MALMÖ UNIVERSITY isbn 978-91-7104-403-7 (print) isbn 978-91-7104-404-4 (pdf) issn 0348-6672 LILLEMOR DIMBER G MALMÖ UNIVERSIT SWEDISH DENT AL JOURN AL, SUPPLEMENT 237 , 20 1 5. DOCT OR AL DISSERT A TION IN ODONT OL OG Y
LILLEMOR DIMBERG
MALOCCLUSIONS
AND QUALITY OF LIFE
Cross-sectional and longitudinal studies in children
Swedish Dental Journal, Supplement 237, 2015
MAL OCCLUSIONS AND QU ALIT Y OF LIFE
Swedish Dental Journal Supplement 237, 2015
© Copyright Lillemor Dimberg 2015
Illustrations: Lillemor Dimberg and Sam Guggenheimer ISBN 978-91-7104-403-7 (print)
ISBN 978-91-7104-404-4 (pdf) ISSN 0348-6672
LILLEMOR DIMBERG
MALOCCLUSIONS AND
QUALITY OF LIFE
Cross-sectional and longitudinal studies in children
Malmö högskola, 2015
Odontologiska fakulteten
Publikationen finns även elektroniskt, se www.mah.se/muep
INNEHÅLL
PREFACE ... 9 ABSTRACT ... 10 Paper I ...11 Paper II ...11 Paper III ...12 Paper IV ...13 Paper V ...13 POPULÄRVETENSKAPLIG SAMMANFATTNING ... 14 INTRODUCTION ... 16 Malocclusion ...16 Quality of life ...19 Significance ...20 AIMS ... 22 Paper I ...22 Paper II ...22 Paper III ...22 Paper IV ...23 Paper V ...23 HYPOTHESES ... 24 Paper I ...24 Paper II ...24 Paper III ...24 Paper IV ...24 Paper V ...24MATERIALS AND METHODS ... 25
SUBJECTS ...25
METHODS ...28
Papers I – III ...28
In Paper III, following variables were also registered ...30
New registrations reported in the frame story ...30
Paper IV – systematic review ...31
Paper V ...33
RESULTS ... 37
General results ...37
Cross-sectional and longitudinal studies on malocclusion (Paper I-III) ...38
Systematic review (Paper IV) ...44
Impact of malocclusions on oral health related quality of life (OHRQoL) - (Paper V) ...48
DISCUSSION ... 52
Methodological aspects ...52
Prevalence and change in malocclusions ...56
Influence of sucking habits on the prevalence of malocclusions ...57
Influence of breathing disturbances and allergies on the prevalence of malocclusions ...58
Orthodontic treatment need ...59
OHRQoL in children and adolescents ...59
Research on children – ethical aspects ...60
Future research ...62
CONCLUSIONS ... 63
ACKNOWLEDGEMENTS ... 65
REFERENCES ... 68
PREFACE
This thesis is based on the following papers, which are referred to in the text by their Roman numerals I-V:
I. Dimberg L, Bondemark L, Söderfeldt B, Lennartsson B. Prevalence of malocclusion traits and sucking habits among 3-year old children. Swed Dent J 2010;34:35-42.
II. Dimberg L, Lennartsson B, Söderfeldt B, Bondemark L. Malocclusions in children at 3 and 7 years of age: a longitudinal study. Eur J Orthod 2013;35:131-37.
III. Dimberg L, Lennartsson B, Arnrup K, Bondemark L. Prevalence and change of malocclusions from primary to early permanent dentition – a longitudinal study. Accepted for publication in Angle Orthodontist.
IV. Dimberg L, Arnrup K, Bondemark L. The impact of malocclusion on the quality of life among children and adolescents: a systematic review of quantitative studies. Eur J Orthod 2014; doi:10.1093/ejo/cju046
V. Dimberg L, Lennartsson B, Bondemark L, Arnrup K. Oral health related quality of life among children – The impact from malocclusions. Submitted.
The papers are reprinted with kind permission from the copyright holders.
ABSTRACT
There are few longitudinal studies of the prevalence of malocclusions and possible self-correction of malocclusions during the development of the dentition. Early intervention might be unnecessary if self-correction of the malocclusion occurs during the transition from the primary to the permanent dentition. Most studies are cross-sectional and in those of longitudinal design, the results are inconsistent and difficult to interpret.
Malocclusions may or may not influence the quality of life in children and adolescents. Thus, evaluations of the influence of different malocclusions on quality of life will certainly underpin a broader understanding and knowledge about how malocclusions affect the daily life of young patients. This information may also be important when it comes to assessing the most appropriate time for starting orthodontic treatment, not only from a professional point of view, but also, most importantly, from the patients’ perspective.
