Implant-supported
zirconia-based fixed dental
prostheses
A literature review
Hannah Fransson, K10
Handledare:
Christel Larsson, Avdelningen för Materialvetenskap och Teknologi
Minh Le, Avdelningen för Materialvetenskap och Teknologi
Examensarbete (30 hp)
Malmö högskola
Tandläkarprogrammet
Odontologiska fakulteten
Februari 2013
205 06 Malmo
Summary
The increasing interest in ceramic materials has mostly centered on zirconia-based ceramics lately. Zirconia-based fixed dental prostheses (FDPs) is an ongoing subject of discussion. There are a few articles published on the subject but with varying quality and there is no review on implant-supported zirconia-based FDPs to be found. The purpose of this study is to evaluate available studies on zirconia-based implant-supported FDPs, reporting the results from clinical studies.
Three electronic databases were searched for studies reporting on zirconia-based FDPs. The electronic search was complemented by a hand-search made from the reference lists of the retrieved full-text articles. The search result yielded 4,253 titles. Based on pre-established criteria, 5 full-text articles were obtained. One study did not separate the results between tooth-supported and implant-supported groups, why it was excluded from further analysis. Three studies reported on cross-arch restorations, and the majority of the FDPs included were cross-arch restorations. Sufficient data for calculation of cumulative survival-and complication-rates was available in 4 studies. Analysis was based on 47 implant-supported FDPs. This review concludes that cross-arch implant-supported zirconia-based FDPs could be considered as a treatment alternative. The results are, however, based on small number of studies with relatively few FDPs included thus interpretation of the results should be made with caution. Further studies are needed to evaluate how these types of constructions stand the test of time.
Abstract
Det ökade intresset av keramiska material har främst centrerat kring zirkoniabaserade keramer på sistone. Zirkoniabaserade fastsittande broar är ämne för en pågående diskussion. Det finns några få publicerade studier på ämnet men med varierande kvalitet och det finns ingen sammanställning av implantatstödda zirkoniabaserade broar. Syftet med den här studien är att bedöma tillgängliga studier på tidigare nämnda konstruktion och redogöra för resultat från kliniska studier.
På elektroniska databaser söktes artiklar på implantatstödda zirkoniabaserade
fastsittande broar. Artiklar som också rörde tandstödda konstruktioner inkluderades i sökningen. Sökningen kompletterades med en manuell referenssök på de utvalda fulltextartiklarna. Sökningen resulterade i 4,253 artiklar. Baserat på förutbestämda kriterier inhämtades 5 fulltext artiklar. En av de studierna skilde inte på tandstödda och implantatstödda grupper i resultatet, därför exkluderaderades den från fortsatta analyser. Tre studier redogjorde för helkäkeskonstruktioner, och majoriteten av de inkluderade konstruktionerna var helkäkeskonstruktioner. Tillräcklig data för uträkning av överlevnad och komplikationsrisk var tillgänglig i 4 studier. Analysen bar baserad på 47 implantatstödda konstruktioner. Slutsatsen av litteraturstudien blir att zirkoniabaserade helkäkeskonstruktioner som är implantatstödda kan övervägas som behandling. Resultaten är dock baserade på få studier med relativt få
konstruktioner inkluderade, varför tolkning av resultaten bör göras med försiktighet. Fortsatta studier behövs för att konkludera hur den här typen av konstruktioner håller med tiden.
Introduction
Fixed dental prostheses (FDPs) have the ability to restore the functions lost, such as eating and speaking, due to a person’s loss of teeth. The most commonly used technique is the porcelain-fused-to-metal FDP, a metal-ceramic restoration1. Metal-ceramic restorations have passed the test of time and are recognised as reliable solutions for fixed prostheses. New, upcoming materials are therefore compared to them2,3.
