Jönkö
p
ing
Un
ivers
ity
,
Schoo
l
o
f
Hea
lth
and
We
l
fare
SHOULD
I
STAY
OR
SHOULD
I
GO
–
Factors
assoc
iated
w
ith
hosp
ita
l
izat
ion
r
isk
among
o
lder
persons
in
Sweden
Jenny
Ha
l
lgren
DISSERTATION SERIES NO. 70, 2016
©
Jenny Hallgren, 2016Publisher: School of Health and Welfare
Print: Ineko AB, Göteborg
ISSN 1654-3602
“Whatis ageing? HereI might betoo expansivein a biological and
philosophical way, asI say: What doeslife consist of besides ageing? Itis so
banal.If you cannot relatetothefactthat you are ageing, you cannot relate
tolife. Itis aform of ethics oflife,itisthe most essential, and you needto
talk aboutitin all ages”.
Abstract
Anincreasingly older population will mostlikelyleadto greater demands on
the health care system, as older age is associated with an increased risk of
having acute and chronic conditions. The number of diseases or disabilitiesis
notthe only marker ofthe amount of health care utilized, as persons may seek
hospitalization without a disease and/or illness that requires hospital health
care. Hospitalization may pose a severe risk to older persons, as exposureto
the hospital environment mayleadtoincreased risks ofiatrogenic disorders,
confusion, falls and nosocomial infections, i.e., disorders that may involve
unnecessary suffering andleadto serious consequences.
Aims: The overall aim of this thesis was to describe and explore individual
trajectories of cognitive development in relation to hospitalization and risk
factors for hospitalization among older persons living in different
accommodations in Sweden and to explore older persons´ reasons for being
transferredto a hospital.
Methods: The study designs were longitudinal, prospective and descriptive,
and both quantitative and qualitative methods were used. Specifically, latent
growth curve modelling was used to assess the association of cognitive
development with hospitalization. The Cox proportional hazards regression
model was used to analyse factors associated with hospitalization risk over
time. In addition, an explorative descriptive design was used to explore how
home health care patients experienced and perceived their decision to seek
hospital care.
Results: The most common reasons for hospitalization were cardiovascular
diseases, which caused morethan one-quarter of first hospitalizations among
the persons living in ordinary housing and nursing home residents (NHRs).
The persons who had been hospitalized had a lower mean level of cognitive
performance in general cognition, verbal, spatial/fluid, memory and
processing speed abilities comparedto those who had not been hospitalized.
Significantly steeper declines in general cognition, spatial/fluid and
processing speed abilities were observed among the persons who had been
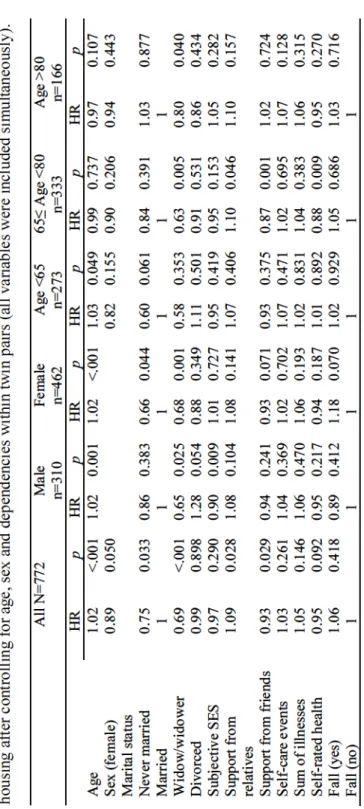
hospitalized. Cox proportional hazards regression analysis showed that the
assessed as malnourished accordingtothe Mini Nutritional Assessment scale
wererelatedto anincreased hospitalizationrisk amongthe NHRs. Amongthe
older persons living in ordinary housing, the risk factors for hospitalization
were relatedto marital status, i.e., unmarried persons and widows/widowers
had a decreased hospitalizationrisk.In addition, among socialfactors,receipt
of supportfromrelatives wasrelatedto anincreased hospitalizationrisk, while
receipt of supportfromfriends wasrelatedtoa decreasedrisk. The number of
illnesses was not associated withthe hospitalization risk for older personsin
any age group or forthose of either sex, when controlling for other variables.
The older persons who received home health care described different reasons
for their decisions to seek hospital care. The underlying theme of the home
health care patients’ perceptions oftheir transfer to a hospital involved trust
in hospitals. This trust was shared by the home health care patients, their
relatives andthe home health care staff, accordingtothe patients.
Conclusions: This thesis revealed that middle-aged and older persons who
had been hospitalized exhibited a steeper decline in cognition. Specifically,
spatial/fluid, processing speed, and general cognitive abilities were affected.
The steeper decline in cognition among those who had been hospitalized
remained even after controlling for comorbidities. The most common causes
of hospitalization amongthe older personslivingin ordinary housing andin
nursing homes were cardiovascular diseases, tumours and falls. Not only
health-related factors, such asthe number of diseases, number of drugs used,
and being assessed as malnourished, but also social factors and marital status
were related to the hospitalization risk among the older persons living in
ordinary housing and in nursing homes. Some risk factors associated with
hospitalization differed not only betweenthe men and women but also among
the different age groups. The information provided in this thesis could be
applied in care settings by professionals who interact with older persons
before they decide to seek hospital care. To meet the needs of an older
population, health care systems needto offerthe proper health care atthe most
appropriate level, and they need to increase integration and coordination
among health care delivered by different care services.
Keywords: Older persons, hospitalization,risk factors, cognitive decline,
qualitative content analyses,longitudinal, Cox regression,latent growth
Or
ig
ina
l
papers
Thethesisis based onthe following papers, which arereferredto bytheir
Roman numeralsinthetext:
Paper
I
Hallgren, J., Fransson, E.I., Reynolds, C.A., Finkel, D., Pedersen, N.L, &
Anna K. Dahl Aslan, A.K.(2016). Cognitivetrajectoriesinrelationto
hospitalisation among older Swedish adults. Submitted.
Paper
I
I
Hallgren, J., Ernsth Bravell, M., Mölstad, S., Östgren, C.J., Midlöv, P., &
Dahl Aslan, A.K. (2015). Factors associated withincreased hospitalization
risk among nursing home residentin Sweden: a prospective study with a
three-year follow-up. International Journal of OlderPeople Nursing.DOI:
10.1111/opn.12107.
Paper
I
I
I
Hallgren, J., Fransson, E.I., Kåreholt, I., Reynolds, C.A., Pedersen, N.L., &
Dahl Aslan, A.K. (2016). Factors associated with hospitalization risk among
communityliving older persons: resultsfromthe Swedish Adoption/Twin
Study of Aging (SATSA). Archives of Gerontology and Geriatrics,
(accepted for publication). DOI:10.1016/j.archger.2016.05.005.
Paper
IV
Hallgren, J., Ernsth Bravell, M., Dahl Aslan, A.K., & Josephson, I. (2015).