The overall aim of this thesis was therefore to evaluate the prevalence of malocclusions, and to document changes occurring during the development of the dentition, from the primary dentition stage at age 3, through the mixed dentition at age 7, to the early permanent dentition at age 11.5 years. Further aims were to review the current state of knowledge about the impact of malocclusions on oral health related quality of life (OHRQoL) and to investigate how malocclusions affect the quality of life in a cohort of children, aged 11.5 years, whose dental care is provided by the Swedish Public Dental Service.
The thesis is based on five studies:
Papers I-III are cross-sectional and longitudinal studies with a
prospective study design following a cohort of children from 3 to 11.5 years of age. The prevalence and change of malocclusions was evaluated on both individual and group level. Possible environmental etiologic factors for development of malocclusions e.g. sucking habits, breathing disturbances and allergies were evaluated.
Paper IV comprises a systematic review of the scientific literature
investigating the influence of malocclusions on OHRQoL. Five databases were used and the literature search spanned from January 1960 to January 2014 and was subsequently expanded in the frame story of this thesis to September 2014.
Paper V assesses OHRQoL in a cohort of children whose dental
care is provided by the Swedish Public Dental Service. OHRQoL was assessed by means of the Child Perceptions Questionnaire 11-14 Impact Short Form (CPQ11–14–ISF:16) with special reference to the impact from malocclusions or orthodontic treatment need.
These five studies led to the following conclusions:
Paper I
• At 3 years of age the prevalence of one or more malocclusions was 70%: the most common were anterior open bite (50%), Class II relationship (26%), increased overjet (23%) and posterior crossbite (19%). Sucking habits were very prevalent; more malocclusions were attributable to dummy sucking than to finger/thumb sucking.
Paper II
• Between the ages of 3 and 7 years, the overall prevalence of malocclusion decreased significantly, from 70 to 58 %. This decrease was attributable primarily to self-correction of anterior open bite, excessive overjet and Class III malocclusion.
• Although high rates of self-correction were also recorded for deep bite, Class II malocclusion and posterior or anterior crossbite, new malocclusions developed at almost the same rates, resulting in unchanged prevalence at the end of the observation period, at 7 years of age.
• There was a significant association between sucking habits and anterior open bite and posterior crossbite at 7 years of age. • Self-correction of anterior open bite and excessive overjet
was less frequent among thumb or finger suckers than among dummy suckers, seen at 7 years of age.
• Allergy, breathing disturbances and snoring had potentially negative effects on the occlusion at 7 years of age.
• The results clearly support clinical guidelines recommending deferral of orthodontic treatment of malocclusion diagnosed in the primary dentition until transition to the mixed dentition stage.
Paper III
• The prevalence of malocclusions at 3 and 11.5 years of age was similar.
• Deep bite, contact point displacement and spacing were the malocclusions most commonly emerging from primary to early permanent dentition.
• Gingival or palatal trauma was recorded in 12% of children with deep bites at 11.5 years of age.
• Children at 11.5 years of age exhibiting a combination of overjet >4mm and incomplete lip closure had a 3.1 times greater risk of dental trauma than those with normal lip closure.
• Orthodontic treatment need, at age 11.5 years, was severe or extreme in 22.0%, moderate or borderline in 23.5% and minor to negligible in 54.5%.
• Habits and allergies found at 3 years of age had no associations with malocclusions at 11.5 years of age.
Paper IV
The systematic review disclosed that:
• There is strong scientific evidence that malocclusions in the aesthetic zone have negative effects on OHRQoL, predominantly on emotional and social well-being.
Paper V
In the evaluation of the impact of malocclusions or orthodontic treatment need on oral health related quality of life (OHRQoL) in the Swedish cohort, it was concluded that:
• The OHRQoL of the cohort was good.
• The effect of malocclusions or orthodontic treatment need on OHRQoL was limited and inconsistent.
• Dental fear and headache emerged as more distinct impact factors on OHRQoL than malocclusions or orthodontic treatment need.
Key conclusions and clinical implications:
At group level the prevalence of malocclusions may seem to be constant. Nonetheless, following the same individuals over time clearly shows that changes occur at the individual level. As self-correction occurs frequently, any orthodontic treatment should be postponed until at least the mixed dentition stage.
The clinician should also be aware of that in children with visible malocclusions the malocclusions often have negative effects on children’s quality of life. In addition, dental fear or headache at the end of childhood may have a greater impact on the OHRQoL than malocclusions or orthodontic treatment need. This should be taken into account in determining the most propitious time to begin orthodontic treatment.
