established over years of assessing severely ill patients. When triage assessment models are used it should be by
28
experienced nurses, skilled in interviewing techniques and clinical diagnosis.
29
Introduction
30
There is an ongoing debate in Sweden about the extent to which the practice of triage contributes to
31
patient´s safety. The debate is based on notification to the Swedish National Social Board where a
32
patient was left in a waiting room with a life threatening condition. Although the triage category was
33
correct according to the decision tool used, the patient's urgent condition wasn’t identified. The
34
criticism outlined was that in situations where assessment models are used, they might strongly
35
influence priority to a greater degree than the triage nurse's experience. 1 When a triage assessment is
36
not consistent with the triage nurse's perception; based on experience, the corresponding model tends
37
to be assigned first priority. If this is the case, the assessment model could be a hindrance and become
38
a real risk to the patient.1, 2, 3The present study describes 74 nurse´s perception of the impact
39
experience and Manchester triage system (MTS) have onpatient safety. Patient safety is defined as to;
40
minimize the risk of patient´s complications or early death as well as to identify the need for hospital
41
care. 4
42
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 Triage models
43
The workload of emergency departments varies according to the number and acuity of the patients.
44
5, 6
An efficient triage system regulate the length of the patients’ waiting times in the emergency
45
department by combining immediate assessments and interventions. 5 In order to properly assess the
46
care patient´s need, triage nurses must understand, identify and evaluate available information from
47
the patient. Triage is intended to ensure that patients are taken care of according to the urgency of the
48
clinical needs rather than the order in which they arrive. 5, 6
49
Modern emergency department triage was developed in Australia, United Kingdom, Canada and
50
USA.7 National Triage Scale (NTS) is a five- point triage scale adopted in Australia 1993/94. The
51
British and Canadian scales are based on this system. The NTS scale was revised in 2000/01 to include
52
the patients’ vital signs and symptoms, and was also renamed Australian Triage Scale (ATS). 8 The
53
need for a triage scale in Canada was described in the early 1970’s, but the scale did not become a
54
reality until the 1990’s, when The Canadian Emergency Department Triage (CTAS) was introduced.
55
CTAS is a scale based solely on the vital signs.9 The Manchester Triage System (MTS) was
56
introduced in the UK in 1996.6 US hospitals currently use a variety of triage scales, the most widely
57
used and dispersed triage system is a scale called Emergency Service Index (ESI). 10 The Cape Triage
58
Score (CTS) was introduced in 2004 in South Africa. It is a scale appropriate for specific problems,
59
which include a large number of people with HIV infections and severe trauma cases.11
60
In Sweden registered nurses work with triage assessment and there is no standard triage available.
61
Currently three different methods are of use; Adaptive Triage (ADAPT), Medical Emergency Triage
62
and Treatment Systems (METTS), and the Manchester Triage System (MTS). ADAPT and METTS
63
are based on subjective parameters combined with vital parameters such as respiratory rate, oxygen
64
saturation in blood, level of consciousness and pulse rate. 4 12
65
MTS has a five-level scale; immediate care, very urgent, urgent, and two levels of not urgent. The
66
highest category level means that gravely ill patients with a life-threatening condition is assigned red
67
and is given immediate care. Patients with very urgent conditions such as ongoing chest pain is
68
assigned category orange and is given care within ten minutes. Urgent cases are assigned category
69
yellow and can wait up to one hour, less urgent patients are assigned category green and can expect a
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
waiting time of up to three hours. Other patients are given a blue triage level. They can wait for four
71
hours. They can also be advised to visit a primary care medical clinic. 6
72
The first step in MTS assessments is when the nurse, responsible for triage chooses a flow chart
73
based on the patient’s reason for contacting the emergency department for example “chest pain”. The
74
chart begins by identifying possible criteria indicating life-threatening conditions for the patient, such
75
as affected breathing, blood pressure or pulse. If none of these conditions exist, the nurse continues
76
along the flow chart asking questions such as; do you have a problem breathing, dyspnea? If the
77
patient describes “pain correlated to breathing” the nurse assigns the patient a yellow category. MTS is
78
considered a sensitive instrument that identifies severely ill patients in need of intensive care.13 90% of
79
the nurse´s assigned patients to exactly the same triage categories in a study using fictive scenarios and
80
MTS. 14
81
Triage and nurses’ experience
82
83
Experience is considered to be an important part of nursing skills.15 In the present study the
84
definition of an experienced nurse, is a nurse who have acquired assessment skills that recognize
85
symptoms and relate symptoms to known disease categories.21 Skills are not based on education alone,
86
the transition into a skilled nurse requires experience that can be acquired during clinical work. 5, 16, 17,
87
18
Triage requires an ability to make independent decisions and a triage nurse is considered to be able
88
to establish trust and confidence with the patient. 19, 20 Dialogue improve trust and confidence between
89
nurse and patient and helps the nurse to collect data about the patient's condition.5
90
91
The ideal triage system should quickly and accurately distinguish patients in need for immediate
92
care and patients able to wait for treatment. 6, 22, 23 Triage scales and assessment levels must be absolute
93
comprehensible.24, 25 Sometimes the MTS model is not sufficient; the nurse has difficulties finding
94
matching keywords to the patient’s subjective parameters or symptoms, which might complicate the
95
assessment. 26
96
If the patient is assigned a lower triage priority than required the patient’s health may be
97
jeopardized, however, an over-triage can contribute to a less than optimal use of the emergency
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 department’s resources.24, 27
The triage nurses interview technique and the ability to make accurate
99
clinical observations contributes to patient safety.3 In order to reach an accurate priority quickly, the
100
length of the interview and added examinations must be limited. Time-consuming assessments are
101
balanced with the need to correctly identify a severely ill patient. A misjudgment can lead to unwanted
102
consequences due to incorrect triage category.23 Prioritizing requires a sufficient basis for evaluation,
103
the nurse must learn techniques to get the patient to focus on their symptoms and pass on relevant
104
information.28 A common cause of error is a conversation that is too superficial.28, 29
105
Experience has proven to contribute to accurate triage assessments 30. Nurses who regularly practice
106
triage, have proven to be those who make the best decisions.30 However, clinical experience do not
107
always make a significant difference.31 Risks may arise if a nurse generalizes his or her evaluation of
108
the patient's condition, comparing it with previous cases without considering alternative possibilities.