In Hospital We Trust: Experiences of older peoples’ decisionto seek
hospital care. Geriatric Nursing: 36(2015)306-311.DOI:
10.1016/j.gerinurse.2015.04.012
The articles have been reprinted withthe kind permission oftherespective
Contents
Abbreviations ...8
Preface ...9
Introduction...10
Background ...12
Ageing and health ...12
Biological ageing ...13
Cognitive ageing ...13
Illness and disease...14
Hospitalizations ...15
Riskfactorsfor hospitalization ...16
Hospitalization among older personsin Sweden ...18
Re-hospitalization...19
Negative outcomes associated with hospitalization ...19
Ambulatory care-sensitive conditions ...21
Swedish health and social care ...22
Andersen’s behavioural model of health care utilization ...27
The active ageing policy framework ...31
Rationale ...33
Aims ...35
Methods ...36
Design ...36
Studiesincludedinthe quantitative studies (I,II andIII) ...37
Measurements (studiesI,II, andIII)...42
Data analysis ...45
Ethical considerations ...48
Results ...50
Cognitive changein relationto hospitalization (studyI) ...50
Causes of hospitalization (studiesII andIII) ...54
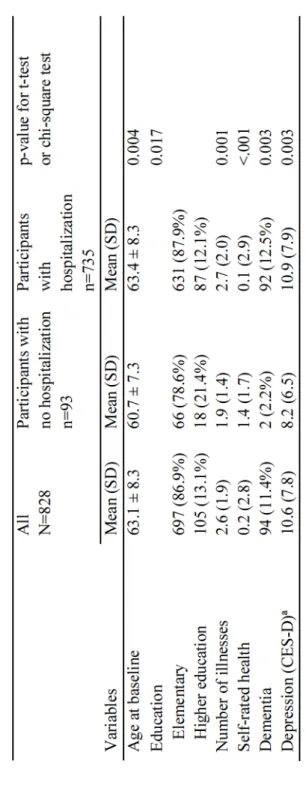
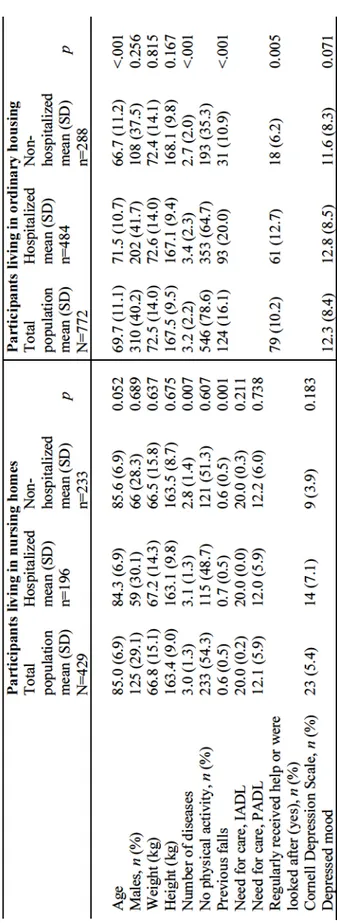
Baseline characteristics of hospitalized and non-hospitalized participants (studiesII andIII) ...56
Riskfactorsfor hospitalization (studiesII andIII) ...58
Reasonsfortransfer of older personsto a hospital (studyIV) ...63
Discussion ...66
General discussion ofthe results ...66
Methodological considerations ...78
Comprehensive understanding ...83
Conclusion ...86
Relevance andimplications ...87
Future research ...89
Svensk sammanfattning ...90
Acknowledgements ...93
Abbrev
iat
ions
ACSC Ambulatory Care Sensitive Conditions
ADL Activity of Daily Living
CES-D Center for Epidemiologic Studies Depression Scale
CHF Congestive Heart Failure
COPD Chronic obstructive pulmonary disease
ED Emergency Department
EU European Union
ICD-10 International Classification of Diseases and related Health
Problems 10thRevision
IPT In Person Testing
MMSE Mini-Mental Status Examination Test
MNA Mini Nutritional Assessment
NHR Nursing Home Residents
OECD Organization for Economic Co-operation and Development
RN Registered Nurse
SES Socio Economic Status
Preface
the physician asked mein one of hundreds
of medical consultationsthatI attended while working as a nursein a medical
wardin an acute hospitalin Sweden. I did not know, asit was not clearinthe
medicalrecord andthere were no obvious signs of any disease, whythe older
man had sought care atthe emergency department earlierthat morning. After
many hoursinthe emergency department waitingforthe physicianto examine
him,the old man was so exhaustedthat he hadlain down onthe bench beside
him. Routine bloodtests did reveal that his electrolyte status was not within
thereferencerange andthat some adjustmentsto his medications were needed,
as with many older persons. Duetothe generalstate ofthis manandthe
adjustmentsrequiredto his medications,the physicianthought thatit was best
to hospitalize him,justin case. Laterthat day, Itookthetimeto sit down and
talkto him properly. After a few minutes,it was clearto methatthe man was
not sure why he had sought care atthe emergency departmentthat day. He had
beencalling his primarycare, but the voice mail hadinformed him that he
wouldreceive a callfrom a nursethefollowing day. The old man did not want
to wait untilthe next day. He wantedto meet with health carestaff onthat day.
Duringthelast month, he had been feelingtired, hislegs had felt heavier, he
had experienced difficulty walking, and he had feltlonely.
The old man did not actually need hospital health care.If health care at alower
level had been available onthe same day,this man probably would not have
been hospitalized. Thisscenariois commonfor many people every day.
During mytime as a nurse at a hospitalin Sweden, I met many older persons
whoforsomereason had chosento seek hospital careinstead of care at alower
level or as a substitute for something else. These persons should have been
takencare ofata primarycare, municipalcare orsome othertype ofcare
facility,not inthe hospital setting. As a graduate student,I hadthe opportunity
to explore some areas within this research field. Do older persons who seek
hospital care have somethingin common?If we canidentify persons atrisk of
Introduct
ion
Rising life expectancy and an increasingly older population will most likely
leadto greater demands on health care systems, as older ageis associated with
anincreased risk of development of acute and chronic conditions. According
tothe Health and Medical Services Act 2§,
to provide good health and care on equal terms for the entire population,
giving priority to those most in need (SFS 1982:763). Coordinationand
continuity of health care can be difficultfor some older persons because many
ofthem meet with different care providers at differentlevels of care each year
(Modin & Furhoff, 2004). The most appropriate carelevelis not always clear
in each situation, and different carelevels have differentlevels of availability.
Today, a substantial number of older personslackthe knowledge, ability and
patienceto seek health care atthe appropriatelevel. Further, some carelevels
are not available during the evening, at night or on weekends. As a
consequence, older(and younger) personssometimesseekcareat andare
transferredto a hospital when alowerlevel of care would be preferable. Every
year, 1.4 million visits are madeto acute care providers or hospitalsin
Sweden,and one-third ofthese visitsare made by older persons (National
Board of Health and Welfare, 2015d). Many hospitalizations of older persons
are believedto be unnecessary, and/orthese persons could have beentreated
at alowerlevel of care (primary care and/or outpatient hospital care) (Berry
et al., 2011). Littleis known about why older persons aretransferredto
hospitals and whetherthere are certain older persons who are at a higher risk
of being hospitalized(Condelius, 2009). Hospitalization, which isthefocus of
thisthesis,is defined as staying at an acute hospitalfor one or more nights.