POPULÄRVETENSKAPLIG
SAMMANFATTNING
Denna avhandling presenterar en unik longitudinell studie av förekomsten av bettavvikelser och förändringar av bettavvikelser som uppträder från mjölktandsbettet genom växelbettsperioden ända fram till det unga permanenta bettet. En grupp bestående av 277 barn från Örebro läns landsting undersöktes och följdes kliniskt från 3 års ålder tills dess de var i genomsnitt 11.5 år. Barnen fick också vid 11.5 års ålder besvara en enkät om munhälsorelaterad livskvalitet.
Bland de viktigaste resultaten var att medan den totala förekomsten av bettavvikelser var oförändrad i mjölktandsbettet respektive det unga permanenta bettet så inträffade flera förändringar under denna period på individnivå. Korrigering av bettavvikelser utan behandling s.k. självkorrigering var vanligt förekommande i alla bettavvikelser, men nya bettavvikelser utvecklades också, i vissa fall i lika stor omfattning. Således var den totala förekomsten av bettavvikelser oförändrad. Ytterligare en viktig slutsats var att barn med stora överbett och utan läppslutning om tänderna löpte 3 gånger ökad risk att råka ut för tandskador.
Efter en systematisk genomgång av litteraturen kunde konstateras att det finns starka vetenskapliga bevis för att synliga bettavvikelser har negativa effekter på munhälsorelaterad livskvalitet, särskilt känslomässigt och socialt.
Vidare visade en studie på en grupp barn inom den svenska tandvården att den munhälsorelaterade livskvaliteten var hög och effekten av bettavvikelser eller objektivt tandregleringsbehov på den munhälsorelaterade livskvaliteten var begränsad och inkonsekvent.
Ett viktigt fynd var att tandvårdsrädsla och huvudvärk visade sig ha en tydligare effekt på munhälsorelaterad livskvalitet än vad bettavvikelser eller objektivt behov av tandregleringsbehandling hade. Den övergripande slutsatsen blir därför att bettavvikelser har negativ inverkan på den munhälsorelaterade livskvaliteten men att resultaten tyder på en komplex effekt. Således behövs fler studier inom detta område.
Klinisk betydelse:
Förekomsten av bettavvikelser hos en grupp barn kan förefalla vara konstant vid två olika tidpunkter. Följer man dock samma individer över tid blir det tydligt att förändringar sker på individnivå. Då självkorrigering av bettavvikelser är vanligt förekommande bör all tandreglering skjutas upp åtminstone till växelbettsperioden.
Tandläkaren bör också vara medveten om att på barn med synliga bettavvikelser har bettavvikelserna ofta negativa effekter på barnens livskvalitet. Dessutom kan tandvårdsrädsla eller huvudvärk i slutet av barndomen ha större inverkan på den munhälsorelaterade livskvaliteten än bettavvikelser och objektivt tandregleringsbehov. Detta bör beaktas vid val av tidpunkt för tandregleringsbehandling.
INTRODUCTION
Malocclusion
Normal or ideal occlusion is a concept constructed by the orthodontic profession. In the 1890’s Edward H Angle introduced the first clear and simple definition of normal occlusion for the permanent dentition:
“The upper first molars are the key to occlusion and the upper and lower molars should be related so that the mesiobuccal cusp of the upper molar occludes in the buccal grove of the lower molar. If the teeth are arranged on a smoothly curving line of oc-clusion and this molar relationship exists, then normal ococ-clusion
would result”.1
The opposite condition is malocclusion and was once defined:
“The nature of malocclusion, not a disease but, rather a variation from accepted societal norm that can lead to functional
difficul-ties or concerns about dento-facial appearance for a patient”.2
Occlusion is evaluated in terms of sagittal, vertical, and transverse relationships between the maxillary and mandibular dental arches, displacement of teeth, crowding and spacing. Some malocclusions e.g. overjet are classified as a range. This implies that normal occlusion may have minor variations (within a range) and is not a fixed value. Subsequently, methods for registration of malocclusions in epidemiological studies were developed for both the primary and the permanent dentitions.3, 4
Etiology
The etiology of different malocclusions is complex and varied, and includes specific causes, hereditary and environmental factors. Specific causes can be disturbances in the embryological process which can result in cleft lip or palate or other cranio-facial defects.5A relatively
high heritability of craniofacial dimensions and low heritability of dental arch variations has been described5, 6, but it is still unclear how
this relates to the development of malocclusions which have both skeletal and dental components.5, 7
Heredity is reported to have a stronger influence on mandibular prognathism or posterior rotation of the mandible and large anterior face height, described as a long face pattern.5 Environmental factors
such as sucking habits have been associated with anterior open bite and posterior crossbite.8 Mouth breathing, due to allergies, hypertrophic
adenoids, and/or enlarged tonsils has been associated with posterior crossbite, anterior open bite, posterior rotation of the mandible and large anterior face height.9, 10 Snoring and nocturnal breathing
disturbances may also have negative effects on the occlusion, as they also lead to mouth breathing and depression of the tongue during sleep.9, 11-13 Thus, not only hereditary factors but also environmental
components have the potential to impact on the developing dentition. Because of this complex developmental pattern, it is difficult not only to predict the development of a malocclusion, but also to prevent its development.