109
The nurse might make hasty assumption, “locks on the target” and acts within a limited set of data.
110
The potential risk of hasty assumptions underpins the need to meet every patient without bias. 32
111
Method
112
113
Questionnaires were sent to 102 triage nurses in four emergency departments in Western Sweden
114
working with MTS. All informants were registered nurses, working with MTS triage assessment only
115
during regular periods of their work schedule for at least six months. The supervisors at each
116
respective emergency department gave permission to approach staff to the research area.
117
The questionnaire design
118
119
A questionnaire was chosen as the best method for conducting the initial investigation to describe
120
the impact of emergency nurses' experience during MTS triage assessment on patient safety .The
121
instrument was designed by the authors to provide a possibility to answer the research question. The
122
survey included nurses basic demographic details; age, work experience, years working with triage
123
assessment, the education level and additional medicine courses. Other areas were job satisfaction
124
related to their nursing work at the ED, such as interesting and stimulating task, possibilities to take
125
initiative and to act independently.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
Questions about their job satisfaction related to their triage assessment task, such as additional
127
triage training, triage organization and attitudes to the MTS and patient safety. The questionnaire
128
contained 37 questions with five possible Likert type answers. 35 Data was also collected with two
129
open questions using the Critical Incident Technique (CI). The informants were asked to describe two
130
triage assessment scenarios in text - one which they thought was satisfactory and one which they
131
thought was unsatisfactory (see appendix).
132
The instrument was piloted by five nurses responsible for triage assessment at respective
133
emergency departments. The purpose was to test the questionnaire on a small group of volunteers, as
134
similar as possible to the target group.36,37 This led to small adjustments to clarify some of the
135
questions.
136
A power calculation was performed before the study. With a power of 75%, and given the number of
137
included predictors (i.e. an alpha value at 0.05) a total of 70 participants were needed to be included in
138
the study.33,34 The instrument’s internal reliability was tested by calculating Cronbach’s alpha. The
139
results varied between 0.68 and 0.84, which is considered to be variable but satisfactory3,40
140
39
Questionnaires were numbered and the variables were defined and fed into the computer program,
141
Statistical Package for the Social Sciences (SPSS) 14.0.34 Statistical Significance was established at p
142
< 0.05. The quantitative part of the analysis consisted of descriptive data, bivariate and multivariate
143
regressions. The CI was used to capture the informants’ views on the triage assessment. The technique
144
focuses on a factual incident, which may be defined as observable and integral episode of human
145
behavior. The incident must have had an impact on some outcome; it must have either a positive or
146
negative contribution to the accomplishment of some activity of interest.15, 42 The qualitative analysis
147
meant that the obvious part of the answers was extracted from each respective question. 43
148
149
Ethics
150
151
The study complied with ethical procedures according to Swedish law, 44 and the Declaration of
152
Helsinki.45 Participants fulfilling the inclusion criterions was included with the help from senior
153
managers and by the human resource departments. The questionnaire contained an introductory letter
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
where the background of the study was described. It contained detailed instructions and information
155
stating that participation was voluntary. Participants were informed that they were free to withdraw at
156
any time. They were assured of strict confidentiality and secure data storage. Swedish statutes do not
157
require ethics approval for research that does not involve a physical intrusion that affects the
158
participants.44159
Results160
161
The survey response rate was 75%. The age of the informants were evenly distributed between 25
162
and 64, most of the nurses (25%) was between 35- 44 years. Sixty three percent of the nurses who
163
participated in the study had more than five years’ nursing experience, and 70% had practiced MTS
164
for more than a year. Sixty two percent of the triage nurses had undergone a one-day MTS training
165
course. Thirty percent had studied trauma care at university level. Only one of the nurses had been to
166
university to specialize in triage.