All-ceramic FDPs were introduced in the 1960s as an alternative treatment to conventional metal-ceramic restorations 4,5. At first, all-ceramic restorations, were limited to small size anterior restorations due to the high risk of fracture. With increasing estetic demand, the development of high-strength ceramics contributed to the use of all-ceramic FDPs no longer being limited to small size restorations and could be recommended for both anterior and posterior regions2,4,5. Multiple
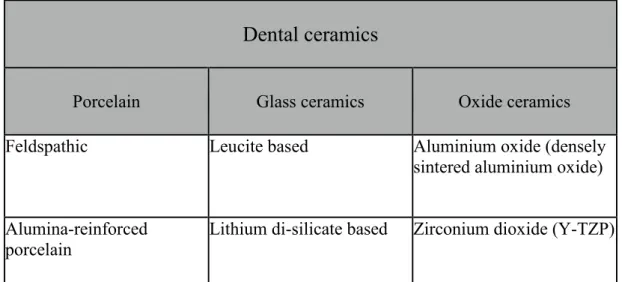
all-ceramic materials and systems are available for clinical use today, there is not a single universal material or system for all clinical situations6. They can be divided in three groups; porcelain, glass ceramics and oxide ceramics 7 as shown in figure 1.
Dental ceramics have been used for many years. Dental porcelains were first
introduced in the eighteenth century and were attractive for dental restorations due to their excellent esthetic1. Ceramics are characterised by high hardness and high E-module but brittle and often with low flexural strength, why several methods are used to improve strength and clinical performance of the material8,9. The principle behind the strengthening methods are to reinforce the material in such a way that it can withstand or deflect the energy at a crack tip. One method is to incorporate crystals in the glass matrix of a porcelain material. In 1965 a porcelain reinforced with alumina crystals was introduced, which increased the strength of the material sufficiently to make it successful for single anterior restorations, but still not strong enough to be recommended for molar restorations. In the early 1990’s a glass ceramic containing leucite-crystals was introduced, followed by a glass ceramic containing
lithia-disilicate crystals in the late 1990‘s. Recently this material has been further developed and these materials are recommended for use for single crowns in anterior and
posterior areas as well as for small anterior FDPs. A high-strength oxide ceramic material was developed in 1994 with the introduction of a material system that densely sinters high-purity aluminium oxide, reaching 99,9% alumina content1. In terms of all-ceramic FDPs systems, yttra-stabilized tetragonal zirconia polycrystal (Y-TZP), commonly called zirconia, have been recommended and suggested to be the most successful system for the future. Partly because of excellent biocompatibility, good esthetics and optical properties, as ceramics in general are known for, but
mainly because of the fracture resistance and high flexural strength1,4-6,10 as seen in fig 2.
As well as the materials are being improved, so is the technology of production. The modern CAD/CAM methods have made it possible to produce FDPs with unlimited numbers of units in high-strength oxide ceramics 11.
Zirconia is a polymorphic material that occurs in 3 forms; cubic structure, tetragonal phase and monoclinic phase, the latter in room temperature. By adding stabilizers such as yttrium oxide, the tetragonal phase can be maintained metastably at room temperature, creating Y-TZP1,6.
There are other based materials although Y-TZP is the most studied zirconia-based material at this time3 and in the last decade, the majority of zirconia
frameworks have been made of Y-TZP2,10.
Clinical studies have shown that the main cause for failure of most all-ceramic FDPs is fracture in the connector area, although that does not include zirconia-based FDPs1,11. Since Y-TZP is a strong ceramic material, core failures are rare
complications10,19. This is mostly due to a transformation toughening it undergoes. When a stress is applied to a material a crack develops that tries to propagate through the material. Metastable tetragonal zirconia grains adjacent to the crack tip can then expand by transforming to the monoclinic crystal form. This transformation involves a volume increase of the grains which places the crack in compression and stops it from propagating. Additional stress is needed for the crack to be able to propagate further1,3.
