FACULTY OF ODONTOLOGY
Reliability and precision of root length
measurements in cone beam CT images: a
study of adolescents
Fanny Hellberg
,Alexander Coholic
Supervisors: Ayman Al-Okshi, Liselotte Paulsson
Master degree in Odontology, 30 CreditsODONTOLOGISKA FAKULTETEN
Tillförlitlighet och precision vid mätning av
rotlängd i CBCT-bilder: En studie på
ungdomar
Fanny Hellberg
,Alexander Coholic
Handledare: Ayman Al-Okshi, Liselotte Paulsson
Uppsats på masternivå i odontologi, 30 HP3
Abbreviations
2D two dimensional 3D three dimensional
AAOMR American Academy of Oral and Maxillofacial Radiology CBCT cone beam computed tomography
CI confidence interval
CROWDIT crowding displaced teeth CT computed tomography
FOV field of view
ICC intra class correlation coefficient LOA limit of agreement
MME standard moment of measure variance estimator OIIRR orthodontically induced inflammatory root resorption OTM orthodontic tooth movement
PDL periodontal ligament ROI region of interest
SBU statens beredning för medicinsk och social utvärdering (Swedish agency for health technology assessment and assessment of social services)
4
Contents
Reliability and precision of root length measurements in cone beam CT images: a study of
adolescents ... 1
Tillförlitlighet och precision vid mätning av rotlängd i CBCT-bilder: En studie på ungdomar ... 2
Abbreviations ... 3 Abstract ... 6 Background ... 6 Sammanfattning ... 7 Bakgrund ... 7 Syfte ... 7 Metod ... 7 Resultat ... 7 Konklusion ... 7 Introduction ... 8
Fixed orthodontic appliances ... 8
Biological processes during tooth movement ... 8
Root resorption ... 9
Role of radiographic imaging in orthodontics ... 9
Cone Beam Computed Tomography ... 10
Applications of CBCT in orthodontics ... 11
CBCT for diagnostics of root resorption ... 11
Measurements and measurement errors ... 11
Methods of measurement error and reliability assessment ... 13
Intra-class correlation (ICC) ... 14
Bland Altman plot ... 14
Earlier studies of measurement error in orthodontics ... 15
The CROWDIT-project ... 15
The objective ... 16
Hypothesis ... 16
Materials and method ... 17
Study sample ... 17
Radiographic equipment and data processing ... 17
Raters and ratings ... 17
Root length measurement ... 18
Statistical analysis ... 18
5 Sample ... 20 Measurement error ... 20 Reliability of measurements ... 22 Discussion ... 23 Method ... 23
Results and comparison to other studies ... 24
Clinical impact of measurement errors ... 25
Ethical considerations and influence on society ... 25
Future studies ... 27
Limitations ... 27
Conclusion ... 28
Acknowledgements ... 28
6
Abstract
Background: An orthodontic treatment may cause root resorption of varying extent on the involved teeth. The resulting root resorption can be measured in cone beam computed
tomography (CBCT) images. However, measurement results may vary among different raters because of measurement errors, affecting the reliability of the method of measurement. Objectives: To evaluate reliability and precision of measurement of root length following orthodontic treatment in CBCT images. Methods: Ten adolescents participating in a trial of orthodontic treatment were examined with CBCT of both jaws. Five raters measured root length in preselected CBCT images of 100 roots from 90 teeth. The measurements were later repeated by the same raters. Reliability was expressed as intra-class correlation coefficient (ICC 2.1). Measurement error was
calculated with Dahlberg’s formula and standard moment of measure variance estimator (MME)formula. Results: The inter-rater reliability for all raters had an ICC-value of 0,88 for the first
measurement and an ICC-value of 0,87 for the second measurement. The intra-rater reliability for all raters had an ICC-value between 0,84-0,92. Measurement error calculated with the Dahlberg's formula ranged between 0,44-0,64 mm for all teeth for all raters. The largest difference of measurement error between raters was observed in canines, 0,44-1,15 mm. The smallest measurement error was observed in molars, 0,42-0,53 mm. Measurement errors calculated by the MME formula showed similar results. Conclusion: Root length measurements in CBCT-images show high intra- and inter rater reliability. The precision varies between raters and tooth groups but measurements of severe root resorptions (>2 mm) are reliable with this method. The reliability and precision of a method should always be considered when conducting measurement studies. CBCT could be considered a reliable method for measurement of root resorption following orthodontic treatment with different orthodontic appliances.
7
Sammanfattning
Bakgrund: Under en ortodontisk behandling med fast apparatur finns det en risk för att tänderna drabbas av rotresorption. Rotresorptioner kan mätas med hjälp av Cone Beam Computed Tomography (CBCT). Mätresultatet kan dock variera mellan olika observatörer och mätfel kan uppstå vilket påverkar metodens tillförlitlighet.
Syfte: Att beräkna det mätfel som uppstår vid mätning av rotresorptioner som uppstår till följd av en ortodontisk behandling i CBCT-bilder och utvärdera mätmetodens tillförlitlighet. Metod: Tio ungdomar som genomgick ortodontisk behandling undersöktes med hjälp av CBCT-röntgen av båda käkar (tand 16-26 samt 36-46). Fem observatörer mätte tändernas rotlängd i utvalda CBCT-snitt. Studien omfattade 100 rötter från totalt 90 tänder. Mätningen upprepades av samma observatörer vid ett senare tillfälle. Tillförlitlighet utvärderades med intraklass-korrelationskoefficient (ICC 2.1) med 95% konfidensintervall. Mätfelet beräknades med Dahlbergs formel och standard moment of measure variance estimator (MME)-formel. Resultat: Tillförlitligheten mellan observatörer uppmättes till ICC = 0,88 under den första mätningen och ICC = 0,87 vid den upprepade mätningen. Inom observatörerna uppmättes tillförlitligheten till ICC = 0,84-0,92. Mätfelet uppmätt med Dahlbergs formel var 0,44-0,64 mm för samtliga tänder och observatörer. Det största mätfelet uppstod vid mätning av kuspider, 0,4-1,15 mm. Det minsta mätfelet uppstod vid mätning av molarer, 0,42-0,53 mm. Mätfelet vid mätning av premolarer och incisiver var 0,42-0,70 respektive 0,43-0,66 mm. När mätfelet beräknades med MME-formeln erhölls liknande resultat.
Konklusion: Mätning av rotlängd i CBCT-bilder uppvisar hög reliabilitet inom och mellan olika observatörer. Precisionen varierar mellan olika tandgrupper och observatörer, men vid mätning av allvarliga rotresorptioner (>2 mm) är metoden pålitlig.
CBCT anses vara en pålitlig metod för mätning av rotresorptioner som uppstått till följd av ortodontisk behandling. Vid studier där en mätning utförs bör reliabilitet och precision tas i beaktande.
8
Introduction
Orthodontics is the field of studies of maxillofacial and occlusal development and growth, and the diagnosis and treatment of the malocclusions (1). Depending on the age and malocclusion of the patient, treatment can be performed with either fixed or removed appliances.
Fixed orthodontic appliances
Orthodontic appliances use force to move the teeth. The force exerted on the teeth triggers biological mechanisms causing the teeth to move. The appliance comprises three main parts: brackets, archwires and auxiliaries. The bracket is the part that transfers the force from the archwire and auxiliaries to the tooth. It is bonded to the tooth with a resin or a resin cement on an etched enamel surface (2, 3).
The bracket can be divided into two different parts. The base is the part that is aligned against the tooth. It is shaped according to the tooth curvature. The bracket body consists of tie wings and a slot. Tie wings can be used to attach different auxiliaries to the archwire during
orthodontic treatment. The bracket slot is the part into which the archwire is inserted. The angulation, torque and rotation of tooth movement is built in during the shaping of the bracket slot (2). There are different locking mechanisms for the archwire, either orthodontic ligatures or metal clips, the last category being referred to as self-ligating brackets. This category is said to be more tissue friendly and more efficient, however evidence is inadequate (4).