Hospitalization may pose a severe risk for older persons, as exposure to the
hospital environment mayleadtoincreasedrisks ofiatrogenic disorders,
confusion,falls and nosocomialinfections,i.e., eventsthat mayinvolve
unnecessary suffering andleadto serious consequences (Creditor, 1993;
Grabowski, Stewart, Broderick, & Coots, 2008; Intrator et al., 2007;
Ouslander et al., 2009). Alreadyin 1967, areport was publishedthat described
how physiological changes occurin healthy,ill orinjured persons who
undergo bedrest(Olson, 1990). However,the possible consequences affecting
different cognitive domains that occur several years after hospitalization are
hospitalizationiscostlyforsociety becausein-patientcareissignificantly
more expensivethan outpatient or primary care (Byrd, 2009). An investment
in increased care at a lower level would probably reduce overall
hospitalization costs(Intrator et al., 2007).Inthisthesis, persons 65 years and
above are referred to as older persons; well aware that it may differ
substantiallyin both physical and cognitive health, whetherthey are 65 or 85
years of age. Notably, this thesis should be interpreted on the basis of how
Background
Age
ing
and
hea
l
th
Worldwide population ageing, a high life expectancy, and declining fertility
areleadingto a significantincreaseinthe proportion ofthe populationthatis
overtheage of 65. Attheend of 2014in Sweden, one-fifth of thetotal
population wasabove 65 years ofage(SCB, 2016). Lifeexpectancy has
increased substantially duringthe second half ofthelast century, andin 2014,
the life expectancies of Swedish men and women were 80.1 and 84.0 years,
respectively (SCB, 2016). Although public health care in Sweden has
generally improved and disease onset often occurslater in life, many older
personslive for several years with disease. Thistrendis mainly explained by
reduced mortality from cardiovascular diseases (CVDs)
(Folkhälsomyndigheten, 2014).
Health is a multifaceted concept that includes different meanings and
dimensions. Health care, which should promote health, may beinfluenced by
an individual dimension, a societal dimension, i.e., the way society is
structured,andanenvironmental dimension,i.e.,the physical environment
affectingthe person (Naidoo & Wills, 2009). The World Health Organization
(WHO) defines healthas a state of complete physical, mental and social
well-being and not merelythe absence of disease orinfirmity (World Health
Organization, 1948). According to international human rights laws, all
persons,including old persons, havethe rightstolife andto health, as well as
to participate and maketheir own decisions abouttheir health based on
relevantinformation (United Nations Human Rights. General Assembly,
1966). Equal health care access should be a human right for all people of all
ages. Research that contributes toenabling all persons to receive equal and
appropriate health careis vital. Surprisingly,thereis no common definition of
,althoughthistermiscommonly usedin policy
practice as well asin research. The Organization for Economic Co-operation
and Development(OECD) defines healthy ageing as
personsin good health and keepingthem autonomous andindependent over
(Oxley, 2009), while The Swedish
NationalInstitute of Public Health(Swedish NationalInstitute of Public
physical, social and mental health to enable older persons to take part in
society without discrimination andto enjoy anindependent and good quality
. Although several studies have assessed healthy ageingin analyses of
health-related aspectsin older persons(Ennis et al., 2014; Simons, McCallum,
Friedlander, & Simons, 2000), some studies have arguedthatthe concept of
healthyageing may not beapplicabletothe oldest old persons (McKee &
Schüz, 2015) becauseitignoresthe physical realities of persons of advanced
age associated with biological ageing(Stephens, Breheny, & Mansvelt, 2015).
B
io
log
ica
l
age
ing
Thechangesthatinfluenceandconstituteageingarecomplex(Kirkwood,
2008). Biological ageing refers to the degree of age-associated decline
experienced by anindividual (Kaeberlein & Martin, 2015). As ageincreases,
numerous underlying physiological changes occur. From a biological
perspective, ageing is associated with a wide variety of cellular damage that
affects differentsystemsandtheirabilitiestofunction(Steves, Spector, &
Jackson, 2012; Vasto et al., 2010). Overtime,this damageleadsto a decrease
in physiologicalreserves and a general declinein health,leadingtoincreased
risks of many diseases. Forinstance,age-relatedlossesin motorfunction,
hearing and vision occur morefrequently withincreasing age(Cruz-Jentoft et
al., 2010; Hickenbotham, Roorda, Steinmaus, & Glasser, 2012; Yamasoba et
al., 2013). Diseases such as heart disease, stroke,respiratory disorders, cancer
and dementia are commonin old age. Further,the number of chronic diseases
is associated withincreased physical functioning difficultiesin persons of all
ages, and decreased physicalfunctioning has beenshownto be an early
marker of declining health (Guralnik et al., 2000). The combination of
different diseases,i.e., multi-morbidity, alsoimpacts physicalfunctioning and
isassociated withanincreasedrisk offrailty(Ernsth Bravell & Mölstad,
2010).
Cogn
i
t
ive
age
ing
Withincreasing age, a higher proportion ofindividuals exhibit cognitive
decline. The risk of decline in cognitionincreases with each decade over 60
thatisreached. However, manyindividuals do notshowcognitive decline
untilthelast years oflife, and some even show cognitive gains from midlife
functioning and are thus diagnosed with dementia (Schaie & Willis, 2016).
The mostcommon pattern ofcognitiveageingischaracterized by modest
declinesin most cognitive abilities startinginthe early 60s and continuingto
theearly 80s, when more marked decline occurs (Bosworth, Schaie Willis,
1999). However,there arelarge differences in cognitive performance and in
the rate of decline among individuals, and these difference seem to increase
in old age(Lövdén, Lindenberger, Schaefer, Bäckman, & Florian, 2010;
Steves et al., 2012). This variation in cognitive decline has also been shown
to beinfluenced by factors such as socioeconomic status,lifestyle and
medication use (World Health Organization, 2015), partly because many of
the mechanisms ofageingare random. However,this variationalso occurs
becausethesechangesarestronglyinfluenced bytheenvironmentand by
individuals behaviours. Loss of cognitive functioning may negatively affect
the self-care component of health care andthereforeincreasethelikelihood of
development of medical conditions. Lack of health-related behaviours, such
as medication adherence (Insel, Morrow, Brewer, & Figueredo, 2006), oral
hygiene maintenance (Wu, Plassman, Crout, & Liang, 2008) and avoidance
ofaccidentalfalls(Welmerink, Longstreth, Lyles, & Fitzpatrick, 2010),is
associated with a lower level of cognitive functioning and may increase the
need forformal health care.
I
l
lness
and
d
isease
Remaining healthyandavoidingchronic diseasesin oldageare desirable.
However,the number of diseases orlevel of disabilityis nota completely
accurate marker of quality of life and/or the amount of health care utilized.
Individualsseeking care may not alwaysrecognize whatis causingtheir
uneasiness. The abilityto distinguish between symptoms and signs,i.e., what
the care-seeking person describes andthe measurable or ocular signs of
illness,is vital (Ekman, 2014). Disease can occur without affecting a person
and withoutrequiring anytreatment. Likewise, a person may seek health care
and/or be hospitalized without having any disease and/orillness. Earlier
definitions ofillness were focused primarily on diseases,i.e.,
if and onlyif he or she has a disease whichis serious enoughto be disabling
(Boorse, 1977). However, more recent definitions are focused more on signs
and symptoms. Eisenberg and Kleinman define disease as n abnormalityin
andillness as
(Eisenberg & Kleinman, 2012). Theillness process begins with awareness of
a changeinthe body, and sometimesthe person cannottell what is wrong. The
(Kleinman,
Eisenberg, & Good, 2006).Illness and disease areimportant aspects affecting
health care utilization.
Hosp
i
ta
l
iza
t
ions
Hospitalization is common among older persons in Sweden and
internationally. Among older personsin general,the most common causes of
unplanned, i.e., non-elective, hospitalization, are cardiac insufficiency,
pneumoniaandchest pain(Table 1). The mostcommonreasonthat older
persons aged 65 years and above receive treatment for injury is due to falls
(44% of all admissions duetoinjury)(National Board of Health and Welfare,
2015c).
Table 1. The 10 most common causes of unplanned hospitalization among
persons aged 65 years and abovein Swedenin 2012(National Board of Health
and Welfare, 2013a).