The resistance of all-ceramic constructions to fracture also depends on the stability of the support to reduce strain in the beam of the prosthesis. Implants can be used to replace the natural abutments, when teeth are lost. Implants are characterized by direct contact between bone and the loaded implant and lack of shock absorption, sensory response and movement. The biomechanical support provided by implants differs from the support provided by natural teeth as the implants lack periodontal ligament12. It is reported in an in vitro study that the fracture load decreased in tooth-supported FDPs, compared to implant tooth-supported teeth, probably due to the mobility of natural teeth, and implants may provide a more solid support1,12,13.
Systematic reviews on metal-ceramic FDPs imply that the observed survival of FDPs after 10 years ranged between 85% and 95% for both tooth-supported and implant-supported constructions21. The survival rates of modern all-ceramic restorations are now close to the ”gold standard” of metal-ceramic restorations19. According to a systematic review of the literature that evaluated tooth-supported all-ceramic restorations survival, the 5year survival rate resulted 93%3, although, studies on all-ceramics often has a limited follow-up time compared to studies on metal-all-ceramics.
Zirconia stands out as an abutment material because of its excellent linking between estetics and mechanical properties. Ceramic materials have been found to accumulate less plaque and plaque with reduced vitality, compared to other restorative
materials14-17. The clinical significance is uncertain however. A review comparing metal and ceramic abutments found a numerical difference with higher frequency of biological complications around metal abutments compared to ceramic abutments but the difference was not statistically significant18.
Clinical studies have revealed that the most common technical complications in FDPs, and in particular implant-supported zirconia FDPs, is fracture of the esthetic veneering porcelain1-3,6,10,19,20. Ceramics are highly brittle, they cannot withstand deformations of more tan 0,1% without fracturing12. The risk of veneering material fracture are higher for implant-supported restorations than tooth-supported
restorations12,19. The short-term veneering fracture rate can be as high as 89% which is significant higher than metal-ceramic restorations2.
As mentioned, there is continuous development on ceramic materials in an attempt to improve the mechanical properties without damaging the esthetic quality9. Most studies assessing the fracture resistance of Y-TZP-based restorations have shown promising results10 however, clinical studies on FDPs so far mainly concerned tooth-supported FDPs. Studies on implant-tooth-supported FDPs are few and often with limited follow-up times5,12,13.
Since zirconia-based restorations are a topic of interest and the number of studies is increasing, a systematic review evaluating results is warranted.
The aim of this study is to evaluate available studies on zirconia-based implant-supported FDPs also including full-arch restorations, reporting the results from clinical studies.
Materials and methods
A search was made in the Sciencedirect, Cochraine and PubMed database, in November 2013. Two blocks of search terms were built and then combined. One block contained only text terms and the second one both MeSH terms and free-text terms (fig 3). The search words were; ”all-ceramic”, ”all-ceramics”, ”ceramic”, ”yttrium”, ”yttria”, ”ytzp”, ”y-tzp”, ”zirconium”, ”zirconia” and ”dental restoration”, ”dental restorations”, ”fixed partial dentures”, ”fixed partial prosthesis”, ”fixed partial prostheses”, "Denture, Partial, Fixed"[Mesh].
A limit was set for language; articles had to be written in English, and with an abstract. A limit was also set for publication dates; Jan 2000 to Oct 2013.
Initially titles of relevance were screened and followed by a screening of abstracts by two independent reviewers. Articles reporting on results from clinical trials on zirconia-based FDPs were retrieved in full-text format. Fig 4 describes the process of identifying the 5 full-text articles selected from an initial yield of 4253 titles.
A hand-search was made from the reference lists of the selected articles.
Study selection
Studies on implant-supported zirconia-based FDPs were included. Patients had to have been clinical examined at the follow-up.
Studies were selected from set inclusion and exclusion criteria. Inclusion criteria were; prospective or retrospective clinical trials reporting on implant-supported zirconia-based FDPs. Solely implant-supported FDPs were included.
Case-studies were excluded.
The original search concerned zirconia-based FDPs and was made without specify the type of support. The original search is a part of a systematic review on
tooth-supported and implant-tooth-supported Y-TZP FDPs which is still in progress. From that search, articles on implant-supported FDPs was selected to analyse for this master thesis. 2
Definitions
Survival was defined as the reconstruction remaining in situ at the follow-up examination visit irrespective of its condition.