Archwires exert forces on the teeth when placed in the bracket slot, due to the physical
properties of the material. In different tooth alignment stages, archwires of different materials, shapes and sizes are used (2, 4). Additional auxiliaries are used in fixed appliance therapy for extra force application and space holding (4).
Orthodontic forces can be applied continuously or intermittent. Fixed appliance systems use a light continuous force from the archwire. After a certain amount of time, the force is flattened out and the appliance needs to be reactivated by the responsible dentist to once again work effectively. This is referred to as interrupted continuous force (2). The patient visits the clinic every 5th to 8th week for adjustment of the appliance. Treatment duration varies but generally lasts 1-2 years (1).
Biological processes during tooth movement
During orthodontic tooth movement (OTM) the pressure from the orthodontic equipment causes tension in the periodontal ligament (PDL) and surrounding alveolar bone on the side from which the tooth is moving and compression of the corresponding tissues on the opposite side of the tooth. On the sites of tension blood flow increases and osteoblasts from the bone surface are eventually activated. The cells deposit osteoid surrounding the PDL fibers and is later mineralized to form new bone (2, 5, 6).
At the same time, the intense compression of the PDL and alveolar bone on the pressure side of the tooth causes local capillary thrombosis and subsequent cell death. Sterile, cell free amorphous areas referred to as “hyalinization zones” are formed in which vascular invasion and remodeling time is prolonged (7). When the orthodontic force diminishes, cells and blood vessels from adjacent intact PDL gradually invade the hyalinization zones (8). Phagocytic macrophages remove hyalinized tissue and osteoclasts remove adjacent bone. Fibroblast- and
9
cementoblast like cells synthesize collagen fibers attached to cementum and the alveolar wall and tooth attachment of normal width is reestablished (2, 9).
Root resorption
Orthodontically induced inflammatory root resorption (OIIRR) is a common effect of OTM (SBU). Root resorption may appear in conjunction with removal of the hyalinization zones that are formed when an orthodontic force is applied to the teeth. Activated osteoclasts continue to remove the root cementum underlying the hyalinized zones. If the resorbing osteoclasts penetrate the cementum entirely, the underlying root dentine could be resorbed to a varying extent and may cause irreversible root shortening if the tissue is not replaced completely after the orthodontic force diminishes (2, 4, 5).
According to SBU, root resorption up to one third of the root length occurs in 11-28 % of orthodontically treated patients. Teeth with incomplete root development seem to be less resorbed than teeth with fully developed roots (1). Root resorption is usually discovered with the use of panoramic or intraoral apical X-ray. It may be measured in absolute values, relative values or classified according to an index, for instance Malmgren’s root resorption index (10). Qualitative measures of severe root resorption include Malmgren’s index score 3-4. Quantitative measures of severe root resorption are root resorption greater than 2 mm (11). If the patient is likely to experience a heavy amount of root resorption, it is recommended to take radiographs 6 - 9 months into treatment for evaluation (5). The long term consequences of root resorption are yet unknown and the scientific basis is insufficient to determine if tooth vitality is affected by root resorption (1).
Role of radiographic imaging in orthodontics
Before the initiation of an orthodontic treatment, a radiographic image foundation of the patient is usually established. Radiographic images serve as a complementary tool to the clinical examination for diagnosis, treatment planning and follow up. However, radiographic images should only be acquired if the clinician has a clinical indication and result in more good than harm to the patient , due to the stochastic (carcinogenic and genetic) effects of ionizing radiation on living tissue (12).
Depending on the clinical findings and the clinician’s issue, different types of radiographic images may be acquired. Two-dimensional (2D) images such as intra-oral (periapical and bitewing) radiographs, panoramic images or cephalometric images are usually acquired initially during orthodontic treatment planning. Bitewing radiographs could be acquired if the orthodontic patient has a high risk of developing caries prior to fixed appliance therapy, or if a tooth has uncertain prognosis. Periapical radiographs could be acquired for assessment of missing teeth or the eruption path of unerupted teeth. Also, periapical pathology can be diagnosed. When an overview of the patients’ complete dentition is needed, a panoramic image could be an image of choice. Lateral cephalometric radiographs are used to assess skeletal discrepancies (13).
As the orthodontic treatment progresses, additional radiographic images can be acquired to monitor the effect of the orthodontic treatment on jaws, tooth position and facial profile. The latter is very important prior to orthognathic surgery. After completion of the orthodontic treatment, radiographic images can be acquired for comparison as well as longitudinal follow up of the patient's dentition (14).
10
Cone Beam Computed Tomography
Cone Beam Computed Tomography (CBCT) technology was developed in the 1980s, but the devices for dental and maxillofacial imaging were introduced in the 1990s. This three
dimensional (3D) image acquisition technique was more suitable for dentistry compared to Computed Tomography (CT), due to the size of the device as well as the development of image detectors and more powerful algorithms and computers. The CBCT differs from the CT due to its radiation beam, which is cone-shaped rather than fan shaped. This leads to a larger divergence of CBCT beam at upper and lower borders of the field of view (FOV).
During the CBCT image acquisition, a rotary gantry with a fixed sensor and X ray tube rotates around the patient, more specifically around the region of interest (ROI) in the dental and maxillofacial region. While rotating, the device takes from 150 to over 1,000 sequential 2D images. The image volume is then calculated by a computer software program using algorithms in a process called reconstruction, where all the 2D images are put together into one 3D image. The image can then be studied in three planes: axial, sagittal and coronal. The spatial resolution (or sharpness) of the image mainly depends on voxels; the individual volume elements created when the grayscale value of the pixels in each 2D image merge during reconstruction (12, 15).
A CBCT image acquisition exposes the patient to a relatively high effective radiation dose.In a systematic review, Al-Okshi et al (15) reported median effective doses of 28.5 μSv for dental CBCT scans with FOV heights ≤5 cm, 69.9 μSv for FOV heights of 5.1–10.0 cm, and 114.0 μSv for FOV heights >10 cm compared to <1,5 μSv for an intraoral image and 3,85-30μSv for a panoramic image (16). This means that a clinician or radiologist must take many factors into consideration before scanning the patient by CBCT, according to the
ALARA/ALADA - “As Low As Reasonably/Diagnostically Achievable”principle. The optimal image must be obtained with the least amount of radiation exposure possible. The factors to consider are the usage of a continuous or pulsating x radiation generator, the scan volume, the size of the ROI and the scan factors: frame rate, trajectory arc and rotation speed. The exposure parameters such as tube current (mA) and tube voltage (kV) can often be adjusted for optimization (12, 17).
The scan volume depends on the size of the image detector and the beam projection geometry. The scan volume can either be of spherical or cylindrical shape. However, the radiation beam is collimated to limit radiation exposure to the ROI and the scan volume is individually selected, depending on the patients’ needs, to minimize scattered radiation and unnecessary exposure to radiation. The spatial resolution determines the reproduction of fine details in the CBCT image. The image resolution is affected by fill factor (portion of a pixel’s area capable of collecting light), the number of basis images, beam projection geometry, pixel size and the recreational algorithm that is used. The detector frame rate (number of images acquired per second) can be increased to improve the image quality but doing so prolongs reconstruction time and increases radiation exposure to the patient. CBCT scanning time varies from 5 seconds to over 30 seconds; thus, motion artifacts are more likely to occur in CBCT than modern CT (12).
11
Applications of CBCT in orthodontics
CBCT-images have many advantages over 2D images in orthodontics, mainly because of anatomic accuracy, image quality and the possibility to create digital three dimensional models. However, due to the relatively high radiation of CBCT scanning, experts from the American Academy of Oral and Maxillofacial Radiology (AAOMR) have provided guidelines regarding the indications for CBCT in orthodontic treatment. This three point based index takes into consideration whether previous CBCT-images exist, treatment stage, modifying factors and the severity of the oral anomaly (18).