Diagnoses Number of hospitalizations
Cardiacinsufficiency 21 543
Pneumonia 16 510
Chest pain 15 388
Atrialfibrillation and flutter 11 382
Cerebralinfarction 11 287
Chronic obstructive pulmonary disease 10 959
Bacterial pneumonia 9911
Acute sub-endocardialinfarction 9452
Atrialfibrillation 9418
R
isk
fac
tors
for
hosp
i
ta
l
iza
t
ion
Differentfactors have beenfoundto be associated with anincreased or
decreased hospitalization risk. Previous studies have reported that increased
age andthe male gender are risk factorsfor hospitalization (Dorr et al., 2006;
Ehlenbach et al., 2010). Previous hospital admissions (Landi et al., 2004) and
an increased number of contacts in outpatient care are associated with even
more hospital admissions (Condelius, Edberg, Jakobsson, & Hallberg, 2008).
Cognitive function (Dorr et al., 2006; Wilson et al., 2013) and comorbidity
(Dorr et al., 2006)increasethe hospitalization risk. Specifically,the presence
of one or more geriatric conditions (depressive symptoms, cognitive
impairment, falls, and urinary incontinence)is associated with an increased
number of hospitaladmissionsanda longerlength of hospitalstay(Wang,
Sheu, Shyu, Chang, & Li, 2014). As aresult of diseases, alarge proportion of
older personstake many prescribed drugs,as wellas manyinappropriate
drugs, which alsoleadsto anincreased hospitalization risk (Albert, Colombi,
& Hanlon, 2010; Klarin, Wimo, & Fastbom, 2005). Many older persons need
help withtheir medications. Lack of medication assistance among older
personsin need of medication supportis relatedto hospitalization (Kuzuya et
al., 2008). Further, polypharmacyisitself ariskfactorfor hospitalization, and
50% of medication-related hospitalizationsare believedto be preventable
(Jensen, Friedmann, Coleman, & Smiciklas-Wright, 2001; Mazzaglia et al.,
2007; Rogers et al., 2009). Previous studies have shownthatreduced physical
function(Carter, 2003; Grabowskietal., 2008),low physical performance
(Dorr et al., 2006; Li, Chu, Sheu, & Huang, 2011), and limitations in daily
livingactivities(Li, Chang, Wang, & Bai, 2011)affect hospitalizationand
care needs,suchasthoserelatedto pressure ulcersandfeedingtubeand
catheter use(Albertetal., 2010; Flaherty, PerryIII, Lynchard, & Morley,
2000; Fried & Mor, 1997; Horn, Buerhaus, Bergstrom, & Smout, 2005).
Different aspects of nutrition seemto haveimportantinfluences onthe
hospitalizationrisk. The use ofspecial dietsand weightloss increasethe
hospitalization risk (Jensen et al., 2001), as well asthe nutritional risk (poor
appetite and oral health problems) (Buys et al., 2014). Further, the presence
of obesity at 25 years of ageis predictive of avoidable hospitalizationinlater
life(Schafer & Ferraro, 2007). A Canadianstudy hasrevealedthat older
rate andthatthose who consume atleast one drink per week havethelowest
rate (Wilkins & Park, 1996).
Personalityis also associated with anincreasedlikelihood of emergency
department (ED) visits (B. Friedman, Veazie, Chapman, Manning, &
Duberstein, 2013), but no association with hospitalization has beenidentified
thusfar. Further, socialrelationships have beenfoundto not only decreasethe
hospitalization risk (Laditka & Laditka, 2003) but also to have heal
th-promoting effects(House, Landis, & Umberson, 1988). However,few studies
have examined experiences (Huckstadt, 2002).
During hospitalization, some people feel that they are left out, not provided
with information and given mixed messages(Dilworth, Higgins, & Parker,
2012). Others experience a sense of securityinthe hospital setting, meaning
thatthey feel safe being cared forin a hospital (Andersson, Burman, & Skär,
2011; Dilworth et al., 2012).
The hospitalizationrisk may differamong older personsliving in different
accommodations. Studies conductedinthe U.S. have demonstrated that
increasedage,reduced physicalfunction(Carter, 2003; Grabowskietal.,
2008)andcare needsareassociated withanincreased hospitalizationrisk
among nursing home residents (NHRs) (Albert et al., 2010; Flahertyetal.,
2000; Fried & Mor, 1997; Horn et al., 2005). In contrast, older persons who
livein ordinary housingin Sweden have similarlengths of hospital stays,take
similar amounts of drugs and have similar numbers of comorbidities but are
hospitalized morefrequentlycompared withthoselivingin nursing homes
(Condelius, 2009). Older personslivingin nursing homes are commonlythe
most diseased elderly, and accordingly, they have the highest need for care
(Grabowski et al., 2008). Hence,the disease burdenis nottheonly factorthat
influences whois hospitalized.
Livingarrangements mightinfluencetheassociations ofsomefactors with
hospitalization. For example,in several studies, a dementia diagnosis has been
shownto havea protectiveeffectagainst hospitalizationfor older persons
livingin nursing homes (Fried & Mor, 1997; Grabowski et al., 2008) and for
thoselivingin sheltered housing(Becker, Boaz, Andel, & DeMuth, 2012) but
notforthoselivingin ordinary housing(Dorr et al., 2006). Further, an
increased hospitalization risk has been reported among older persons
receiving home healthcare wholack medicationassistance(Kuzuyaetal.,
care aslowintensive comparedto hospital care (Fried, van Doorn, Tinetti, &
Drickamer, 1998), which might explain why one-third ofthese patients decide
totransfertoa hospital without prior medicalconsultation(Crossen-Sills,
Toomey, & Doherty, 2006).
Hosp
i
ta
l
iza
t
ion
among
o
lder
persons
in
Sweden
In Sweden, accessto hospital careis based on need, i.e., those mostin need
are prioritized. In addition, patients are only charged a nominal fee, sothere
are no economic barriersto seeking hospital care. Few studies have examined
hospitalization and predictors of hospitalizationin Sweden (Condelius et al.,
2008; National Board of Health and Welfare, 2014a). Studies conducted in
Sweden have suggestedthat among frail older persons orthose with complex
health problems, almost 40% are hospitalized atleast once each year(National
Board of Health and Welfare, 2014a). Further, older personslivingin ordinary
housing have anincreased number of hospital admissions comparedto NHRs
althoughthey are younger and havelessfunctional decline, which may
indicatethat hospital careis more accessibleto younger elderly and healthier
persons (Condelius, 2009). A study conducted in southern Sweden has
revealedthat a small group (15%) of older persons aged 65 years and above
has been admittedtothe hospitalthree or moretimes during one year,
accountingfor one-third ofthetotalin-patientcare. Additionally,alarge
proportion of hospitalized persons do notreceiveany municipal health or
service care; instead, they have increased contacts in outpatient care
(Condelius, 2009; Nägga, Dong, Marcusson, Skoglund, & Wressle, 2012).
The numbers of both diagnoses and physician contactsin outpatient care are
predictors ofthe number of admissions(Condelius et al., 2008). Some studies
have suggestedthat NHRs are frequently hospitalized (Kirsebom, Hedström,
Wadensten, & Pöder, 2014)andthatsome ofthese hospitalizationscan be
prevented (Kirsebom, 2015). However, the referral of NHRs with cognitive
Re-hosp
i
ta
l
iza
t
ion
A number of hospitalizationsleadtore-hospitalization,i.e., hospitalization
within 30 days after hospital discharge. As many as 30% ofre-hospitalizations
are believedto be preventable (Byrd, 2009). Congestive heart failure (CHF),
pneumonia (Jencks, Williams, & Coleman, 2009), and renal conditions
(Gabayanetal., 2015; Ouslanderetal., 2010),inadditionto stroke, hip
fractureandchronic obstructive pulmonary disease(COPD)(Bravata, Ho,
Meehan, Brass, & Concato, 2007; French, Bass, Bradham, Campbell, &
Rubenstein, 2008), arethe most common diagnoses associated with
re-hospitalization. According to patients, the reasons for re-hospitalization
include alack ofinformation or receipt of mixed messagesinthe hospital, as
well as disappointmentinthe health care system (Dilworth et al., 2012).