Soft tissue complications, periimplantitis, bone loss exceeding 2 mm and esthetic complications were included in Biological complications for implant.
Technical complications for implant reconstructions denoted mechanical damage of the suprastructures. Among these, fractures of the implants, fracture of screws or abutments, fractures of the luting cement (loss of retention), fractures or deformations of the framework or veneers, loss of the screw access hole restoration and screw or abutment loosening were included21.
Zirconia or zirconia-based was defined as Y-TZP.
Life table analysis was performed and cumulative survival and complications rates were calculated.
Results
The results of the search in the databases are shown in fig 5. The hand-search of references did not include any new articles.
In total, 5 studies were fulfilling the inclusion criteria and included in the present review5,23,25,26,29. Three was retrospective studies25,26,29, one was a pilot study23, one was a randomized prospective study 5. Two studies 25,29 reported on both implant-supported and tooth-implant-supported FDPs, only the figures on implant-implant-supported FDPs are included here. Mean observation time ranged from 42 to 96 months. Three
studies5,25,26 reported on cross-arch restorations, two of them25,26 reported on both upper and lower jaw, one of them5 only on lower jaw. One study23 reported on both posterior and anterior restorations. One study29 did not specify on positions of the FDPs. In total most FDPs were cross-arch. One study29 did not separate the results between tooth-supported and implant-supported groups or specify when failures occurred, why it was excluded from further analysis. Sufficient data for calculation of cumulative survival-and complication-rates were available in 4 studies5,23,25,26.
Analysis was based on 47 implant-supported FDPs.
The cumulative 5-year survival rate was 100%. The cumulative 8-year survival rate was 100%, though based on one study23.
The cumulative complication rate was 40%. The cumulative 8-year survival rate was 100%, though based on one study23.
Discussion
This review included 4 articles on implant-supported Y-TZP restorations. Most studies included cross-arch restorations. 47 implant-supported Y-TZP restorations were analysed and cumulative survival-and complication rates were calculated.
The interest in durable, metal-free, estethic alternatives to metal-ceramics FDPs has led to a higher use of FDPs based on oxide ceramics22. Earlier studies for all-ceramic restorations report on survival rates on 88-100% after 2-5 years in service6 and studies on zirconia-based FDPs only report survival rates of 100%. Though, clinical studies have so far mostly concerned FDPs supported by natural teeth22. Since results from studies on tooth-supported FDPs cannot be directly transferred to implant-supported reconstructions, it is important to evaluate studies on implant-supported zirconia-based restorations. An in vitro study12 suggests that all-ceramic fixed partial dentures can be used in combination with dental implants. The solid support gained from implants might thus be beneficial for the outcome of such treatment due to decreased strain and stress levels in the prosthesis when loaded on implants compared to when loaded on natural teeth. Clinical studies are, however, needed to confirm these findings as there are more factors that influence the final clinical outcome.
This present review found a 5-year survival rate at 100% for implant-supported zirconia-based FDPs, where survival defines a restoration remaining in situ at the follow up visit. 100% survival is, as mentioned earlier, in line with earlier studies2,22, although very few earlier studies have reported on evaluation time longer than 3 years. Literature on the subject of implant-supported zirconia-based FDPs is still limited to few articles with few patients and short follow-up, although 5 years are considered well accepted. With a growing interest in implant-supported restorations and Y-TZP restorations, a greater number of published studies on the subject are likely to be expected in the near future.
The strength of an all-ceramic restoration mainly depends on the ceramic material used, core-veneer bond strength, crown thickness and design of the restorations6. Total fractures are rarely occurring in Y-TZP1,19, which is consistent with no failures
in this review. A reason for total fractures being rare in Y-TZP is the transformation toughening it undergoes when a small crack occurs.