Recent European guidelines do not recommend large FOV (craniofacial extent) CBCT as a standard method of diagnosis and treatment planning in the orthodontic treatment (16). The guidelines suggest that CBCT should only be used when the question, for which imaging is required, cannot be answered adequately by conventional radiography. Hodges et al.
measured the impact of CBCT in orthodontic diagnosis and treatment planning, compared to treatment plans based on conventional radiographs and study models. It was concluded that frequently reported changes of diagnostics and treatment planning occured in cases of severe root resorption, unerupted teeth or severe skeletal discrepancies (19).
CBCT for diagnostics of root resorption
CBCT images are very useful for diagnostics in the maxillofacial area. However, the patient must benefit from the images and before exposing the patient to x rays. In the field of orthodontics, CBCT images can be used to diagnose root resorption and it is indicated in cases of severe external root resorption (18, 19). By measuring the root length in an image and compare it to previous measurements, an assessment of the extent of the root resorption can be done. In a meta analysis, J. Yi et al reported that CBCT images have a higher
sensitivity and specificity (0,89 and 0,92) when diagnosing orthodontically induced root resorptions compared to periapical images (sensitivity 0,68 and specificity 0,89) (20).
Measurements and measurement errors
A measurement is defined as “a set of operations having the objective of determining a value of a quantity” (21). The performance of a measurement method is influenced by the following factors:
• The accuracy, which describes to which extent the obtained values represent the true
values of the object (21).
• The precision, which describes the reproducibility of the method, i.e its ability to
obtain the same value under similar circumstances (22, 23).
• The reliability, which describes the ability of a measurement to differentiate between
subjects or objects (24). Another definition of reliability is that it could be described as the combination of accuracy and precision (25).
The interplay between accuracy and precision is shown in figure 1a-d. Thus, the reliability of a method is better if it performs as figure 1a. Both accuracy and precision is better within the same rater than compared to different raters (26, 27).
12
(a) (b) (c) (d)
Figure 1. Four examples (a-d) of the interplay between accuracy and precision of
a certain measurement method. The accuracy is represented as a red dot and precision as small black dots. Example A represents a method with high precision and accuracy. Example B represents a method with low accuracy and high precision. Example C represents a method with high accuracy and low precision. Example D represents a method with low accuracy and low precision.
However, the obtained value can differ from the true value of the object due to measurement errors, thus bringing a certain degree of uncertainty to the measurements (28). The definition of a measurement error is “the acquired value minus the true value of the measurand” (21). Every method of measurement is susceptible to measurement errors (21). They can be divided into two categories: Systematic or random errors (12, 28). Systematic errors, or bias, are reproducible errors that are consistently larger or smaller compared to the true value of a certain object. The systematic errors, or bias, affect the accuracy of a measurement method (22).
Random errors affect the precision of measurements. These errors differ in size every time a new measurement of the same object is conducted. Both systematic and random errors are affected by observer-, instrument- and subject factors. However, systematic errors can often be diminished or even omitted by careful calibration of the method (12, 28). The random errors however, limit the reliability of any measurement method. Although these errors’ size may be reduced by calibration, they cannot be omitted. This means that measurement errors cannot be eliminated, only diminished by careful planning of the study design and calibration of the measuring method and the raters (12, 22, 29). The interplay between measurement errors and the true value is shown in figure 2a-c.
13 (c)
Figure 2a-c. Examples of the influence of measurement errors on five measurements. Figure 2a shows the
influence of a positive systematic error on five repeated measurements of an object with the true value 1 unit (u). The registered value (1,5 u) is always larger than the true value due to a positive systematic error (0,5 u). Figure 2b shows the influence of random errors on five repeated measurements of an object with the true value 1u. The registered value differ for each measurement (0,3-1,8u) due the different sizes of random errors for each
measurement (-0,7-0,8 u). Figure 2c shows the combined influence of the previous systematic and random errors on five repeated measurements of an object with the true value 1 u. The measurement error, consisting of both systematic and random errors combined, ranges from -0,2-1,3 u. Thus, the registered value ranges from 0,8-2,3 u.
Methods of measurement error and reliability assessment
There are different statistical methods to assess the size of measurement error. In orthodontic literature, measurement errors have mainly been assessed using the Dahlberg formula (15). The Dahlberg formula is defined in figure 3.
Figure 3. The Dahlberg formula. SD is the Dahlberg error, an estimate of the standard deviation, n is the number
of cases and d is the difference between two replicated measurements. It can also be explained as the standard deviation divided by the square root of two. From Springate (30).
However, the Dahlberg formula has its weaknesses. The formula is very sensitive to
systematic errors, making the measurement error much larger than the true value of an object when measuring. Also, it cannot discern between systemic and random errors (12, 27). It must be assumed that there is no systematic error/bias but only random error which is often not the case. As an alternative to the Dahlberg formula, the standard moment of measure variance estimator (MME)- formula has been suggested. This formula provides a reliable estimation of the error even when a constant systematic error is present. According to Springate, the MME-formula is less affected by systemic errors (12). The MME-MME-formula is presented in figure 4.
14
Figure 4. The moments of measure variance estimator formula. SM is the estimate of the standard deviation, n is
the number of cases, d is the difference between two replicated measurements and 𝑑𝑑̅ is the mean of the values. From Springate (30).
Intra-class correlation (ICC)
The intra-class correlation coefficient (ICC) is a measure of reliability, either within the same rater on two separate measurements or between two raters conducting measurements on a certain object. The ICC value is presented as a value between 0 to 1. The closer the value is to one, the better is the agreement (31). Different authors have specific ICC-intervals for
categorising reliability (31).
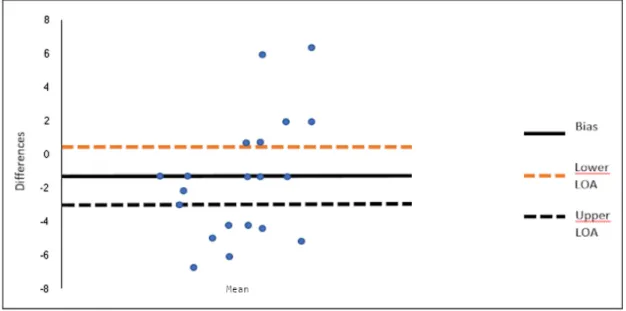
Bland Altman plot
A Bland Altman plot may be used to easily visualize the agreement between two quantitative measurements and to evaluate an eventual bias between the measurements (32, 33). The graph is plotted on an XY-axis, where X illustrates the difference between measurements and Y illustrates the mean of the measurements (34). Limits of agreement are usually added to the plot and tentatively indicates standard deviation (SD) differences. 95% of the data points should lie within ±2 SD of the mean difference according to Bland and Altman who introduced the plot. The limits of agreement are calculated by using the mean and standard deviations of the differences of measurements which must not be equal to acceptable limits (which are based on for instance biological considerations) (33). Normally distributed data points indicates that there is no relationship between the values obtained and the mean
difference (35). One should use statistical tests to determine whether the distribution is normal or not (34).
Figure 5. Example of a Bland-Altman plot with lines of limits of agreement (LOA). Bias is the mean of the
differences. In the example above, over 50% of the values are situated above or under the limits of agreement, which indicates either that the chosen method evaluated is not optimal or that limits of agreement chosen are too narrow (33).
15
Earlier studies of measurement error in orthodontics
To date only a few studies have been published on reliability and precision of root resorption measurements following orthodontic treatment measured in CBCT-images. The authors of this study performed a PubMed research on studies of measurements of root resorption
following orthodontic treatment on CBCT including a measurement of the measurement error. It resulted in four studies.