In Sweden, onereasonforre-hospitalization may bethat older patients seldom
participatein medical decision makingregarding discharge planning(Ekdahl,
Linderholm, Hellström, Andersson, & Friedrichsen, 2012). Thislack of
participation is particularly common when the health problems are not
pronounced and when no changesinthe medicationlist are needed. Because
the decisionto discharge a patientfromthe hospitalis made quickly and often
without patientinvolvement, a patients needs at home are not alwaysfulfilled
following discharge (Ekdahl et al., 2012). Many older persons admitted to a
hospital do not receive any health care or primary or municipal care services
(Swedish Association of Local Authorities and Regions, 2013), whichlimits
the opportunity to decrease the risk of re-hospitalization through preventive
actionsin existing home health care or home help services.
Nega
t
ive
ou
tcomes
assoc
ia
ted
w
i
th
hosp
i
ta
l
iza
t
ion
Hospitalization has been suggestedto be a majorriskfactorfor older persons.
Normal ageingis associated with declinesinthe muscles andlungs and
reduced bone density, among other consequences(Dehlin & Rundgren, 2014).
Hospitalization and bed rest may increasethe occurrence ofthese age-related
changes andleadtoirreversiblefunctional decline and a substantial andrapid
loss of muscle strength and endurance in the legs(Creditor, 1993;
Paddon-Jonesetal., 2006). Specifically, hospitalizationscanleadto a declinein
Capezuti, Shabbat, & Hall, 2010; Gill, Gahbauer, Han, & Allore, 2009;
Lafont, Gérard, Voisin, Pahor, & Vellas, 2011; Ouslander, Weinberg, &
Phillips, 2000). Some patients spend 80 % oftheirtimein bed during
hospitalization (Brown, Redden, Flood, & Allman, 2009), which is a major
reason for functional decline. A study conducted in the U.S. on 12 healthy
volunteers(mean age, 67 years) hasrevealedthat muscle mass, knee extension
strengthand muscle proteinsynthesis decrease by 6 %, 15 %and 30 %,
respectively, after 10 days of bedrest(Kortebein, Ferrando, Lombeida, Wolfe,
& Evans, 2007). Theseresultsshould be comparedtoresultsfrom communi
ty-dwelling older adults, wholose approximately 3-4 % of knee extension
strength each year(Goodpaster et al., 2006). These negative consequences are
oftentheresult of complications not relatedtothe cause of admission ortothe
specifictreatment. A recent European study has revealedthatthe presenting
conditionisthe cause of a declinein ADL during hospitalizationinlessthan
half of cases (Sourdet et al., 2015).
Functional decline during hospitalization has been found to decrease
functionalrecovery andincreasetherisks of morbidity and mortality (Boyd et
al., 2008). NHRs and older persons using home help services are at
particularly highrisks offunctional decline during hospitalization because
they are more often frail and have multi-morbidity (S. M. Friedman,
Mendelson, Bingham, & McCann, 2008). The declinein function after
hospitalizationincreases withincreasing age, polypharmacy, andthe presence
of multiple comorbidities, impaired cognition, delirium, and depression
(McCusker, Kakuma, & Abrahamowicz, 2002; Volpato et al., 2007). In
addition, deliriumisacommoncomplication of hospitaladmissionamong
older persons(Inouye, Schlesinger et al, 1999). The pathophysiology of
delirium is not clear but probably involves the influences of stressor events,
such as exposuretothe hospital environment, on a vulnerable patient group.
The hospitalenvironmentand particularlythe ED, whichis oftenthefirst
department visited byindividuals seeking hospital care, are often designedfor
the effective care of acutely ill individuals. However, this environment
unintentionally promotes the development of delirium. In addition, delirium
contributesto morbidity and mortality andis associated with anincreasedrisk
of developing dementia. However,thereasonfortheassociation between
delirium and dementiais not clear (Inouye, Schlesinger, & Lydon, 1999).
A further risk factor of hospitalizationisthe danger of developing a hospita
pneumoniaarethe mostcommon hospital-acquiredinfectionsin Swedish
hospitals. Accordingto one study,thelength of hospital stay istwice aslong
for patients with a hospital-acquiredinfection (National Board of Health and
Welfare, 2015b). No intervention aimed at reducing unnecessary
hospitalizations has achieved success thus far. Instead, studies have focused
onidentifying patients who can betreated at alowerlevel of care by
identifying diagnosesthatshould be handledinan outpatientsetting,i.e.,
ambulatory care-sensitive conditions (ACSCs), also termed avoidable
hospitalizations.
Ambu
la
tory
care-sens
i
t
ive
cond
i
t
ions
Avoidable hospitalizationsincludethose relatedto diagnosesthat should not
require hospital care, for example, anaemia, asthma, diabetes, CHF,
hypertension, angina pectoris and COPD. In Sweden in 2014, ACSCs
accounted for over 100 000 care days in hospitals; the most common
diagnoses were CHF, COPDand pyelonephritis(National Board of Health
and Welfare, 2014c)(Table 2).
Table 2. Number of avoidable hospitalizationsfor persons aged 65 and above
in Swedenin 2012(National Board of Health and Welfare, 2013a).
Diagnoses Number of hospitalizations
Congestive heartfailure 30 608
Chronic obstructive pulmonary disease 19 522
Pyelonephritis 19 031
Angina pectoris 13 024
Epileptic seizures 4859
Hypertension 3561
Diabetes 3340
Diarrhoea 3081
Ear, nose andthroatinfection 2213
Anaemia 2208
Asthma 1117
Gastric ulcer 1090
The ACSCrateis knownto be higher among persons aged 65 years and above.
International studies have reported that common reasons for avoidable
hospitalization are deficiency of andlack of continuityin primary care
(Cheng, Chen, & Hou, 2010; Menec, Sirski, Attawar, & Katz, 2006; Mytton
et al., 2012).
Inrecent years, criticism has arisenregardingthe content, meaning and choice
of diagnoses classified as ACSCs (Anell & Glenngård, 2014; Ljung, 2012).
Researchersand physiciansclaimthatitis difficult orevenimpossibleto
avoid hospitalizations related to ACSCs, and therefore, this classification is
not useful.In Sweden, ACSC diagnoses have beenrevised, andthey have been
reducedin number (National Board of Health and Welfare, 2014c).
Swed
ish
hea
l
th
and
soc
ia
l
care
To understand the findings of this thesis, it is necessary to understand how
health care, home help and social services are organized and providedto older
personsin Sweden.
The Swedish healthcaresystem wasconstructed to ensurethatallcitizens
receive healthcareaccordingtothe principles of human dignity, needand
solidarity,thatis,the personin greatest needis prioritized. Thestateis
responsible for overall health policy, andthe county councils are responsible
for most ofthe hospital care. The municipalities are responsible forthe care
and housing needs of older persons and of persons with disabilities(Anell,
Glenngard, & Merkur, 2012). Medical health care and home help services are
financed primarilythroughtaxation and areregulated bythe Health and
Medical Services Act (SFS 1982:763) and Social Services Act (SFS
2001:453).