167
When asked if their employers had offered them any on-the-job additional triage training besides
168
the MTS introduction over the past six months, 20% of the nurses answered yes. The additional
169
training included briefings about fictitious patient cases and different triage situations. Sixty one
170
percent expressed a need for initial and additional triage training. Of these 46% felt that they
171
specifically needed more training on simulated patient cases.
172
The questionnaire contained questions concerning the nurse´s personal attitudes, to experience,
173
reliability and patient safety regarding triage assessments using the MTS method. There were 70% of
174
the informants that felt the need for experience. Seventy-eight of the informants thought that MTS was
175
patient safe and 77% thought that it was a reliable method. Asked if the nurses were given sufficient
176
time for the triage assessment 90% of the nurses answered yes. Sixty one percent had sufficient time
177
for analysis and 66% gained support for the task and cooperation at the ED.
178
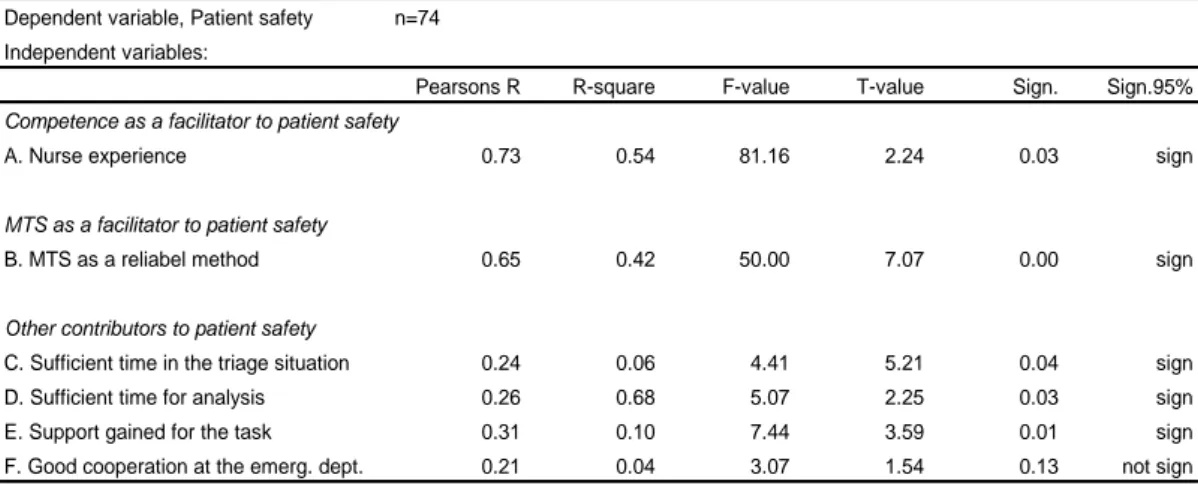
The relationship between the participant’s perception of the impact of MTS and nursing experience
179
on patient safety was tested in a number of bivariate regressions. The MTS triage model was
180
considered to contribute to patient safety (R = 0.65, R2 = 0.42). The triage nurse's skills as a result of
181
experience were however considered to be even more valuable. Experience was considered to improve
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
the patient’s safety (R = 0.73, R2 = 0.54). The patient safety was considered to increase the longer the
183
nurse had worked with triage (R = 0.33, R2 = 0.11).
184
Additional contributors to patient safety than nursing experience were found in the data. Patient
185
safety was considered to increase slightly when the nurse had enough time for assessment (R = 0.24,
186
R2 = 0.06) and enough time for subsequent analysis (R = 0.26, R2 = 0.68). If the organization offered
187
peer support to the triage nurse, patient safety was considered to increase even more (R = 0.31, R2 =
188
0.10) (tab:1).
189
Table 1: The importance of nurse´s experiences, MTS and other contributors as a determinant of patient safety,bivariate regression.
190
191
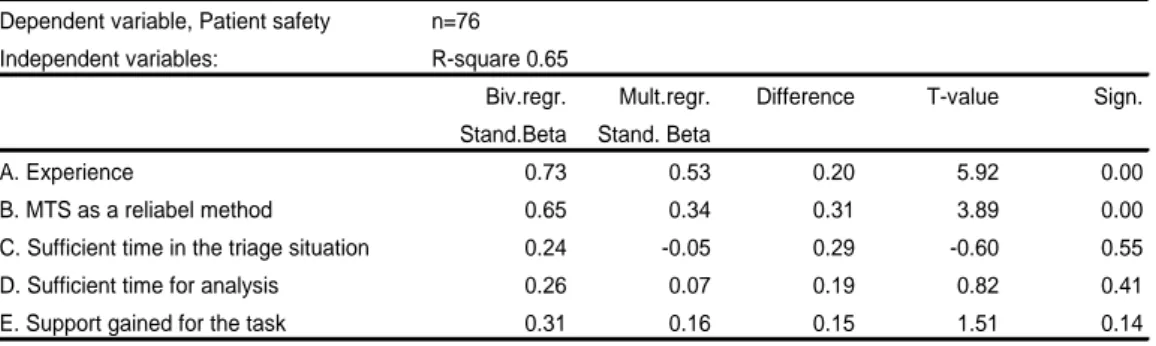
A multiple regression showed that nurses' skills, MTS as a method, and organizational factors
192
together accounted for 65% of patient safety (R2 = 0.65). This meant that 35% remained unexplained.