Iury O. Castro et al (36) studied the frequency of apical root resorption following orthodontic treatment with the use of CBCT on 1256 roots from 30 patients. CBCT images were obtained before and after treatment. All teeth were examined except for third molars. Root length was measured from cusp tip to root apex by one rater. The measurement was repeated in a two week interval by the same rater. The measurement error calculated with Dahlbergs’ formula was 0,36 mm. H. Lund et al evaluated the accuracy and precision of CBCT in measurement of root length during orthodontic treatment on 13 patients (37). CBCT images were obtained at the start of the treatment, six months into treatment and after treatment. Two teeth from each tooth group were measured on every patient. Root length was measured from CEJ to root apex by one rater. All measurements were made with intervals of at least two days. The measurement error calculated with Dahlberg's formula was 0,32 mm.
C. Aman et al (38). investigated the incidence and severity of orthodontically induced root resorption on maxillary incisors undergoing orthodontic treatment using CBCT. It was a retrospective study of 160 patients and CBCT images were taken at the start as well as in the end of the orthodontic treatment. Root length was measured from CEJ to the root apex by one rater. The measurements were repeated in 10% of the patients in a minimum of three weeks after the first measurement. Intra rater measurement error was evaluated with ICC and was calculated to ICC = 0,99. J. P. Schwartz evaluated the frequency of root resorption during orthodontic treatment by CBCT images (39). It was a retrospective study of 23 patients and all dental roots except for third molars were examined. CBCT images were obtained before and after treatment. Root length was measured from the cusp tip to the root apex by one rater. Measurements were repeated two weeks later by the same rater. Intra rater measurement error was evaluated with ICC and was calculated to ICC = 0,91.
The CROWDIT-project
According to the Swedish agency for health technology assessment and assessment of social services (SBU), there is a lack of evidence for the effects of buccally placed fixed appliance to treat crowding in adolescents (1, 40). In the department of Orthodontics Malmö University, a project called CROWDIT (Crowding Displaced Teeth) is conducted. The project is a
randomized multicenter study, and its aim is to compare and evaluate the effects of standard edgewise appliance to self-ligating brackets. The factors studied are both the biological effects and the psychological effects of the treatments. One of the adverse effects of fixed appliance therapy that will be studied in the CROWDIT-project is root resorption (41). According to some studies, self-ligating brackets cause less root resorption than standard edgewise appliances (42). Other studies have found inconclusive results (43). To further research the effects of self-ligating and conventional brackets on root resorption in adolescents, a prospective follow up study using CBCT-images of all teeth treated with both types of appliances will be conducted. However the measurement error of the method that will be used, proposed by Al-Okshi et al (44), is not studied. The size of the measurement error, if
16
large enough, could render the results unreliable. Thus, a registered shortening of the root length could not be discerned between a biologic process leading to a root resorption or an error in the measurement. The result from this study would then be used to compare the result of a future follow up study.
The objective
The main objective of this study is to evaluate precision and reliability of different root length measurements in CBCT-images according to a method proposed by Al-Okshi et al (44). It is of importance for future measurements of root resorption when evaluating different fixed appliance therapies on adolescents with crowded teeth, as measurement errors will impact the results. Additionally, comparing five raters could yield a better understanding of the
applicability of the method as a tool for research and root length measurements in CBCT-images.
Hypothesis
17
Materials and method
This is an observational study of precision and reliability of root length measurements in CBCT images in adolescents. This study uses the same study sample and methodology, consisting of CBCT-unit settings and measuring technique for root length measurements in CBCT-images, as used in a study by Al-Okshi et al (44). The CBCT-images are acquired from a randomized controlled trial in a project called the CROWDIT-project and it has been given ethical approval from The Regional Ethical Review Board, Lund, Sweden, (D.no: 2014/647). The study was reported in accordance with Guidelines for Reporting Reliability and Agreement Studies (24).
Study sample
Ten adolescents included in the clinical trial in the CROWDIT-project (mean age 13 years and 3 months; the sample was between 12-17 years) were selected randomly. The male-to-female ratio was 1:1. The inclusion criteria were that the subjects should have permanent teeth, crowding and tooth displacement.
The CBCT-images were acquired between March 2016 and March 2017. Central and lateral incisors, canines, first and second premolars and first molars in both jaws were examined.
Radiographic equipment and data processing
The CBCT-images were obtained with 3D Accuitomo® 170 (J. Morita, Kyoto, Japan) units in two departments, using the same scanning protocol and operating at 80 kV and 3 mA. The option of 360 revolution of the X-ray source and standard acquisition mode with a FOV of 8
cm (diameter) x 8 cm (height) and 160-μm voxel size were used to examine both jaws
together. Ten patients were oriented with the same plane setting controlled by a specialists in dental and maxillofacial radiology as a part of the study protocol.
Ten CBCT volumes were stored in Digital Imaging and Communications in Medicine file (DICOM) format and prepared with i-Dixel software on a workstation. For all images, a BARCO (MFGD 1318; BARCO, Kortrijk, Belgium) 18.10 greyscale liquid crystal display monitor with a luminance of 400 cd/m2 and resolution of 1280 x 1024 pixels was used.
Raters and ratings
Five raters were selected to ensure a diverse level of professional experience: two were specialists in dental and maxillofacial radiology with 25 and 30 years of experience in radiology respectively (rater 1 and 2), one was a specialist in orthodontics with 10 years of experience (rater 3) and two raters were dental students at master level (rater 4 and 5). The raters were aware of the purpose of the study and blinded to each other’s measurements. A radiologist with experience of CBCT selected cross sectional CBCT images and sites to be measured using i-Dixel software. Measurements were derived from the CBCT images using Image J software. The reading room illumination was dimmed, below 50 lux and kept constant. The reading distance was approximately 50-60 cm. There were no restrictions on reading time.
18
Before the measuring, raters attended an educational session given by an odontology doctor in orofacial radiology, demonstrating the procedure using examples of root length measurement on CBCT images. During the session, the raters were given examples of a procedure similar to what they were expected to perform. The aim was to familiarize the raters with the image J software and measurement procedure.
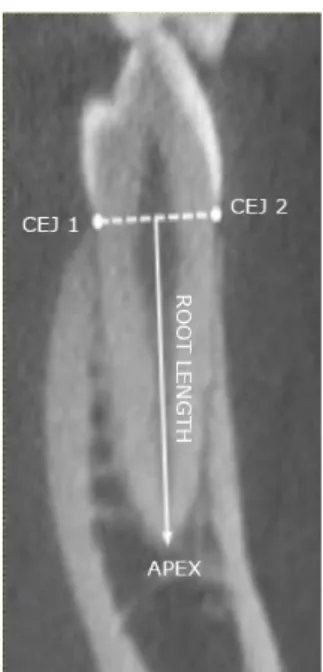
Root length measurement
The measurements of root length in all CBCT-images were replicated by all five raters in order to calculate measurement error and intra-rater reliability. The measuring session were conducted between February 2018 and October 2018.
Root length was measured between the midpoint between the two cementoenamel junctions (CEJs) and root apex (see figure 6). When the root was curved, measurement could be performed in two steps: first measure was the distance from the midpoint between the CEJ and the point where the root start to curve and secondly from this point to the root apex. The distances were then summed up. In case of a premolar with two apices, the buccal root was measured. Upper molars were examined by measuring the palatal root and the distobuccal root in the first quadrant and the mesiobuccal root in the second quadrant.The root length was registered in millimeters (mm) and rounded to one decimal. The patient information was masked on all images.
Figure 6. Example of conducted root length measurement in CBCT-images. A hypothetical line was drawn
between the CEJs. The measurement of the root length was conducted from the midpoint of the hypothetical line to the apex of the tooth. Modified image from Al-Okshi (15).
Statistical analysis
All results were collected in a computer database for statistical analysis. The measurement error was calculated with both the Dahlberg-formula and the moments of measure variance estimator (MME). Additional Bland-Altman plots were made to evaluate measurement errors.