Home
he
lp
and
home
hea
l
th
care
serv
ices
Accordingtothe Social Services Act (SFS 2001:453),the municipalities are
responsible for providing publically funded services and help to individuals
regardless of age, health and need of care. Home help services include care
and social services relatedto dailyliving, e.g., personal hygiene and physical
and social needs. Ofthe approximatelytwo million persons aged 65 and older
in Sweden, morethan 250 000(14%)eitherreceive home helpservicesin
those above 80 years of age is 38% (National Board of Health and Welfare,
2013b). Ifthe municipality cannot ensure for a reasonable standard ofliving
and carethrough home care and home health care services, a personis granted
nursing home placement (SFS 2001:453). Among persons aged 65 years and
above, approximately 5%livein nursing homes;the corresponding percentage
ofthoseaged 80 yearsandaboveis 14 %(Swedish Association of Local
Authorities and Regions, 2013).
Home health careincludes medicaltreatment and/orrehabilitation providedin
ordinary housingand in nursing homes. The majority of home healthcare,
long-term care and home help services are provided by staff representingthe
municipalities,andthe minority oftheseservicesare provided by private
providers. Most home healthcareis provided byaregistered nurse(RN).
However, in several municipalities, home health care tasks are delegated to
nurse assistants withless formal competence (SFS 1982:763). Older persons
receiving home help and home health care who live in their own homes can
taketheinitiativetocontacta hospital withoutconsulting withtheir home
health care providers.
Nurs
ing
home
care
Accessto nursing homesis based on needs assessment, with prioritization of
personsin greater need of care. Nursing homes provide basic health care under
the specificinstruction of primary care physicians, who serveas consultants,
as nursing homes do not have physicians stationed attheir facilities (National
Board of Healthand Welfare, 2005). Commonly, physiciansfrom primary
carefacilities visit nursing homes oncea weekand when needs arise. The
decision to transfer an individual from a nursing home to a hospitalis made
by the same consulting physician in agreement with the RN stationed at the
nursing home. As NHRsrepresentthe oldest,frailest, and most diseased group
ofthe elderly population,they frequently use health care services.
Inrecent decades,the number of bedsin nursing homes has decreased,
resultingina higher number of older personslivingin ordinary housing,
indicatingthatthe needfor home healthcareand home helpservices has
increased. Thistrendisinline withthe Swedish policystatingthat older
persons should be supportedinliving at homefor aslong as possible(Ministry
Pr
imary
ca
re
Primarycareand hospitalin-and outpatientcareare provided bycounty
councils and are also based on need. In total, 14 million visits were made to
physiciansat primarycarecentresin 2013,correspondingto 2.7 visits per
inhabitant (National Board of Health and Welfare, 2015d). From an
international perspective, this number is very low; the average stated in the
OECDistwice as high. Sweden has an overall high number of physicians, but
the proportion of physicians working in primary care is very low compared
with other Nordic countries (Sveriges Läkarförbund, 2014). Compared with
other European Union (EU) countries, Sweden is considered to have strong
primary care, meaningthatitis structured,i.e.,thereis an equal distribution
of primary care providers and population coverage for primary care services.
However, accessibility, e.g., the use of an appointment system, provision of
after-hours care, and continuity(doctor-patientrelationship), isratedlowerin
Sweden compared with most countriesinthe EU (Kringos, Boerma, van der
Zee, & Groenewegen, 2013). Normally, primary care centres are accessible
during business hours on weekdays. Duringtheeveningand on weekends,
thereis oftenthe opportunityto seek primary care emergency centres, buttheir
availabilities and accessibilities vary widely among different regions
(Sveriges Läkarförbund, 2014).
Inrecent years,the Act on System of Choice(SFS 2008:962) has been
implemented in the Swedish health care system, giving individuals the
freedomto choosefrom available providers. Afterthereform wasintroduced,
200 new primary care centres opened (National Board of Health and Welfare,
2015d). The National Audit Office has reported that individuals with minor
ailments have made more visitsto physicians afterthe care choicereform was
introduced, while frailer persons have made less visits. In addition, primary
carecentresinsocio-economically disadvantaged urbanareas havefewer
physicians compared with those in resource-rich areas (Riksrevisionsverket,
2014). Despitethereform,the number ofindividualsin permanentcontact
with a physician has notincreased (Riksrevisionsverket, 2014), althoughthe
Health and Medical Services Act 5 § claims that all citizens are entitled to
Hosp
i
ta
l
care
At the end ofthe 1960s, there were 120 000 hospital beds (15.3 beds/1000
inhabitants)in Sweden. Sincethen,the number of hospital beds has decreased
acrossthe country. Atthe beginning ofthe 1990s,
in which the responsibility for elderly carein Sweden was transferredto the
municipalities, was passed. This reform led to a reduction in the number of
hospital bedsto 50 000 because many ofthe departmentsthat had focused on
long-terminpatient health care, primarily for older persons, had closed. From
1999-2008,the percentage of hospital beds decreased by 21 %(National
Board of Healthand Welfare, 2010).In 2013, 25 000 hospital beds were
available, with 2.6 beds/1000inhabitants(National Board of Health and
Welfare, 2015d). The number of acute hospital bedsin Sweden is belowthe
averageinthe EU.
Thecurrent healthcaresystemsin many high-incomecountriesare better
equippedto handleacuteconditionsthanto manageand prevent chronic
conditionsthat are commonin old age(Patterson, 2014).In addition, specialist
care and hospital care often focus on one treatment at a time (Barnett et al.,
2012). The priorities of Swedish politics areto reducethelong waittimes for
diagnosis andtreatment andto decrease differencesin quality of care among
regionsandsocioeconomic groups(Anelletal., 2012).Inline with other
OECD countries,thelength of hospital stay hasfallenfrom 7 days on average,
as it was 10 years ago, to 5.5 days at present (OECD, 2013). This decrease
may partly be explained by not only better and more efficienttreatment
optionsthat do notrequire aslong of a hospital stay as before but also primary
careand municipal healthcarefacilitiesthat provideincreasedamounts of
curativetreatments and after-hours care.
Wa
i
t
ing
t
ime
in
the
emergency
depar
tmen
t
The number of visitstothe EDin Sweden hasincreasedinrecent years andis
currently approximately 2.5 million visits per year. Considerable successful
efforts have been madeinrecent yearsto decreasethe median waittimeinthe
ED (National Board of Health and Welfare, 2014d); however, this decrease
does notapplytoallage groups. For peopleaged 80 yearsand above,the
median wait time is even longer than before. A longer wait time affects the
aged 70 years and above who visitthe ED, 52% are hospitalized, and among
those aged 80 and above, 58 % are hospitalized(National Boardof Health and
Welfare, 2015d). Health problems,especiallyin oldage,are often mult
i-causal and complex. When older persons seekthe ED, physicians haveto be
awarethatthis patient group may have different needsthan younger patients
Andersens
behav
ioura
l
mode
l
of
hea
lth
care
ut
i
l
izat
ion
One ofthe most widely usedtheoreticalframeworksregarding healthcare
utilizationisthe behavioural model of healthcare utilization developed by
R.M. Andersen(Andersen, 1968), which has been usedinseveral studies
(Bass & Pracht, 2006; Bazargan, Bazargan, & Baker, 1998; Condelius, 2009;
B. Friedmanetal., 2013; Lehnertetal., 2011; Näggaetal., 2012; Stein,
Andersen, & Gelberg, 2007; Strain, 1991). The behavioural model (Figure 1)
utilization of health careis a human behaviourthatis
influenced by predisposing factors (socio-demographic factors), enabling
factors (factorsthat support or impede use), the need for health care (illness
level), and health behaviours (factors performed bytheindividual).