Another reason for few failures could also be that with implant-supported restorations enough space can be obtained in order to have a favourable connector dimension. Maybe that could partly explain why fractures on implant-supported Y-TZP
restorations are rare. The clinical fracture resistance of all-ceramic FPDs is related to the size, shape and position of the connectors and the span of the pontic13. Ceramic FDPs must have a connecting surface area of at least 6.25mm3, and implant treatment can be planned and the implant positioned in a way that enough connecting surface is easily acquired.
While the zirconia cores have performed excellent, complications shifted to the veneers, despite the use of veneering strategies long practiced with metal-core-restorations19. Chipping of the veneering porcelain in posterior FDPs is a relatively frequent complication in metal-ceramic FDPs as well, although for zirconia
restorations the number of fractures in the porcelain per FDP can be three times higher than of the veneer ceramics for metal1,27.
With a 40% complication-rate for implant supported zirconia FDPs chippings are important to discuss. Particularly since the majority of all-ceramic restorations rely on veneers to achieve clinically acceptable esthetics on high-strenght cores19. Often minor chippings are not a cause for replacing the restorations, especially since many of the patients are unaware of them until the clinical examination, but a fracture is always undesirable and is in one way a failure and indicates merely survival rather than success of the restoration.
A majority of the FDPs studied in this review had more than only one chipping fracture, although it should be noted that chippings was not a reason for replacement of the construction and could be polished, but the 40% complication rate is consistent with previous studies, although it can vary from 0% to 88% from one study to the other2,21,24.
The cause of veneer chippings on zirconia cores is complex19. Veneers fractures are not related to a specific type of restoration (cemented, screw-retained, crown or FDP). The parameters, which were shown to be associated with chipping where the nature of the antagonist, the presence of parafunctional habits and the type of support. More fractures are observed in implant-supported restoration with ceramic restorations as antagonist in the presence of parafunctional habits2. The problem with veneer fractures does occur in both implant- and tooth-supported zirconia restorations, although the risk of veneer fractures increases with implant-supported
restorations19,22. Probably because the biomechanical support differs between tooth- and implant-supported FDPs5. Tooth-supported, with its periodontal ligament, allows for shock absorption, sensory function, and tooth movement. Implants have direct contact with the bone resulting in a lack of those properties24. Since implants provide a rigid support for the framework and reduce the bridge bending, they on the other hand reduce the proprioception and therefor may increase the occlusal stress possibly leading to higher chip-off rates, and most veneer fractures originate from occlusal surfaces2.
Different factors may influence veneer cracking, as material factors; differences in thermal expansions coefficient and thermal conductivity between core and ceramic, firing shrinkage of ceramics, flaws on veneerings and poor wetting by veneering on core3,19. But non-material-related factors, such as thickness ratios and core or framework design, also play a significant role19. It has also been discussed that
manufacturing procedures can increase the risk of veneer fractures. To avoid exposing the zirconia framework to unfavourably high temperatures during porcelain firing, creating undesirable phase transformation, porcelain of a low firing temperature was used. The modification to lower the firing temperature affects the mechanical properties of the veneering porcelain, making it more susceptible to tensile forces24. The influence of slow cooling procedures of the veneering ceramic was introduced recently by manufacturers to reduce failures, but it need further evaluation in future clinical studies2.
Dental ceramics, particularly porcelains, are vulnerable to slow crack growth; a circumstance that increases the probability of chippings. At low continuous loads, especially in humid environment, a crack slowly but continuously grows in length, degrading the strength for the ceramic19.
In the posterior regions the veneering porcelain is not only for esthetic reasons. A major drawback for zirconia restorations is the suggested material inherent
accelerated ageing. In a humid environment, spontaneous slow transformation from the tetragonal phase to the more stable monoclinic phase occurs in zirconia grains at relatively low temperatures. It initiates at surface grains, and then later progresses toward the bulk material causing a reduction of spontaneous catastrophic failure. A veneer covering the core therefore possibly has additional beneficial effects.Therefore maybe non-veneered zirconia should be avoided.
Though, the relationship between ageing of zirconia frameworks and long-term clinical performance need to be investigated in further evaluations20.