19
For analyzing both inter- and intra-rater reliability of the method, intra-class correlation coefficient (ICC 2.1) with 95% confidence intervals (CI) was calculated. The measurement error was calculated in Microsoft Excel (Microsoft Office 2016). To calculate the ICC, IBM SPSS® Statistics v. 22.0 (IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL) was used.
20
Results
Sample
Ten subjects that fulfilled the inclusion criteria were included in this study. CBCT-images of 90 teeth were acquired. In total, the root length of 100 (30 molar, 40 premolar, 10 canine and 20 incisor) roots were measured twice for comparison by each of the five raters.
Measurement error
According to the Bland-Altman plots, the systematic errors ranged from -0,25-0,25 mm (see figure 7a-e). Most of the measurements were within the upper and lower limits of agreement. The mean bias level ranged from -0,25 to 0,25 mm for different raters. The Bland-Altman plots also show some outliers at every rater, however the majority of measurements lies within ±1,96 SD. As a general feature, the measurements of rater 4 and 5 were more centered around the mean, whereas rater 1-3 were more evenly spread out within ±1,96 SD. Rater 4 and 5 had outliers further away from the bias compared to rater 1-3.
(a) (b)
(c) (d)
Figure 7a-e. Bland-Altman plots representing the
agreement of two root length measurements for each rater. The limit of agreement (LOA) was set to ±1,96 standard deviations (SD). Figure 7a shows a bias level of 0,06mm. Figure 7b shows a bias level of 0,25. Figure 7c shows a bias level of 0,02. Figure 7d shows a bias level of -0,25. Figure 7e shows a bias level of -0,19.
21
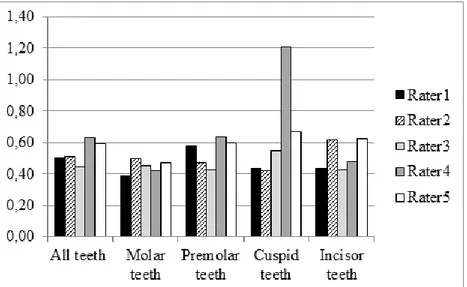
Overall measurement error measured with the Dahlberg's formula ranged between 0,44-0,64 mm for all teeth for different raters, see Figure 8. The measurement error for molar teeth showed the smallest difference between raters, 0,42-0,53 mm. The largest difference of measurement error between raters was observed in canines, 0,44-1,15 mm. The measurement error between raters for premolars and incisors ranged between 0,42-0,70 and 0,43-0,66 mm respectively, see Figure 7.
The measurement error calculated with MME ranged between 0,44-0,63 mm for all teeth between raters, see Figure 9. The smallest difference of measurement error between raters was noted at molar teeth, 0,39-0,50 mm. The largest difference of measurement error between raters was noted at canines, 0,42-1,21 mm. For premolars and incisors, the measurement errors between raters varied between 0,43-0,64 and 0,43-0,62 mm respectively, see Figure 9.
Figure 8. The measurement error in (mm) calculated according to the
Dahlberg formula for all teeth as well as for each tooth group for all five raters.
Figure 9. The measurement error in (mm) calculated according to the
22
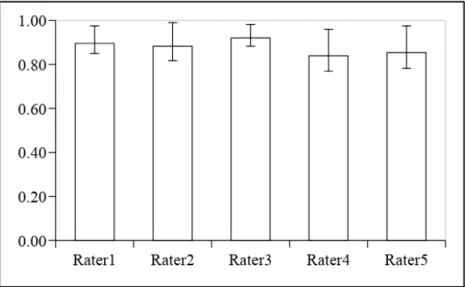
Reliability of measurements
The inter-rater reliability for all raters had an ICC-value of 0,88 (CI 0,84-0,91) for the first measurement. For the second measurement the inter-rater reliability had an ICC-value of 0,87 (CI 0,81-0,91), see figure 10. The intra-rater reliability measured for five raters had an ICC-value between 0,84-0,92. Rater four had the lowest ICC-ICC-value: 0,84 (CI 0,77-0,89) and rater three had the highest ICC-value: 0,92 (CI 0,88-0,95), see figure 11.
Figure 10. Inter-rater reliability expressed as intra-class correlation coefficients with 95% confidence intervals for the two measurements of root lengths in CBCT images.
Figure 11. Intra-rater reliability expressed as intra-class correlation coefficient with 95% confidence intervals for measurements of root lengths in CBCT specified for all five raters.
23
Discussion
The findings of the present study demonstrated high reliability for root length measurement in CBCT-images. Measurement error range calculated by the Dahlberg formula was between 0,44-0,64 mm for all teeth for all raters. The measurement varied between raters and tooth groups. Similar results of measurement error were calculated by the MME-formula. Thus, the hypothesis was incorrect.
Method
As previously mentioned, the quality of CBCT images is highly dependent on imaging parameters such as the size of the FOV. A larger FOV increases noise and artefacts, however, a small FOV could result in shading and truncation artefacts because of asymmetrical masses outside of FOV affecting the projection. It is recommended to keep the FOV just as small as to cover the ROI in order to minimize exposure of radiation to the patient (45). In this study, a FOV of 8 cm X 8 cm was used in order to cover both upper and lower jaw. The CBCT was also set to full rotation, 80 kV and mA modified to 3 to adjust to patient size to gain optimal image quality while minimizing radiation dosage as recommended by Al-Okshi et al (14). The studied sample was selected from images which were obtained from a clinical trial of fixed orthodontic appliances. Therefore, no additional exposure was performed for this study.
Earlier studies have used the same measuring technique when measuring root length in CBCT-images, i.e. measured from the midpoint between two CEJs to the apex of the tooth. However, the units and settings for CBCT-images varies among the studies (36, 45). Similar measuring technique has been used when measuring root length in periapical images (46). The midpoint between the CEJs was chosen over the incisal edge or cusp tip, as the latter could alter the morphology due to for example grinding. Although the measuring technique is commonly used, it has some drawbacks. It cannot measure changes, for example root
resorptions, occuring in the buccolingual direction. Also, only one cross-section of each tooth was chosen to conduct a measurement on. This might not be of concern when measuring initial root length, as the cross section displaying optimal root length could be chosen. However, in follow up studies evaluating root resorption during and/or after treatment, only one cross section of the volume might not be enough to assess the whole root resorption, as multiple surfaces might be involved and one cross section might not be able to display the whole resorption damage.
Five raters performed root length measurements of 100 roots twice, to evaluate the inter- and intra rater reliability and the precision of the method. Several raters conducting measurements with this method will yield a better understanding of its performance when used by different raters. Also, by comparing the results of raters with varying experience of radiographic image measurements, an indication of the method´s reliability for different raters could be evaluated (23). In this study, the measurement errors varied among the raters. However both inter- and intra rater agreement in this study was almost perfect according to Landis and Koch (47) and one could question whether a total of five raters would be needed in a future follow up study of the clinical trial regarding treatment with two different types of fixed orthodontic appliances.
24
Results and comparison to other studies
There was a slight difference between measurement errors calculated with Dahlberg´s formula and the MME-formula. According to Springate, the Dahlberg formula is more affected by bias compared to the MME-formula (30). However in this study, the bias sizes were relatively small. Hence, the impact of the bias would not affect the results from the Dahlberg formula particularly. The relatively small size of the bias could be due to the calibration of the raters before the initiation of the measurements. However, the persisting bias could be explained by an inherent tendency of the raters to either systematically overestimate or underestimate the position of the CEJs or the apical apex. The proposed sample size to assess random error is 25-30 samples (30). In this study, a total of 100 roots were measured which makes the overall estimation of the random error reliable. If the measurement error of different groups of teeth were to be calculated separately, the group of canines (n=10) is too small for reliable results. Since the largest measurement error was obtained in canines according to both Dahlberg’s formula and the MME-formula, the deviant result may be explained by the fact that the sample size was apparently smaller than the other groups of teeth. According to our study results, measurement error varies between raters and also between different tooth groups compared to a general measurement error of all teeth. This should be considered when calculating measurement error and conducting measurements of root resorption in CBCT-images. One measurement error of rater 4 exceeds 1 mm, making the measurement for canines less precise by the rater in question. The measurement error could perhaps be
explained by poor image sharpness or difficulties for the rater to discern between anatomical landmarks (CEJ, apex) on that particular image. The large measurement error was probably due to a large difference of 4,59 mm between the first and the second measurement of tooth 13 on one patient for this rater. As the formulas use differences in obtained values between measurements to calculate measurement error, one large measurement error could impact the result greatly, especially if the sample size is small.