193
Two variables were still significant, nurse’s experience, and MTS as a method. The remaining
194
variables displayed low t-values, and were lacking significance on their own. The reason could be that
195
they co-variate or that they were present as an earlier link in connection to the cause. Results indicate
196
that experienced nurses combined with sufficient time for assessment and analysis while working with
197
MTS contributes to patient safety (tab.2).
198
Table 2: The importance of nurse´s experiences, MTS and other contributors as a determinant of patient safety,multiple regressions.
199
Table 1 Bivariate regression
Dependent variable, Patient safety n=74 Independent variables:
Pearsons R R-square F-value T-value Sign. Sign.95% Competence as a facilitator to patient safety
A. Nurse experience 0.73 0.54 81.16 2.24 0.03 sign
MTS as a facilitator to patient safety
B. MTS as a reliabel method 0.65 0.42 50.00 7.07 0.00 sign
Other contributors to patient safety
C. Sufficient time in the triage situation 0.24 0.06 4.41 5.21 0.04 sign D. Sufficient time for analysis 0.26 0.68 5.07 2.25 0.03 sign E. Support gained for the task 0.31 0.10 7.44 3.59 0.01 sign F. Good cooperation at the emerg. dept. 0.21 0.04 3.07 1.54 0.13 not sign
Table 2 Multiple regression
Dependent variable, Patient safety n=74 Independent variables: R-square 0.65
Biv.regr. Mult.regr. Difference T-value Sign. Stand.Beta Stand. Beta
A. Nurse experience 0.73 0.53 0.20 5.92 0.00
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
200
Open questions201
202
The results of the quantitative part of the study were confirmed by the answers to the open
203
questions in the survey. Fifteen of the nurses gave comments on the positive value of MTS. They
204
argued that the method contributed to patients being cared for safely. When the nurse and the patient
205
met, the conversation was normally held in an environment characterized by peace and quiet, where
206
the nurses' communication skills were used optimally. Patients were rapidly assessed, even if the
207
workload was high. One nurse also stated that the model contributed to early finding and identifying
208
patients with life-threatening conditions.
209
210
“During triage you can directly identify patients with severe symptoms. One can quickly bring
211
them into the emergency room and start the assessment.”
212
213
“A patient with minor subjective symptoms was examined in the emergency room but had a high
214
pulse rate. It did not seem so serious but MTS gave him a high priority and the patient was taken care
215
of faster than usual. It was fortunate because the patient had a ventricular fibrillation shortly
216
afterwards and his life was saved.”
217
218
“The patient had an undefined chest pain, which we thought was nothing serious, but it turned out
219
to be a heart attack. I am glad that such discomforts are given a high priority.”
220
221
There were also critical voices expressing that MTS was sometimes a hindrance to patient safety.
222
They could not find matching keywords or flow charts to substantiate their decisions. They regarded
223
the model as sometimes “ambiguous”, which could make it hard to identify serious conditions. One
224
nurse described an unsatisfactory triage assessment;
225
226
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
“A patient arrived suffering from mild abdominal pain. He had different blood pressures in his
227
arms. There was no keyword for this. The patient was given low priority because he had almost no
228
pain when arriving at the emergency room. Fifteen minutes after arrival the patient was dead. He died
229
of an aortic aneurysm, despite intensive CPR.”
230
231
Experienced nurses could sometimes have a “gut feeling” or intuition that something important had
232
been missed in the assessment. The MTS however, gave no scope of action for this. The model was
233
based on observations sorted under a limited number of headings. When the nurse’s perception did not
234
agree with the triage model they sometimes chose not to express their concerns. The nurses did not
235
want to appear to be unclear or vague in their assessment. However, in some cases the nurses assessed
236
according to their “gut feeling” in order to safely care for the patient
237
238
"When my intuition says that the patient should have a higher priority than MTS provides, it makes
239
me feel uncomfortable. It is a situation that is difficult to manage.”
240
241
“Sometimes, patients have many different symptoms. After a short conversation, I usually give a
242
higher priority to these patients, because I know they cannot manage to sit and wait for a long time in
243
the waiting room.”
244
Discussion
245
The informants in this study stated that a standardized assessment model, like MTS rarely captures
246
all possible symptoms. MTS as a tool will always be constrained by a limited number of keywords and
247
taxonomies. It may be used to help identify priority and give support in decision making, but it seems
248
unlikely to replace the skills an experienced nurse develops over many years in the profession.