Prevalence and treatment need
There is a wide range of reported prevalence of malocclusions: 39-93%.14-19 This reflects variations in study populations with
respect to ethnicity and age and also lack of conformity of methods of registration. There are striking differences between ethnic groups with respect to the prevalence of specific malocclusions. In Northern European populations, postnormal (Class II) malocclusions are much more prevalent than prenormal (Class III malocclusion), whereas Asian populations, Class III malocclusions are more frequent than Class II malocclusions.20 Anterior open bite, a vertical relationship, is
more prevalent in African than in European populations.20 Age also
has an impact on the prevalence of different malocclusions. In early childhood, malocclusions are commonly related to sucking habits,
anterior open bite and posterior cross bites, while in school-age children, crowding and displacement of teeth are more prevalent.17,
21, 22 Finally, variations in criteria for determining malocclusions may
influence the prevalence, because some conditions such as overbite and overjet are defined within different ranges.
Deviation from normal or ideal occlusion does not necessarily mean that the malocclusion needs to be treated. Assessment of treatment need is based on an evaluation of the risk, in the short or long term, for (increasing) disturbances in oral health, function, esthetics or patient dissatisfaction.
Effective use of resources for orthodontic care demands careful selection of patients, prioritizing treatment need. In this context, treatment need indices may be helpful. Although several indices have been developed,2, 23, 24 to date none is considered sufficiently
validated. However, these indices are currently the best tools available. A major drawback is that the patient’s perspective is not properly considered.25 Traditionally this has not been questioned, but
in future it is likely that the patient’s perception will be included in the evaluation of orthodontic treatment need and that the orthodontist will also consider the impact of the malocclusion and the predicted treatment outcome on oral health related quality of life (OHRQoL).
Development of malocclusion and treatment timing
The timing of treatment is an important determinant of successful outcome. Interceptive orthodontics may prevent malocclusions from increasing in severity and also improve the stability of the treatment outcome. One example is early treatment of posterior crossbite. If left untreated, it may result in asymmetries during development and growth.26, 27 However, studies have revealed that self-correction may
occur during the transition from the primary to the early mixed dention28, 29 and therefore early intervention would be unnecessary.
Studies on the development of normal occlusion have contributed to our understanding of the normal pattern of development21, 30 but
the factors underlying the development of a malocclusion in the primary dentition are poorly understood. Changes in malocclusion between the primary and permanent dentition have been shown in earlier studies but the direction of change could not be predicted.31, 32 Subsequently, as described above, self-correction of malocclusion
has been reported for posterior crossbite and anterior open bites, but at what age and to what extent this occurs is not fully understood.19,
28, 29, 33, 34 Other studies have revealed that excessive overjet and
Class II malocclusion do not self-correct.35 Most previous studies
on the prevalence of malocclusions are cross-sectional and, preclude assessment of stability or changes to individual malocclusions. An understanding of this aspect of malocclusion is of great importance to the clinician, in selecting the most propitious time for treatment of different malocclusions.
Quality of life
According to The World Health Organization (WHO) health is “A state of complete physical, mental and social well-being, and not merely the absence of disease and infirmity”.36 In the field of
dentistry this means that good oral health not only include absence of caries or periodontal disease but also the patient’s mental and social well-being.37
Health or oral health and quality of life (QoL)/oral health related quality of life (OHRQoL) are broad terms and are linked with happiness and satisfaction with life. A major challenge in measuring QoL/ OHRQoL is that the term has different meanings within different contexts.