Compared to the study conducted by Lund et al (45), our measurement errors were larger than the measurement error of their study: 0,32 mm, despite using similar methodology. The study by Lund et al, was however conducted by only one rater and some measurements and re-measurements were conducted after 2 days, increasing the risk of recall bias. Our study showed that measurement errors differ in both tooth groups and between rater.
The inter rater-reliability between measurements was almost perfect, according to the definitions suggested by Landis and Koch (47). There was no difference between
measurements due to overlapping CIs around the ICCs. The intra rater-reliability between measurements was generally higher than the inter rater reliability for the more experienced raters and lower for inexperienced raters. The CIs around the ICCs overlapped, indicating no difference. Other studies that have evaluated the reliability of root resorption measurements in CBCT-images showed ICC-values between 0,91-0,99 (38, 39). These studies used one rater to measure root resorption, thus as previously mentioned the reliability varies between raters.
The factors affecting reliability and precision of this method could be explained by the raters' experience of measurement and image interpretation, since diagnostic accuracy in
radiographic images increases with increasing experience of radiographic diagnosis (GRRAS) (24). Also, more experienced raters have a better ability to discern between gray-scale
25
contrasts (48), making the measurements more precise due to a more precise placement of measuring points on root apex and CEJ.
Clinical impact of measurement errors
Large measurement errors brings uncertainties into research as well as clinical work. If image measurements are used in clinical practice to evaluate the treatment progression and to
observe adverse effects of the treatment, i.e. root resorptions, large errors could possibly affect the treatment. If root shortening is registered after six to nine months, it is encouraged to postpone the treatment two to three months and continue it to let the tissues repair and to further evaluate the root resorption. In some cases the treatment should be altered (49). Thus, large measurement errors could hypothetically cause unnecessary treatment delays and treatment cessations. In other cases the cessation of treatment could be justified due to actual root resorption, especially if the difference is larger than the measurement error.
According to a systematic review and meta-analysis of studies on evaluation of OIRR
following orthodontic treatment with fixed appliances using CBCT, mean OIRR was found to be 0,9 mm. Central incisors were affected the most; OIRR = 0,8 mm, lateral incisors had an average OIRR of 0,7 mm, canines had an average OIRR of 0,4 mm. Posterior teeth (premolars and molars) had an average OIRR of 0,2 mm (50). According to another meta analysis of OIRR following orthodontic treatment with fixed appliances using CBCT, mean OIRR was 0,77 mm. Mean OIRR on central maxillary incisors was 0,84 mm. Mean resorption of lateral maxillary incisors and maxillary canines was 0,9 mm and 0,68 mm respectively (51). For some teeth and raters the measurement error exceeded previously mentioned OIRR values. Thus, the measured root resorption is uncertain. However, in cases of severe root resorptions of > 2 mm, where a modification of the orthodontic treatment is needed, CBCT could be considered a reliable method for root length measurement as the measurement error does not exceed the root resorption.
In this study, the largest measurement errors were spotted on canine teeth for some raters. The permanent maxillary canines are on average the longest tooth in the mouth and the roots are particularly long and thick. In comparison, the permanent maxillary incisor has a smaller root (52). Large measurement errors might influence the diagnosis and the prognosis of the lateral incisor more than the canine since the lateral incisor stability might be more affected by root shortening. However, as to date the scientific evidence of the OIRR effect on tooth vitality is insufficient (1).
Ethical considerations and influence on society
The aforementioned superiority of CBCT-images to diagnose root resorptions leads to a discussion regarding the importance of CBCT-images in orthodontics. According to the European commission, CBCT images should only be performed in orthodontics when
clinically and ethically justified, most importantly because of the risk of stochastic damage to the cells in the examined area (16). There is no minimum threshold for this causation,
although the risk of complications increases as radiation dose increases (12). Especially younger subjects are more susceptible to stochastic damage caused by radiation. If stochastic damage was caused at young age, it could show mutations and cellular dysfunction after many
26
cycles of mitosis (53). Thus, the younger the subject is, the larger is the risk of cancer
development from stochastic damage. There is a linear connection between radiation dose and the risk of developing cancer, and there is no lower or higher threshold. The dose to develop cancer is estimated to be 3-4% per Sievert (Sv) for adults and 10-20% per Sv for children (54). Radiographic images have to be acquired on strict indication according to the ALARA/ALADA-principle and be of benefit to further diagnosis. Also, the condition in question should do more than the method used to diagnose it.
This leads to the problem regarding whether it is ethical to use CBCT-images to diagnose root resorptions. Even though root resorption is a common side effect of orthodontic treatment, scientific evidence of its effect on teeth in long term is inadequate (1). According to
Consolaro et al, even severely shortened teeth could maintain their function (55). However, if the subject would develop periodontal disease in the future, the risk of losing the shortened teeth would probably be greater. Thus, the use of CBCT-images to diagnose root resorption is questionable. The radiation exposure of one CBCT-image emits the same amount of radiation as at least 10 intraoral images (17), which is almost enough for a whole-mouth examination. From a clinical standpoint, it is then more justifiable to use periapical images to evaluate treatment outcome on patients treated with fixed orthodontic appliances. In a clinical setting, evaluation of root resorption would perhaps not be made by measuring of root length, but rather with the use of an index to evaluate the severity of root shortening, perhaps the one proposed by Malmgren et al (10).
The CBCT-images obtained and evaluated in this study are parts of a larger study, evaluating the performance of two different fixed appliances. For research purposes it could be
justifiable to obtain images for the treatment evaluation. If measurement in CBCT-images can show that one fixed appliance treatment is better than the other, or if there is no difference, it would influence the orthodontist to use the best and most cost effective treatment.
There is also a cost associated with both CBCT-imagery and fixed orthodontic appliance treatment for the society. The use of CBCT as a diagnostic method during an orthodontic treatment costs more than conventional intraoral imaging (56). CBCT equipment is generally more expensive than intra oral radiological equipment. The use of CBCT does also require longer time of specialist analysis of radiographic images and maintenance as well as accommodation of the equipment is more expensive for CBCT than for conventional radiographic equipment. Altogether this affects the total cost of the diagnostic procedure. Furthermore, intra oral radiology could be considered more cost effective than the use of CBCT for identifying and evaluating root resorption as a result of orthodontic treatment. One should also include caution of radiation dose in the analysis of cost-effectiveness (57, 58). The cost of head and neck cancer treatment the first year after treatment in a region in Sweden year 2015 was 81 million SEK (59). In Sweden there is a 2,2% increase of head and neck cancers (59, 60). Thus, the increasing subjects with cancer cost the society millions in
treatment cost and the lost income is not included. Thereby it is of importance to minimize the stochastic effect of radiation exposure to reduce the risk of cancer development as much as possible. In Sweden, if the malocclusion is severe enough, the patient is granted orthodontic treatment (61). Otherwise the patient has to pay the whole cost by herself. The cost of treatment with fixed orthodontic appliance in Sweden is estimated to be 30 000 SEK per
27
treatment (1). The self-ligating brackets are more expensive than conventional brackets, thus they should be more cost effective than conventional brackets if they were to be used by orthodontists. However, at the moment this is uncertain and further studies have to be made (41).