249
Identifying pattern recognition, intuition and “gut feeling” is the hallmarks of nursing. Repeated
250
exposure to certain conditions gives nurses’ confidence in their abilities to recognize potential danger
251
areas.On the other hand, an experienced nurse sometimes has a tendency to associate the patient’s
252
needs to a simplified classical condition and hence determine a priority level too quickly. They could
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
thus rely on their experience and “lock on the target” by failing to carry out additional checks to
254
confirm the assessment. Experience can have a negative effect on nurse´s if there has been no follow
255
through or reflection after a serious event. It is important for nurses to question their experience and
256
meet each patient openly and unbiased.32 The nurses in present study reported while using MTS they
257
discovered subtle but serious symptoms that could otherwise have been missed. Both of these risks,
258
the limitation of MTS to identify serious conditions, as when a patient arrived suffering from mild but
259
lethal abdominal pain and on the other hand, nurses who performed the assessment too quickly and
260
assigned an incorrect priority – might be prevented by combining the model's benefits with an
261
experienced nurse's abilities (Fig. 1).
262
263
Fig.1264
265
266
267
268
269
270
271
Comments fig. 1.The figure shows three types of triage assessments based on the nurse's experience and MTS. A is representing a
272
combination of experience and MTS. In position A it is probable that the patient will be properly assessed. B is based on experience and C on
273
the model's keywords and taxonomies. Both B and C decrease the patient safety. At B, generalizations can be made. The nurses can rely in
274
their own experience and make a hasty prioritization, associating the patient’s condition with a classical condition. At C, the model leads to
275
problems in assessing patients correctly because of the lack of keywords. B can decrease the risk by using the work processes of the
276
standardized model, and the risk of C can be prevented by the nurse’s experience.
277
278
When excessive influence is given to MTS, the experienced nurses’ ability to convey a “gut
279
feeling” or intuition could be hampered. The “gut feeling” or intuition is a synthesis of all information
280
the nurses register implicitly. Such information is for example; a visual, auditory or a tactile
281
impression associated with previously experienced situations and events.46The nurses in this study
282
were not always able to describe the association, or put it into words at that moment, but the reaction
283
is still valid and the signals are often important to the triage assessment. This phenomenon has been
284
A
C
B
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
termed “tacit knowledge”, knowledge based on experience 46
which cannot be classified in an explicit
285
triage model. Nurses’ concerns that seem vague or evasive may contribute to key findings being
286
ignored. 41 If a standard triage model is given such a superior dominance that no objection can be
287
raised against its taxonomies, the nurse's experience will be neglected. Such a situation can reduce the
288
safety of the patient. The results of this study indicated that a nurse’s experience contributed to higher
289
patient safety than the model itself. This means that if the opportunity to object to the model is
290
reduced, patient safety will be significantly reduced. A triage model should therefore be considered as
291
additional support in order not to miss serious conditions. On the other hand, MTS contributed to
292
increased patient safety because the scheme reduced the risk of missing important parameters in the
293
assessment. The risk of the nurse missing serious conditions was reduced because the model forced the
294
nurse to ask key questions and make vital inquiries.
295
In previous studies regular training develops the triage nurses ability to identify the patient´s degree
296
of urgency and was regarded central to improve patient safety. 48 49, 50, 20, 32, 51, 52 Present study
297
highlights the value of experience. Although training is important, inexperienced nurses should not
298
perform triage assessments without appropriate supervision, even if they are well educated. 49
299
Experience is established through years of assessing severely ill patients. An alternative form of
300
training, which may contribute to acquiring experience, is practical case exercises, because this
301
training can increase the ability to identify severely ill patients. 53 When standardized assessment
302
models are used, they must be combined with skills in interviewing techniques and experience in
303
clinical diagnosis, which is acquired through hands-on exercises.23
304
Strengths and Limitations
305
306
This study highlights the value of experienced nurses performing triage. Experience seems to
307
contribute to more patient safety than the studied triage model itself. Extensive experience such as
308
interviewing techniques and clinical diagnosis is established over years of assessing severely ill
309
patients. It should also be possible to question the priority that a standardized triage model indicates.
310
The limitations in the present study include the fact that the findings may not be able to be
311
generalized to emergency departments outside Western Sweden. Although 74 nurses from four
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
suburban and urban emergency departments and trauma centers participated in the study, hospital
313
emergency departments from other parts of Sweden were not included. This study only describes
314
nurses working with MTS.
315
The fact that the study is based on a questionnaire measuring the perceived effects of experience
316
and MTS on patient safety can be considered as limitation. When analyzing results based on a
317
questionnaire a possibility of over- or underreporting cannot be ignored. In order to verify the
318
causality and generalizability of the results a study not just based on a questionnaire should be
319
performed. A study of the effects of experience versus triage models on the health status of patients
320
treated in emergency departments would give additional and important information.