Fractures of porcelain veneered on zirconia are generally remaining within the veneer and only rarely involving the interface, just as for porcelain fused to metal, suggesting that the bond itself is adequate. The bond strengths to zirconia cores are lower than those of metal ceramics19.
The chipping rates differ a lot between the included studies. Olivia et al and Pozzi et al25,26 have the lowest chipping rates, respectively 4,2%25 and 12%26. Compared with the other two studies5,23 where the chipping rates were 69% and 80%.
This could possibly be explained partly by the use of a night-guard. The use of an occlusal night-guard decreased the chipping occurrence in one study2. The two articles mentioned first provided their patients with a night-guard, the latter two did not specify any such treatment. The results indicates that a night-guard could possibly bring down the chipping rate, although not enough studies are available to make that conclusion.
The 5-year complication-rate for implant-supported zirconia FDPs at 40%, results in a success-rate at 60%. A successful restoration is a restoration without any
complication whatsoever. The limited success-rate of the material depends mostly on the relatively high frequency of veneer fracture, and has been a cause for some concern, although patients are reportedly satisfied, which in a way could be considered to a success.
Maybe caution should be taken when placing a zirconia restoration in patients with bruxism, partly because the maximum bite force occurs in the molar region in cases of parafunctional behaviour such as bruxism13. Mundt et al27 report on a chipping rate at 100% after 40 month on patients with signs of bruxism, though, it is a clinical
evaluation on tooth-implant-supported restorations so it can only be considered an indication. Koenig et al2 shows parafunctional habits being one parameter associated with chippings in all-ceramic FDPs. Although he has a broader definition of
parafunctional habits including more than just bruxism.
It has been suggested that the results on a 100% survival-rate could be overrated as most of the studies exclude patients with parafunctional activity2. In this review only one study included23 report exclusion of patients with bruxism. It could be discussed though how well such an exlusion is executed since bruxism is a condition which is sometimes hard to diagnose.
One study included in this review23 reported follow-up on 8 years, giving a cumulative 8-year survival rate of 100%, however it is based solely on one study which also was the one study excluding bruxism, as discussed. No more
complications where reported the following 6-8 years either, giving an 8-year cumulative complication rate of 40%. This indicates that the risk of complications occurring has a peak the first years and then the risk decreases.
It is suggested that the level of bacterial products is higher on titanium abutments than zirconium oxide3. It is also suggested that a screw-retained implant, that facilitates retrieveability in case of complications, has no risk of retained excess cement which has been suggested to increase the risk of periimplantitis28.
In this review biological complications are limited. Soft tissue complications, as bleeding on probing, is excluded. This because the studies included in this review did not specify how frequently it is observed, and some trials have had hygiene control every fourth to twelfth month, while others have not.
It is shown that zirconia restorations have adequate mechanical resistance for both anterior and posterior restorations3 but it is suggested earlier that all-ceramic implant-supported FDPs of two to five units can be considered a treatment alternative5 but caution should be considered concerning extensive implant-borne zirconia
frameworks, such as cross-arch FDPs with the presence of ceramic restorations as antagonist since it is argued to promote framework fractures, and also due to lack of evidence of clinical long-term data2,20. Although this review suggest that implant-supported zirconia can be considered a treatment alternative as cross-arch FDPs.
It is possibly an advantage that the majority of the patients included in the studies in this review were treated in specialized rehabilitation centres and accordingly to the ideal measurements. However, the results are in line with previous studies since fractures in Y-TZP restorations are reportedly rare. It would benefit with studies including more patients and where treatment is given in general dentistry. That would broader the perspective.
Conclusion
Further studies, with longer evaluation times, are needed to conclude how zirconia-based implant-supported FDPs perform in the long run. The findings and calculations in this review are limited due to the few articles identified but it implies that cross-arch implant-supported zirconia-based FDPs could cautiously be considered as a treatment alternative.