Future studies
The material for this study was CBCT images of ten adolescents prior to orthodontic treatment and therefore constitutes baseline. As a part of the ongoing CROWDIT-project, follow up CBCT-images will be conceived from the same adolescents after one year of orthodontic treatment. It would be in our interest to measure root length in CBCT-images of the same participants after one year of treatment to investigate whether root resorption has occurred, and in that case compare the results to the measurement error achieved in this study. By doing so, one might be able to estimate the actual impact of the measurement error when evaluating root resorptions in CBCT-images.
Limitations
The method used measures the root length from the CEJ to the root apex. However, root resorptions do not necessary only affect the apex, and could also occur on other parts of the root. This could lead to an under-registration of root resorptions. Perhaps a better method to assess the size of the root resorption could be one that was proposed by Aras et al (62), who studied the volumetric root loss using CBCT-images. This could yield a more truthful result, as the resorbed areas vary in size and a point on the apex isn't always representable for the whole resorption.
There are some other methodological factors that could influence the result that should be mentioned. The measurements and re-measurements were conducted by some raters nine months apart. The methodology suggested by Al-Okshi et al suggested a period of three weeks to minimize recall bias (15). According to SBU, accordance is better when
measurements are performed over a short period of time (63). The observer’s practice may change with experience or knowledge achieved between two particular measurement occasions (25). This is especially true for the two dental-students. The quality, mostly the sharpness, varied between the CBCT-images. Discerning between anatomical structures in sharp images was easier than in less sharp images, thus leading to more precise placement of measuring endpoints and thereby more reliable results. The measurements were conducted on different times of day. The fatigue of the raters could possibly influence the ability to discern between anatomic structures in the picture (48). Perhaps if the measurements were conducted on the same time of day, this source of error would be ruled out.
The statistical analysis of measurement error was conducted on tooth-groups and not for single teeth. To gather the single teeth into tooth groups could possibly cause discrepancies between the measurement errors of the single teeth and the tooth-groups they were
categorised into. To showcase the measurement errors of the single teeth would present a more accurate result. However, to calculate the measurement error for single teeth, a larger sample size would be needed. As proposed by Springate, at least 25-30 of each single tooth would be needed to calculate the measurement error using either the Dahlberg´s formula or the MME (30).
It should also be acknowledged that some of the subjects could possibly have not fully developed roots due to their age (64). This should be taken into consideration when making
28
follow up measurements of the same subjects one year later. Also, orthodontically induced root resorptions heal better in younger subjects compare to older (65), influencing the size of the root resorption.
Conclusions
• The method of root length measurements by measuring roots from all tooth groups
from the midpoint between the two CEJs to the root apex in CBCT-images acquired with 3D Accuitomo® 170 with settings of 80 kV, 3mA, a FOV of 8 cm x 8 cm and full rotation shows high intra- and inter rater reliability between five raters. The precision varies between raters and tooth groups, however, as most of the
measurement errors varies between 0,4 mm and 0,6 mm, severe root resorptions (≥ 2
mm) could be discovered and adequate treatment initiated.
• Due to high inter- and intra rater reliability values for five raters for root length measurements with this method, future follow up studies using this method for evaluating root resorption after orthodontic treatment with different fixed appliances could use fewer raters.
• The reliability and precision of a method should always be considered when
conducting measurement studies.
• CBCT could also be considered a reliable method for measurement of root resorption
following orthodontic treatment with different orthodontic appliances.
Acknowledgements
We would first of all like to thank our supervisors Liselotte Paulsson and Ayman Al-Okshi for letting us participate in the CROWDIT-project and providing us with the excellent guidance and expertise when needed to write this paper. Quoting Tina Turner: “You're simply the best”. Further we would like to thank Christina Lind and Madeleine Rohlin for their participation in this study, which yielded some interesting results. Finally we would like to thank Per-Erik Isberg for his help with the statistical analysis.
29
References
(1) Statens beredning för medicinsk och social utvärdering (SBU). Bettavvikelser och tandreglering i ett hälsoperspektiv, Stockholm, Sverige, 2005.
(2) Graber L, Vanarsdall R, Vig K. Orthodontics: current principles and techniques. 5th ed. St Louis Mosby cop; 2011.
(3) Phillips R, Anusavice K, Shen C, Rawls H. Phillips' science of dental materials. 12th ed, St. Louis, Mo: Elsevier/Saunders; 2013.
(4) Cobourne M, DiBiase A. Handbook of Orthodontics. 2nd ed, Edinburgh, Scotland: Elsevier; 2016.
(5) Proffit W, Fields H, Sarver D. Contemporary Orthodontics. 5th ed, St. Louis, Mo: Elsevier/Mosby; 2013.
(6) Masella R, Meister M. Current concepts in the biology of orthodontic tooth movement. Am J Orthod Dentofacial Orthop 2006; 129: 458-468.
(7) Brudvik P, Rygh P. Transition and determinants of orthodontic root resorption-repair sequence. Eur J Orthod 1995; 17: 177-188.
(8) Gianelly A, Goldman H. Biologic Basis of Orthodontics. Lea & Febiger; 1971. (9) Ireland A, McDonald F. The orthodontic patient. Oxford: Oxford University Press; 2003. (10) Malmgren O, Goldson L, Hill C, Orwin A, Petrini L, Lundberg M. Root resorption after orthodontic treatment of traumatized teeth. Am J Orthod 1982; 82: 487-491.
(11) Makedonas D, Lund H, Hansen K. Root resorption diagnosed with cone beam computed tomography after 6 months and at the end of orthodontic treatment with fixed appliances. Angle Orthod 2013; 83: 389-393.
(12) White S, Pharoah M. Oral radiology: principles and interpretation. 7th ed. St. Louis, Mo: Mosby/Elsevier; 2014.
(13) Isaacson et al. K. G. Guidelines for the use of radiographs in clinical orthodontics. 2015. https://www.bos.org.uk/portals/0/public/docs/general%20guidance/orthodontic%20radiograph s%202016%20-%202.pdf. (Read 180412)
(14) Scarfe W, Angelopoulos C. Maxillofacial Cone Beam Computed Tomography: principles, techniques and clinical applications. Cham: Springer; 2018.
(15) Al-Okshi A. Maxillofacial cone beam computed tomography (CBCT): aspects on optimisation. MUEP 2018
(16) European Commission. European guidelines on radiation protection in dental radiology. Luxembourg: Office for Official Publications of the European Communities; 2004.
30
(17) ADA Science I. Radiation exposure in dentistry. 2017. http://www.ada.org/en/member- center/oral-health-topics/x-rays. (Read 170111)
(18) Scarfe W C, Azevedo B, Toghyani S, Farman A G. Cone Beam Computed Tomographic imaging in orthodontics. Aust Dent J 2017; 62: 33-50.
(19) Hodges R J, Atchison K A, White S C. Impact of cone-beam computed tomography on orthodontic diagnosis and treatment planning. Am J Orthod Dentofacial Orthop 2013; 143: 665-674.
(20) Yi J, Sun Y, Li Y, Li C, Li X, Zhao Z. Cone-beam computed tomography versus periapical radiograph for diagnosing external root resorption: A systematic review and meta-analysis. Angle Orthod 2017; 87: 328-337.29
(21) Lira I. Evaluating the Measurement Uncertainty Fundamentals and Practical Guidance. Bristol and Philadelphia: Institute of Physics Publishing; 2002.
(22) Hulley Stephen B. Designing clinical research: 3rd ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2007.
(23) Segen J. Concise dictionary of modern medicine. New York; London: McGraw-Hill, 2006.
(24) Kottner J, Audigé L, Brorson S, Donner A, Gajewski BJ, Hróbjartsson A et al.
Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. J Clin Epidem January 2011; 64: 96-106.
(25) Houston W J B. The analysis of errors in orthodontic measurements. Am J Orthod 1983; 83: 382-390.