321
A third limitation might be the fact that the informant´s descriptions of their critical incidents
322
related to the triage assessment are only short stories. A possibility to perform personal interviews 43
323
on the nurse´s perception of patient safety would have been valuable to the study.
324
325
In this study triage nurse’s experience proved to contribute to patient safety in emergency
326
departments. However, an experienced nurse might fail to notice important parameters through
over-327
reliance on his or her own reasoning. On the other hand, there is a risk that triage models may miss a
328
patient’s serious condition. Experience together with MTS minimizes the risk of patient´s
329
complications or early death as well as to identify the need for hospital care.4
330
Competing interests
331
332
There are neither competing interests nor conflicts of interest.
333
Funding
334
335
No founding or research grants were provided.
336
Acknowledgements
337
338
We would like to thank all of the emergency nurses who completed the survey.
339
340
341
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
References
342
343
1. Nyman U, Hellekant C. Har triagesköterskorna adekvat utbildning? Available at:
344
http://www.lakartidningen.se/includes/07printArticle.php?articleId=9845. Accessed June
345
12, 2011
346
2. Widgren BR, Örninge P, Grauman S, Thörn K. Akutvården säkrare och effektivare med
347
gemensamma metoder. Available at:
348
http://ltarkiv.lakartidningen.se/2009/temp/pda37415.pdf Accessed June 11, 2011
349
3. Forsgren S, Forsman B, Carlström E. Working with Manchester triage- job satisfaction in
350
Nursing. International Emergency Nursing 2009; 17: 226-32.
351
4. Swedish Council on Health Technology Assessment (SBU): Triage and flow charts.
352
Available at:
http://www.sbu.se/sv/Publicerat/Gul/Triage-och-flodesprocesser-pa-353
akutmottagningen/ Accessed March 23, 2011
354
5. Grossman VGA. Quick Reference to Triage. Philadelphia: Lippincott Williams & Wilkins;
355
2003.p.3-20.
356
6. Mackway- Jones K, Marsden J, Windle J. Emergency triage- Manchester Triage Group.
357
London: BMJ publishing group; 1997. p. 1-50.
358
7. Burr G, Fry M. Review of the Triage Literature: Past, Present, Future? Australian Emergency
359
Nursing Journal 2002; 5: 33-8.
360
8. Australian college for Emergency Medicine policy document. Emergency Medicine 2002; 14:
361
335-6.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
9. Murray M, Bullard M, Grafstein E. Revisions to the Canadian Emergency Department
363
Triage and Acuity Scale Implementations Guidelines. Canadian Journal of Emergency Medicine
364
2004; 6: 421-7.
365
10. Agency for Health care research and Quality. Emergency severity index version 4
366
implementation handbook. Available at: www.ahrg.gov/research/esi/esihandbk.pdf.
367
Accessed February 3, 2011
368
11.Wallis LA, Gottschalk SB, Wood D, Bruijns S, de Vries S, Balfour C. The Cape Triage Score
369
- a triage system for South Africa. South African Medical Journal 2006; 96: 53-6.
370
12. Olsson T, Terent A, Lind L. Rapid Emergency Medicine Score can predict long-term
371
mortality in nonsurgical emergency department patients. Academic Emergency Medicine 2004;
372
10: 1008-13.
373
13. Cooke MW, Jinks S. Does the Manchester triage system detect the critically ill? Journal of
374
Accident and Emergency Medicine 1999; 16: 179-81.
375
14. Versloot SM, Liutde J. The Agreement of the Manchester triage system and the
376
Emergency Severity Index in Terms of Agreement: A Comparison. Academic Emergency
377
Medicine 2007; 14: 57.
378
15. Sandberg J, Targama A. Ledning och förståelse: - ett kompetensperspektiv på
379
organisationer. Lund: Studentlitteratur; 1998. p. 73-5.
380
16. Chung J. An exploration of accident and emergency nurse experiences of triage decision
381
making in Hong Kong. Accident and Emergency Nursing 2005; 13: 206-13.
382
17. Ritchie J, Aldridge Crafter N, Little A. Triage Research in Australia: Guiding Education.
383
Australian Emergency Nursing Journal 2002; 5: 37-41.
384
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
18. Considine J, Hood K. A study of the effects of the appointment of a Clinical Nurse
385
Educator in one Victorian Emergency department. Accident and Emergency Nursing 2000; 8:
386
71-8.
387
19. Cone KJ, Murray R. Characteristics, Insights, Decision making, and Preparations of ED
388
Triage Nurses. Journal of Emergency Nursing 2002; 28: 401-6.
389
20. Göransson K, Ehrenberg A, Ehnfors M. Triage in emergency departments: national
390
survey. Journal of Clinical Nursing 2005; 14: 1067-74.
391
21. Benner P, Tanner C. How Expert Nurses Use Intuition. AJN-The American Journal of
392
Nursing 1987; 87: 23-34.
393
22. Öhlén G. Akutsjukvården kan få ett uppsving 2008. Läkartidningen. 2008; 4: 194-5.