References
1. Larsson C. Zirconium dioxide based dental restorations. Swed Dent J 2011; 213 (suppl)
2. Koenig V, Vanheusden AJ, Le Goff SO, Mainjot AK. Clinical risk factors related to failures with zirconia-based restorations: an up to 9-year
retrospective study. J Dent 2013; 41: 1167-1174
3. Manicone PF, Rossi Iommetti P, Raffaelli L. An overview of zirconia
ceramics: basic properties and clinical applications. J Dent 2007; 35: 819-826 4. Della Bona A, Kelly JR. The clinical success of all-ceramic restorations. J Am
Dent Assoc 2008; 139(suppl): 8s-13S
5. Larsson C, Vult von Steyern P. Five-year follow-up of implant-supported Y-ZTP and ZTA fixed dental prostheses. A randomized, prospective clinical trial comparing two different material systems. Int J of Prosthodontics. 2010; 6: 555-561
6. Conrad HJ, Seong WJ, Pesun IJ. Current ceramic material and systems with clinical recommendations: a systematic review. J Prosthet Dent 2007; 98: 389-404
7. Kelly JR ,Nishimura I, Campbell SD. Ceramics in dentristry: historical roots and current perspectives. J Prosthet Dent 1996; 75: 18-32
8. Ehrnford L. Dentala keramer. In; Ehrnford L. De vita materialen i praktiken. Malmö. 2006-2007;220-292.
9. Deany IL. Recent advances in ceramics for dentistry. Crit Rev Oral Biol Med 1996; 7: 134-143
10. Komine F, Blatz MB, Matsumura H. Current status of zirconia-based fixed restorations. J Oral Sci 2010 52: 531-9
11. Larsson C, Holm L, Lövgren N, Kokubo Y, Vult von Steyern P. Fracture strength of four-unit Y-TZP FPD cores designed with varying connector diameter. An in-vitro study. J Oral Rehabil 2007; 34: 702-709
12. Vult von Steyern P, Kokubo Y, Nilner K. Use of abutment-teeth vs dental implants to support all-ceramic fixed partial dentures. Swed Dent J 2005; 29: 53-60
13. Kokubo Y, Tsumita M, Sakurai S, Torizuka K, Vult von Steyern P et al. The effect of core framework designs on the fracture loads of all-ceramic fixed partial dentures on posterior implants. J Oral Rehabil 2007; 34: 503-507 14. Hanh R, Weiger R, Netuschil L, Bruch M. Microbial accumulation and vitality
on different restorative materials. Dent Mater 1993; 9: 312-316
15. Kawai K, Urano M. Adherence of plaque components to different restorative materials. Oper Dent 2001; 26: 396-400
16. Rosentritt M, Behr M, Burgers R, Feilzer AJ, Hahnel S. In vitro adherence of oral streptococci to zirconia core and veneering glass ceramics. J Biomed Mater Res B Appl Biomater 2009; 91:257-263
17. de Medeiros RA, Vechiato-Filho AJ, Pellizzer EP, Mazaro JV, dos Santos DM et al. Analysis of the peri-implant soft tissues in contact with zirconia
abutments: an evidence-based literature review. J Contemp Dent Prac 2013; 14: 567-572
18. Sailer I, Philpp A, Zembic A, Pjetursson BE, Hammerle CHF, Zwahlen M. A systematic review of the performance of ceramic and metal implant abutments
supporting fixed implant reconstructions. Clin Oral Implants Res 2009; 20: 4-31
19. Rekow ED, Silva NR, Coelho PG, Zhang Y, Guess P, Thompson VP. Performance of dental ceramics: challenges for improvements. J Dent Res. 2011; 90:937-952
20. Guess PC, Att W, Strub JR. Zirconia in fixed implant prosthodontics. Clin Implant Dent Relat Res 2012; 14: 633-645
21. Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported FDPs and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res 2007; 18: 97-113
22. Larsson C, Vult von Steyern P, Sunzel B, Nilner K. All-ceramic two- to five-unit implant-supported reconstructions. Swed Dent J 2006; 30: 45-53