(26) Statens beredning för medicinsk och social utvärdering (SBU). Utvärdering av metoder i hälso- och sjukvården: en handbok. 2 ed. Stockholm, Sverige, 2014.
(27) Nationalencyklopedin. Wilhelm Röntgen.
https://www.ne.se/uppslagsverk/encyklopedi/l%C3%A5ng/wilhelm-r%C3%B6ntgen. (Read 180221)
(28) Everitt B, Palmer C. Encyclopaedic companion to Medical Statistics. 1st ed. London, Great Britain: Hodder Education; 2005.
(29) Strålsäkerhetsmyndigeten. SSMFS 2008:35 Strålsäkerhetsmyndighetens föreskrifter om allmänna skyldigheter vid medicinsk och odontologisk verksamhet med joniserande strålning.
https://www.stralsakerhetsmyndigheten.se/publikationer/foreskrifter/ssmfs-2008/ssmfs-200835/ (Read 18031)
(30) Springate S D. The effect of sample size and bias on the reliability of estimates of error: a comparative study of Dahlberg's formula. Eur J Orthod 2012; 34: 158-163.
(31) Koo Terry K, Li Mae Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J chiropract med 2016; 15: 155-163.
31
(32) Bland J M, Altman Douglas G. Statistical methods for assessing agreement between two methods of clinical measurement. Int J Nurs Stud 2010; 47: 931-936.
(33) Giavarina D. Understanding Bland Altman analysis. Biochem Med 2015; 25: 141-151. (34) Kalra S, Kalra B. Inositols in Midlife. J Pract Cardiovasc Sci 2017; 3: 36-38..
(35) Donatelli R E, Lee S J. How to report reliability in orthodontic research: part 1. Am Orthod Dentofacial Ortho 2013; 144: 156-161.
(36) Castro I O, Alencar A H, Valladares-Neto J, Estrela C. Apical root resorption due to orthodontic treatment detected by cone beam computed tomography. Angle Orthod 2013; 83: 196-203.
(37) Lund H. Cone beam computed tomography in evaluations of some side effects of orthodontic treatment. Swed Dent J Suppl 2011; 219: 4-78.
(38) Aman C, Azevedo B, Bednar E, Chandiramami S, German D, Nicholson E et al. Apical root resorption during orthodontic treatment with clear aligners: a retrospective study using cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2018; 153: 842-51. (39) Schwartz J, Raveli T, Almeida K, Schwartz-Filho H, Raveli D. Cone beam computed tomography study of apical root resorption induced by Herbst appliance. J Appl Oral Sci 2015; 23: 479-485
(40) Statens beredning för medicinsk och social utvärdering (SBU). Buckalt placerad fast apparatur vid trångställning med displacering av tänder hos ungdomar. 2016.
https://www.sbu.se/sv/publikationer/kunskapsluckor/buckalt-placerad-fast-apparatur-vid-trangstallning-med-displacering-av-tander-hos-ungdomar-/ (Read 180906)
(41) Johansson Kristina. Behandling med fast tandställning. 2018.
http://www.tandlakartidningen.se/wp-content/uploads/2018/04/Forskarskolan-2018_Johansson.pdf.
(Read: 180830)
(42) Yi J, Li M, Li Y, Li X, Zhao Z. Root resorption during orthodontic treatment with self-ligating or conventional brackets: a systematic review and meta-analysis. BMC Oral Health 2016; 16: 125.
(43) Weltman Belinda, Vig Katherine W L, Fields Henry W, Shanker S, Kaizar E. Root resorption associated with orthodontic tooth movement: a systematic review. American J Orthod and Dentofacial Ortho 2010; 137: 462-476.
(44) Al-Okshi A, Paulsson L, Rohlin M, Ebrahim E, Lindh C. Reliability of assessment of root lengths and marginal bone level in CBCT and intraoral radiography: a study of adolescents. http://muep.mau.se/handle/2043/23279. (Read 180315)
(45) Lund H, Grondahl K, Hansen K, Grondahl H G. Apical root resorption during
orthodontic treatment. A prospective study using cone beam CT. Angle Orthod 2012; 82: 480-487.
32
(46) Mirabella AD, Artun J. Prevalence and severity of apical root resorption of maxillary anterior teeth in adult orthodontic patients. Eur J Orthod. 1995 Apr;17(2):93-9.
(47) Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977 Mar;33(1):159-74.
(48) Martin C J, Sharp P F, Sutton D G. Measurement of image quality in diagnostic radiology. Applied Radiation and Isotopes 1999; 50: 21-38.
(49) Feller L, Khammissa R A, Thomadakis G, Fourie J, Lemmer J. Apical External Root Resorption and Repair in Orthodontic Tooth Movement: Biological Events. Biomed Res Int 2016; 2016: 1-7.
(50) Samandara A, Papageorgiou SN, Ioannidou-Marathiotou I, Kavvadia-Tsatala S, Papadopoulos M. Evaluation of orthodontically induced external root resorption following orthodontic treatment using cone beam computed tomography (CBCT): a systematic review and meta-analysis. Eur J Orthod 2019; 41: 67-79
(51). Deng Y, Sun Y, Xu T. Evaluation of root resorption after comprehensive orthodontic treatment using cone beam computed tomography (CBCT): a meta-analysis. BMC Oral Health 2018; 18: 116
(52) Scheid Rickne C, Weiss G, Woelfel J. Woelfel's dental anatomy. 9th ed. Philadelphia: Wolters Kluwer; 2017.
(53) Garinis G A, van der Horst G T, Vijg J, Hoeijmakers J H. DNA damage and ageing: new-age ideas for an age-old problem. Nat Cell Biol 2008; 10: 1241-1247.
(54) Aspelin P, Pettersson H. Radiologi. 1st ed. Lund: Studentlitteratur; 2008. (55) Consolaro A. Effects of medications and laser on induced tooth movement and associated root resorption: four key points. Dental Press J Orthod 2013; 18: 4-7.
(56) Christell H. Cost and benefits of cone beam computed tomography: for maxillary canines with eruption disturbance. MUEP 2017.
(57) de Freitas M, Beltrao R, Janson G, Henriques J, Chiqueto K. Evaluation of root resorption after open bite treatment with and without extractions. Am J Orthod Dentofacial Orthop 2007; 132: 143
(58) de Freitas J, Lyra O, de Alencar A, Estrela C. Long-term evaluation of apical root resorption after orthodontic treatment using periapical radiography and cone beam computed tomography. Dental Press J Orthod 2013; 18: 104-112.
(59) Nyman Jan, Beran Martin. Huvud- och Halscancer Regional nulägesbeskrivning – Standardiserat vårdförlopp. 2015. https://www.cancercentrum.se/globalassets/vara-
uppdrag/kunskapsstyrning/varje-dag-raknas/vast/huvud-och-halscancer_nulagesbeskrivning.pdf. (Read 190127).
(60) Cancerfonden. Cancerfondsrapporten 2018. 2018.
https://static-files.cancerfonden.se/Cancerfondsrapporten2018_webb_(2)_1521607903.pdf. (Read190127).
33
https://folktandvardenskane.se/globalassets/media/pdf/vardgivare_ortodonti/ortodonti--skaneindex.pdf (Read 190127).
(62) Aras I, Unal I, Huniler G, Aras A. Root resorption due to orthodontic treatment using self-ligating and conventional brackets: a cone-beam computed tomography study. J Orofac Orthop 2018; 79: 181-190.
(63) Statens beredning för medicinsk och social utvärdering (SBU). Kronisk parodontit : prevention, diagnostik och behandling : en systematisk litteraturöversikt. Stockholm, Sverige, 2004.
(64) Koch G, Poulsen S. Pediatric dentistry: a clinical approach. 2nd ed. Oxford: Wiley-Blackwell; 2009.
(65) Owman-Moll P, Kurol J, Lundgren D. Repair of orthodontically induced root resorption in adolescents. Angle Orthod 1995; 65: 403-410.