394
23. Nyström M, Herlitz J. Möte mellan två kunskapsområden. In: Suserud BO, Svensson L,
395
editors. Prehospital akutsjukvård. Stockholm: Liber AB; 2009.p.13-21.
396
24. Fernandes C, Tanabe P, Gilboy N, McNair R, Rosenau A, Sawchuk P. et al: Five- level
397
triage: A Report from the ACEP/ENA Five-Level Triage Task Force. Journal of Emergency
398
Nursing 2005; 31: 339-50.
399
25.Travers D, Waller A, Bowling M, Flowers D, Tintinalli J, Hill C. Five- Level Triage System
400
More Effective Than Three- Level in Tertiary Emergency Departments. Journal of Emergency
401
Nursing 2002; 28: 395- 400.
402
26. Olofsson P, Gellerstedt M, Carlström E. Manchester Triage in Sweden-Interrater
403
reliability and accuracy. International Emergency Nursing 2009; 3: 143-8.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
27. Considine J, LeVasseur S. The Australian triage scale: examining emergency department
405
nurses performance using computer and paper scenarios. Annals of Emergency Medicine 2004;
406
44:516-523.
407
28. Hjelm NM. Benefits and drawbacks of telemedicine. Journal of Telemedicine and Telecare
408
2005; 11:60-70.
409
29. Eldh AC, Ekman I, Ehnfors M. Conditions for Patient Participation and Non-
410
Participation in Health Care. Nursing Ethics 2006; 13:503-14.
411
30. Chioffi, J. Triage decision making: educational strategies. Accident & Emergency Nursing
412
1999; 7: 106-111.
413
31. Cone K. The development and testing of an instrument to measure decision making in
414
emergency department triage nurses. Faculty of the Graduate School Missouri; St Louis
415
University; 2000.
416
32. Hamilton S. Clinical decision making: thinking outside the box. Emergency nurse 2004; 12:
417
18-21.
418
33. Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis
419
for the behavioral sciences. Mahwah, NJ: Erlbaum; 2003.
420
34. Sjöberg L. Methods and practice of psychological research: three disasters. VEST: Journal
421
for Science and Technology Studies 1999; 12: 5-25.
422
35. Trost, J. Enkätboken. Lund: Studentlitteratur; 2001. p. 158-9.
423
37. Teijlingen van E, Rennie AM, Hundley V, Graham W. The importance of conducting and
424
reporting pilot studies: the example of the Scottish Births Survey. Journal of Advanced Nursing
425
2001; 34: 289-95.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
38. Baker TL. Doing Social Research (2nd Edn.), New York: McGraw-Hill Inc. 1994
427
39. Bosma H, Marmot MG, Hemingway H, Nicholson AC, Brunner E, Stansfield SA. Low job
428
control and risk of coronary heart disease in Whitehall ll. British Medical Journal 1997;
314:517-429
23.
430
40. Bland JM, Altman DG. Stastistic notes: Cronbach´s alpha. British Medical Journal
431
1997;314:558-65.
432
41. Brace N, Kemp R, Snelgar R. SPSS for Psychologists. New York: Palgrave Macmillan.
433
2006. p. 331-6.
434
42. Altman DG. Practical statistics for medical research. London: Chapman & Hall.
435
1997.p.277, 320-1.
436
43. Polit DF, Beck CT. Nursing Research- Principles and Methods. Philadelphia. Lippincott
437
Williams & Wilkins. 2004. p. 344-5.
438
44. Graneheim UH, Lundman B. Quality content analysis in nursing research: concepts,
439
procedures and measures to achieve trustworthiness. Nurse Education Today 2003; 24: 105-12.
440
45. The Swedish Code of Statutes: Act concerning Ethical Review of Research involving
441
Humans. Available at:
442
http://www.riksdagen.se/webbnav/index.aspx?nid=3911&bet=2003:460. Accessed
443
February 7, 2011
444
46. World Medical Association Declaration of Helsinki: Ethical Principles for Medical
445
Research Involving Human Subjects. Available at: http://www.wma.net Accessed
446
December 6, 2010
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
47. Herbig B, Büssing A, Ewert T. The Role of Tacit Knowledge in the Work Context of
448
Nursing. Journal of Advanced Nursing 2001; 34: 687-95.
449
48. Meerabeau L. Tacit nursing knowledge: an untapped resource or a methodological
450
headache? Journal of Advanced Nursing, 2006; 34: 687-95.
451
49.Atack A, Rankin J, Then K. Effectiveness of a 6-week Online Course in the Canadian
452
Triage and Aquity Scale for Emergency Nurses. Journal of Emergency Nursing 2005; 31: 436-41.
453
50. Considine J, Hood K. A study of the effects of the appointment of the Clinical Nurse
454
Educator in one Victorian Emergency Department. Accident and Emergency Nursing 2000; 8:
455
71-8.
456
51. Considine J, LeVasseur S, Villanueva E. The Australian Triage Scale: Examining
457
Emergency Department Nurses Performance Using Computer and Paper Scenarios. Annals
458
of Emergency Medicine 2004; 44:516-23.