The behavioural model focuses on individual of health services
and on outcomesrelatedto health, satisfaction with health care, and quality of
life. The behavioural
utilization of health services during the late 1960s. The original theory was
thatindividual health care useis afunction of demographic, social and
economic characteristics of the family as a unit, and this model could both
predict and explain health care use (Andersen, 1995). Over time, the
behavioural model has been developed and nowalsoincludes contextual
determinants, such as health organization and community characteristics
Figure 1. Theconcepts ofthe behavioural model of healthcare utilization
(Andersen, 1995) (figure modified and drawn bythe author).
Env
ironmen
t
Hea
l
th
care
sys
tem
Andersen hasthoroughly reformulated and revisedthe original model (Aday,
1993; Andersen, 1995; Andersen et al., 2014; Andersen & Newman, 1973),
addingthe environment as a conceptthat affectsthe population characteristics
and outcomes of health care utilization. The environmentincludesthe health
care system, e.g., national health policy, as well as organization ofthe health
care system.
Popu
la
t
ion
charac
ter
is
t
ics
Pred
ispos
ing
charac
te
r
is
t
ics
Predisposing characteristicsrefertoindividualfactorsthat exist priortoillness
and affect hospitalization directly orindirectly. These characteristicsinclude
demographicfactors, such as age and sex, andsocialfactors, such as education
and occupation. Health beliefs,including knowledge, attitude and valuesthat
ofthe need for health care and health service use, are also considered
predisposing factors(Andersen, 1995).
Enab
l
ing
resources
Enabling resources make health services accessible to individuals. Enabling
factorsincludefinancingand organization. Financinginvolves incomeand
insurance, which affect individuals abilities to pay for health care services.
Healthcareservice organization describes whetheranindividualreceives
health care or home help. Socialrelationships also serve as an enablingfactor
that facilitates orimpedes health service use(Andersen 1995).
Need
charac
ter
is
t
ics
Needcharacteristicsareconsideredthe major determinants of healthcare
utilization. Need factors involve both perceived and evaluated health status.
Perceived needis a social phenomenonthatinvolves howindividualsrespond
totheir health problems and health conditions and howtheirresponsesleadto
decisionsregarding whethertoseek medicalcare. Evaluated need involves
healthcare professional judgements
needfor medical care (Andersen, 1968; Andersen & Newman, 1973).
Hea
l
th
behav
iours
Persona
l
hea
l
th
prac
t
ices
Personal health practices refer to activities performed by individuals
themselvesthatinfluences healthstatusandincludetobacco use, dietand
nutrition, exercise and care compliance.
Use
o
f
hea
l
th
serv
ices
According to the behavioural model, the use of health services includes the
numbers of hospitalizations and visits to primary care facilities or the
Ou
tcomes
Consumer
sa
t
is
fac
t
ion
In this model, outcome is defined as consumer satisfaction, and it are
concerned with how persons perceivetheirreceived healthcare. Customer
satisfactioninvolvestraveltime, waittime, communication with providers and
technical care received. Centraltothe behavioural model are feedbackloops,
which showthat outcomes affect predisposing factors,the perceived needfor
services, and health behaviours (Andersen, 1995).
Inthisthesis,the behavioural modelis usedto describe and understand how
predisposing, enabling and need characteristics, as well as health behaviours
andthe environment, arerelatedto hospitalization among older personsliving
The
act
ive
age
ing
po
l
icy
framework
Accordingtothe WHO, health and social care systems shouldfocus on health
promotion and disease prevention and promote accessto high-quality primary
andlong-term health carethatis accessible and agefriendly and addressesthe
needs of people as they age (World Health Organization, 2015). The active
ageing policy framework developed by the WHO in 2002 was meant to be
implementedin health policy documents worldwide. Active ageingis defined
as
securityin orderto enhance quality oflife and aimsto promote
healthyliving and quality oflife for all persons,including frail and disabled
persons and thosein need of help (World Health Organization, 2002).
Accordingtotheactiveageing policyframework, health policies needto
achieve a balance between support for self-care,informal support and formal
careincludedin healthandsocialservices. The WHO hassuggestedthat
health care professionals may need more knowledge and practice regarding
how to recognize older persons individual strengths and how to encourage
themto usetheirstrengthsto maintain independence, whichis particularly
important whentheir caretakers areill,frail or notfeeling well (World Health
Organization, 2015).Intheactiveageing policyframework,a number of
determinants, i.e., economic, behavioural, personal, social, health and social
services and the physical environment, have been suggested to be related to
andto promote active ageing(Figure 2). Moreresearchis warrantedto clarify
Figure 2. The concepts ofthe active ageing policy framework (WHO, 2002)
(figure constructed and drawn bythe author).
Active ageingis based onrecognition ofthe humanrights of older persons and
onthe United Nations Principles ofindependence, participation, dignity, care
and self-fulfilment (World Health Organization, 2015). Theterm active
ageing wasadopted bythe WHO duringthelate 1990sand was meantto
communicate a broader message compared with
recognizing factorsthat affect howindividuals and populations age (Kalache
& Kickbusch, 1997). Further, older ownthoughts,argumentsand
abilitiesto seek health care,including hospital care, areimportant knowledge
for promotingactiveageing. Theresults ofthisthesisattempt to provide
further understanding ofthefactorsassociated with hospitalizationandto
Rat
iona
le
As people age, physiological changes occurthat have physical and cognitive
effects. These physiological changes eventually lead to a general decline in
health and anincreasedrisk of development of disease. Alogical consequence
ofthese changes should bethatthose personsin greatest need of health care
receive the most appropriate care, sometimes including hospitalization.
However,the number of diseases or disabilitiesis notthe only marker ofthe
amount of healthcare utilized. Persons mayseek hospitalization withouta
disease and/orillnessthat requires hospital care.
Itis knownthat hospitalization mayresultin anincreasein age-related
changes and lead to irreversible functional decline. Few studies have
examined whether the decline in cognitive function is associated with
hospitalization and,if so, which cognitive domains are particularly affected.
In Sweden, there has been a decrease in the number of hospital beds, along
with a decreaseinthelength of hospital stay. In addition, Swedenisregarded
as havinglow accessibilityto and continuity of primary care compared with
other European countries, which may affect older persons health care
behaviours. Previousresearch hasrevealedfactorsthat arerelatedto and may
increasethe hospitalization risk among older personslivingin different
accommodations. Unfortunately,thisresearch was not conducted on Swedish
older persons, which limits the generalizability, recommendations and
subsequent implementation of the suggested interventions. The reason
underlyingthe needfor hospitalization may varyamong persons, andthe
reason for admissionis not always clear. Few studies have examinedthe risk
factors for hospitalization and how hospitalization affects older persons.
In this thesis, different aspects of hospitalization among Swedish older
persons are explored. Specifically, how development of cognition is
associated with hospitalization and what risk factors are related to
hospitalization among older persons living in differentaccommodations are
analysed,andthereasons why older personsaretransferredto a hospital
The knowledge generatedinthisthesis could be applicable for professionals
interacting with older persons whoare onthe verge ofseeking or needing
hospital care. Further,this knowledge could be usedto guidethe decisions of
A
ims
The overall aim of this thesis was to describe and explore individual
trajectories ofcognitive developmentinrelationto hospitalizationandrisk
factors for hospitalization among older persons living in different
accommodations in Sweden and to explore older persons´ reasons for being
transferredto a hospital.
The specific aims ofthe different studies were asfollows:
To examinethe developmentin cognitioninrelationto hospitalisation
among middle aged and older adults in a population-based
longitudinal study with upto 25 years offollow-up.
To evaluate physical and psychological factors associated with
hospitalizationrisk overtime among nursing home residents.