23. Larsson C, Vult von Steyern P. Implant-supported full-arch zirconia-based mandibular fixed dental prostheses. Eight-year results from a clinical pilot study. Acta Odontol Scand. 2013; 71: 1118-1122
24. Larsson C, Vult von Steyern P, Nilner K. A prospective study of implant-supported full-arch yttria-stabilized tetragonal zirconia polycrystal mandibular fixed dental prostheses: three-year results. Int J Prsosthodont 2010: 23: 364-369
25. Olivia J, Olivia X, Olivia JD. All-on-three delayed implant loading concept for the completely edentulous maxilla and madible: a retrospective 5-year follow-up study. Int J Oral Maxillofac Implants 2012; 27: 1584-159 26. Pozzi A, Holst S, Fabbri G, Tallarico M. Clinical reliability of CAD/CAM
cross-arch zirconia bridges on immediately loaded implants placed with computer-assisted/template-guided surgery: a retrospective study with a
follow-up between 3 and 5 years. Clin Implant Dent Relat Res 2013; 5 doi: 10.1111/cid.12132
27. Mundt T, Heinemann F, Schankath C, Schwahn C, Biffar R. Retrospective and clinical evaluation of retrievable, tooth-implant supported zirconia-ceramic restorations. Acta Odontol Scand 2013; 71: 1326-1334
28. Wilson TG. The positive relationship between excess cement and periimplant disease: a prospective clinical endoscopic study. J Periodontol 2009; 80:1388-1392
29. Wolleb K, Sailer I, Thoma A, Menghini G, Hämmerle C. Clinical and
radiographic evaluation of patients receiving both tooth-and implant-supported prosthodontic treatment after 5 years in function. Int J of Prosthodontics 2012; 25: 252-259
30. Vult von Steyern P. Dental ceramics in clinical practice. In: Nilner K. Karlsson S. Dahl BL. A textbook of fixed prosthodontics. The scandinavian approach. Stockholm: Gothia, 2013; 205-222
Figures
Dental ceramics
Porcelain Glass ceramics Oxide ceramics
Feldspathic Leucite based Aluminium oxide (densely
sintered aluminium oxide)
Alumina-reinforced
porcelain Lithium di-silicate based Zirconium dioxide (Y-TZP) Fig 1. A classification of dental ceramics. Ref; Fixed Prosthodontics, the
Scandinavian approach30 and Larsson C. Zirconium dioxide based dental restorations1.
Classification Flexure strength (MPa)
Feldspathic porcelain Porcelain 50-70
Alumina-reinforced
porcelain Porcelain 150
Leucite-reinforced glass
ceramics Glass ceramic 70-180
Lithia-disilicate reinforced
glass ceramics Glass ceramic 350-400
Densely sintered aluminum
oxide Oxide ceramic 600-700
Y-TZP Oxide ceramic 900-1300
Fig 2. Flexure strength of some ceramic materials. Ref; Larsson C. Zirconium dioxide based dental restorations1.
Block 1
(n = 29,218) (n = 32,210) Block 2
all-ceramic or dental restoration or all-ceramics or dental restorations or ceramic or fixed partial dentures or yttrium or fixed partial prosthesis or yttria or fixed partial prosthesises or ytzp or denture, partial, fixed
[Mesh]
y-tzp or
zirconium or
zirconia
4253 titles
344 abstract
69 full-text
3; no data o survival of FDPs
8; no detailed information on the FDPs 1; no statistical analysis
2; reporting on implant constructions 1; reporting on resin bonded FDPs 8; reporting on metal-ceramic FDPs 4; reporting on glass-infiltrated alumina-based ceramics
1; reporting on tooth-implant supported FDPs
36; reporting on tooth-supported FDPs
5 full-text on implant-supported
hand search from reference list studies 0
Final number of studies included 5
Fig 4. Search strategy
Block 1
(n=29,138) and (n=32,210) Block 2 = Total 11,273
Limit English: 11,237 Abstract available: 6,202 Jan 2000 to Oct 2013: 4,253