459
52. Ritchie J, Aldridge Crafter N, Little A. Triage Research in Australia: Guiding Education.
460
Australian Emergency Journal 2002; 5:37-41.
461
53. Stuhlmiller C, Tolchard B, Lyndall T, Crespigny C, Kaluncy R, King D. Increasing
462
confidence of emergency department staff in responding to mental health issues: An
463
educational initiative. Australian Emergency Nursing Journal 2004; 7: 9-17.
464
54. Tippins E. How Emergency Department Nurses Identify and Respond to Critical Illness.
465
Emergency nurse 2005; 13: 24-33.
466
467
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
APPENDIX: Questionnaire (reduced and translated from Swedish, likert scales not
469
presented)
470
471
Demographics472
Your Age? For how long have you been working as registered nurse?
473
For how long have you been working with triage assessment?
474
475
Work contentment in general
476
Do you find your work interesting?
477
Do you find your work stimulating?
478
Are you given opportunities to take initiatives at your work?
479
Are you able to make your own decisions at work?
480
Is it your opinion that; “you have a good work environment”?
481
482
Educational level
483
Have you attended and /or graduated from any additional medical courses?
484
Have your employer offered you any additional training in triage during the last six months?
485
Have you attended any additional training based on simulated patient cases?
486
Do you feel the need for commence and additional triage training – generally?
487
Do you feel the need for commence and additional triage training based on simulated patient cases?
488
489
General attitudes related to triage
490
Is it your opinion that: A triage nurse should possess certain characteristics?
491
If often or sometimes: Give an example
492
Is it your opinion that: A triage nurse should possess these characteristics (in order to minimize patient
493
complications or early death as well as to identify the need for hospital care)?
494
Triage assessment is a nursing task? If never or seldom: Explain…
495
496
Working conditions related to the triage assessment task
497
What was your attitude towards the implementation of Manchester triage?
498
Is it our opinion that:
499
You get sufficient time to evaluate and interpret the information you get from the patient
500
You have sufficient time to evaluate the triage decision
501
You get support gained for the task (from your colleagues and staff at the ED)
502
You have a good cooperation with all the other staff when you are responsible for the triage task
503
504
MTS the method
505
Is it our opinion that:
506
It is difficult to use the Manchester triage system
507
The MTS is a reliable method
508
MTS minimize patient complications or early death as well as to identify the need for hospital care?
509
Every (all nurses) can learn how to practice MTS
510
Not every nurse is suited to work with triage
511
Any nurse can, by training, become more competent in their triage assessment task
512
513
Work satisfaction related to the triage assessment
514
Is it our opinion that:
515
There is a need for triage at your ED
516
Manchester triage is the key to (lead to) a more “prompt” care of the patient
517
The patients are more content after the implementation of Manchester triage
518
It is patient safe to work /perform according to MTS
519
520
Describe a triage assessment that you perceive satisfactory
521
Describe a triage assessment that you perceive as unsatisfactory
522
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
523
524
525
526
527
528
529
530
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60
Table 1 Bivariate regression
Dependent variable, Patient safety n=76 Independent variables:
Pearsons R R-square F-value T-value Sign. Sign.95%
Competence as a facilitator to patient safety
A. Experience 0.73 0.54 81.16 2.24 0.03 sign
MTS as a facilitator to patient safety
B. MTS as a reliabel method 0.65 0.42 50.00 7.07 0.00 sign
Other contributors to patient safety
C. Sufficient time in the triage situation 0.24 0.06 4.41 5.21 0.04 sign
D. Sufficient time for analysis 0.26 0.68 5.07 2.25 0.03 sign
E. Support gained for the task 0.31 0.10 7.44 3.59 0.01 sign
F. Good cooperation at the emerg. dept. 0.21 0.04 3.07 1.54 0.13 not sign
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
Table 2 Multiple regression
Dependent variable, Patient safety n=76
Independent variables: R-square 0.65
Biv.regr. Mult.regr. Difference T-value Sign.
Stand.Beta Stand. Beta
A. Experience 0.73 0.53 0.20 5.92 0.00
B. MTS as a reliabel method 0.65 0.34 0.31 3.89 0.00
C. Sufficient time in the triage situation 0.24 -0.05 0.29 -0.60 0.55
D. Sufficient time for analysis 0.26 0.07 0.19 0.82 0.41
E. Support gained for the task 0.31 0.16 0.15 1.51 0.14
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 Fig.1.
B
C
A
experience
triage model
Ethics
The study complied with ethical procedures according to Swedish law, and the Declaration of Helsinki.Participants in the intervention group were selected by senior managers and by the human resource departments. The survey contained an introductory letter where the background of the study was described. It contained detailed instructions and information stating that participation was voluntary. Participants were informed that they were free to withdraw at any time. They were assured of strict confidentiality and secure data storage. Swedish statutes do not require ethics approval for research that does not involve a physical intervention that affects the participants.