To describeandcompareindividualcharacteristics of hospitalized,
and non-hospitalized community-living older persons, and to
determine factorsthat affect hospitalization risk overtime.
To explore how older people with a variety of health problems
experience and perceive decisionto seek hospital care whilereceiving
Methods
Des
ign
Inthisthesis, different designs were usedinthefourincludedstudies. An
overview ofeach designis presentedin Table 3. Thestudy designs were
longitudinal, prospective and descriptive, and both quantitative (studies I, II,
and III) and qualitative (study IV) methods were used.
Long
i
tud
ina
l
and
prospec
t
ive
des
igns
(s
tud
ies
I
,
I
I
,
I
I
I)
A longitudinal design can be applied when studying changes over time, and
this approach uses data collected at morethantwotime points(Kazdin, 2002;
Polit & Beck, 2014).In studyI, alongitudinal design was used, with collection
of data on cognitive abilities at upto 8 differenttime points. In studies II and
III, a prospective design was used. A prospective design measures the
presumed future effects of a certain cause. The advantage of using a
prospective design ratherthan a cross-sectional designisthat itis possibleto
establish atime relation between exposure and outcome. In studies II and III,
factors associated with hospitalization risk over time were analysed by
comparing participants who did and did not experience hospitalization.
Exp
lora
t
ive
descr
ip
t
ive
des
ign
(s
tudy
IV
)
In study IV, an explorative descriptive design was usedto examine how older
personsreceiving home health care experience and perceivetheir decisionsto
seek hospital care. An explorative designis used when a phenomenon is not
well understood and whenthe design can shedlight on underlying processes
Table 3. Overview ofthe four different studies.
Study Design Sample Data collection Data analyses
I Longitudinal
Quantitative 828olde mr peiddrsonsle-agedin and
varied housing
In-persontesting,
Registers Lacurvetent ana growlysesth
II Prospective
Quantitative 429residen nursts ing home JournaIn-personls testing, Coxhazards propo modertionall
III Prospective
Quantitative 772olde mr peiddrsonsle-agedin and
ordinary housing
Self-reported
questionnaires,
Registers
Cox proportional
hazards model
IV Descriptive
Qualitative 22pat homeients health care Indintervividuaiewsl Quaconltenitattive analyses
S
tud
ies
inc
luded
in
the
quan
t
i
ta
t
ive
s
tud
ies
(
I
,
I
I
and
I
I
I)
Thisthesisincludestwolongitudinalstudies, The Swedish Adoption/Twin
Study of Ageing(SATSA)and The Study of Healthand Drugsin Elderly
Livingin Institutions (SHADES).
The
Swed
ish
Adop
t
ion
/Tw
in
S
tudy
o
f
Age
ing
(SATSA)
SATSAis a population-basedlongitudinal study. The participantsin SATSA
were drawnfromthe Swedish Twin Registries(STR)(Lichtenstein, Floderus,
Svartengren, Svedberg, & Pedersen, 2002) andincluded same-sex twin pairs
reared both together and apart. In brief, SATSA was initiated in 1984 when
thefirst questionnaire (Q1) was sent outto a sub-sample ofthe STR, withthe
aim of studying the aetiology of individual differences in ageing (Finkel &
Pedersen, 2004). The responserate for Q1 was 70.7%.In 1986,twin pairs
aged 50 years and above who bothresponded and participatedin Q1(N=2072)
were invited to participate in in-person testing (IPT), which included
the first IPT. Sincethen,twins who participatedin Q1turning 50 have been
askedto participatein IPTs upto IPT5. Intotal, 859individuals have
participatedin atleast one IPT, and 2211 have completed atleast one
questionnaire(Figure 3). TheIPTs were conducted bytrainedresearch nurses
at primarycarefacilitieslocatedclosetothe participants homes orinthe
own homes.
Figure 3. Overview of SATSA.
The S
tudy o
f Hea
l
th and Drugs
in E
lder
ly L
iv
ing
in
Ins
t
i
tu
t
ions
(SHADES)
SHADESis alongitudinal study conducted from 2008-2010. Eleven nursing
homes in three different municipalities in Sweden participated in this study.
The original aim of SHADES was to study mortality, morbidity, nutritional
status,and pharmaceutical treatment among older NHRs(Ernsth Bravellet
al., 2011). The participating nursing homesincluded 30 general departments
andten departmentsfocused on dementiacare. Allresidentslivinginthe
participating nursing homes wereinvitedto participatein SHADES. Among
theinvited persons (N=443), 89 residents ortheir relatives did choose notto
participate, and 49 were excluded dueto severeillness or palliative care. An
additional 11 persons were excluded due to language problems and hearing
difficulties,and 5 wereexcludedforan unknownreason. During thetime
betweenthe provision of consent bytheresidents andthe start ofthe study, 18
persons died. Atotal of 268 NHRs participatedinthe first assessment
(participation rate, 61%). The participants were examined every six months
s of drugs used, biomarkers, and social visits
andstafflevelsatthe various nursing homes. Participants who endedtheir
participation duringthe study either dueto death(n=193), migration(n=7), or
refusal (n=4) were replaced by new residents enteringthe nursing home who
provided consent (Figure 4). Intotal, 429 persons participated in atleast one
assessment wave.
Figure 4. Overview of SHADES.
Par
t
ic
ipan
ts
and
da
ta
co
l
lec
t
ion
An overview ofthe participantsincludedin studies I-IVis shownin Table 4.
Table 4. Participantsin studies I-IV.
Study Total N Mean age at
baseline (range) Gender(female) Housing
I 828 63.1 (50-86) 59.3 % Ordinary housing
and nursing home
II 429 85.0 (65-101) 70.9 % Nursing home
III 772 69.7 (46-103) 59.8% Ordinary housing
IV 22 83.1 (66-93) 68.2 % Ordinary housing
with home health
S
tudy
I
In study I,twins who had participatedin atleast one IPT wave from IPT1-8
in SATSA wereincluded. Participants who did not have completedata on all
four cognitive domains assessed (i.e., memory, verbal, spatial/fluid and
processing speed abilities) were excluded (n = 31), and atotal of 828
participants were ultimately included in the study. The exclusion of
participants was performedto ensurethatthe same sample size (N) was used
and the same individuals were assessed in all analyses. Data on
hospitalizations werecollectedfromthe NationalIn-patient Register. The
participants first hospitalizations after their inclusionin SATSA, regardless
ofthecause, wereincluded. Twins with hospitaladmissions beforetheir
inclusionin SATSA, but not after or duringtheir participation, wereregarded
as having no hospital admission. Of 828twins, 735 had atleast one hospital
admission duringtheir participationin SATSA.
S
tudy
I
I
Study IIincluded atotal of 429 participants (70.9 % women; mean age, 85.0
years) from SHADES. Data were collected by trained research nurses inthe
stated nursing homes. The participants psychological and physical statuses
were assessed using standardized procedures and well-established tests and
scalesand were based oninformation obtained usingcaregivers as proxy
drugs was collected fromthe hospital medical records. In addition,the
research nurses measured s and heights and collected
bloodsamples(Ernsth Bravelletal., 2011). Theresearch nursesextracted
hospitalization dates and reasons for hospitalization during the study period
from the nurses documentation at the nursing homes and from the hospital
medical records.
S
tudy
I
I
I
Thefifth questionnaire(Q5)in SATSAthat was sent outin 2003 (N=794) was
usedasthe baselineforstudyIII. All participants werelivingin ordinary
housing (N=772). Participantslivingininstitutions were excludedto obtain a
more homogeneoussample. Q5 containeditems about health,social and
psychological factors. The study sample was created bylinking the datafrom