Malocclusions and consequences for quality of life
Self-perception of a malocclusion may not always be in accordance with objective assessment of the severity of the condition according to an orthodontic treatment need index. Therefore, when evaluating the individual need for treatment it may be equally important to consider what impact the malocclusion can have on self-perceived OHRQoL. Malocclusions in the aesthetic zone (for example excessive overjet with incomplete lip closure, crowded incisors, large diastema between incisors) have been associated with bullying and lower self-esteem among teenage children.38-40 It is also known that excessive overjet
with incomplete lip closure is associated with a higher prevalence of dental trauma to the upper incisors.25 Untreated posterior crossbite
can cause facial asymmetries and may have an impact on quality of life, with respect to both functional and esthetical aspect.27 Moreover,
malocclusion/orthodontic treatment need and OHRQoL;41 another
systematic review has shown medium to high levels of evidence of an association between posterior crossbite and temporomandibular symptomatology.26
Measuring oral health related quality of life (OHRQoL)
Several quantitative measures have been developed to assess OHRQoL. Most are intended for use in an adult population.42, 43
However, the Child Perception Questionnaire (CPQ11-14) has been designed for self-assessment of OHRQoL among children and adolescents in the age span 11-14 years.44 The original questionnaire
consists of 37 items organized into four subscales; oral symptoms, functional limitations, emotional well-being and social well-being. The reliability and validity of CPQ11-14 has been evaluated in different child populations and it has been translated into Swedish according to a process called “linguistic validation” recommended by Mapi research institute in Lyon, France. The Swedish version of CPQ11-14 was evaluated in a master’s thesis and, was found to be both valid and reliable and seems to be an appropriate instrument for measuring OHRQoL in Swedish children aged 11-14 years.45
Subsequently, the developers Jokovic et al46 introduced shorter
versions of the CPQ11-14, comprising8 and 16 items respectively. A comparative study showed that the psychometric values of the 16 item-version were in good agreement with the long version.47
Significance
There are few longitudinal studies of the prevalence of malocclusions and possible self-correction of malocclusions during the development of the dentition. Most studies are cross-sectional and in those of longitudinal design, the results are inconsistent and difficult to interpret. Longitudinal studies would improve our knowledge and understanding of development of the dentition and would also provide data for effective planning of orthodontic treatment: early intervention might be unnecessary if self-correction of the malocclusion occurs during the transition from the primary to the permanent dentition. It is obvious that determining the factors involved in the development of the occlusion during the transitional period from the primary to
the permanent dentition requires knowledge and experience on the part of the clinical observer.
The basis for evidence-based health evaluation is the systematic review, i.e. a compilation of all available scientific evidence on a specified question/problem. The systematic review is an excellent tool for providing comprehensive summaries of evidence within a certain scientific field. It is almost impossible for the clinician to access and evaluate all available information on a specific topic, hence by managing and critically evaluating large volumes of information, the systematic review helps to identify knowledge gaps, and to clarify the need for trials. From an evidence-based perspective, a systematic review of the literature on oral health related problems, with special reference to malocclusions and their impact on the quality of life of children and adolescents would improve our understanding of the topic, identify knowledge gaps and indicate directions for future research.
Malocclusions may or may not influence the quality of life in children and adolescents. Thus, evaluations of the influence of different malocclusions on quality of life will certainly underpin a broader understanding and knowledge about how malocclusions affect the daily life of young patients. This information may also be important when it comes to assessing the most appropriate time for starting orthodontic treatment, not only from a professional point of view, but also, most importantly, from the patients’ perspective.
The studies on which this thesis is based were therefore designed to address several aspects of childhood malocclusions. A longitudinal study was initiated in a cohort of children, enrolled in the Swedish Public Dental Service, providing a unique opportunity to evaluate the prevalence of malocclusions, and changes which occurred, from the primary dentition stage at age 3, through the mixed dentition at age 7, to the early permanent dentition at age 11.5 years. A systematic review of the literature was undertaken in order to compile and clarify the available evidence with reference to the impact of malocclusions on the quality of life of affected children. Finally, a study was undertaken to assess how malocclusions affect the quality of life in the same cohort of children, at age 11.5 years.
AIMS
Paper I
To evaluate the prevalence of malocclusion traits and sucking habits in a cohort of 3-year old children.
Paper II
The aims were threefold:
• To follow a group of children and record occlusal status at ages 3 and 7 years in a cohort of Swedish children, with special reference to the prevalence of malocclusion
• To determine the frequency of self-correction of malocclusion during the transition from the primary to the early mixed dentition
• To analyse the possible influence of sucking habits on the prevalence of malocclusion
Paper III
• The aim was to follow a group of children to determine: • The prevalence of malocclusion from primary to early
permanent dentition
• The frequency of self-correction and new development of malocclusions
• The orthodontic treatment need among children in early permanent dentition
• The possible influence of habits, breathing disturbances, and allergies on the prevalence of malocclusion.
Paper IV
To conduct a systematic review of quantitative studies for evidence regarding the influence of malocclusions on oral health related quality of life (OHRQoL) in children and adolescents.
Paper V
The aims were:
• To describe OHRQoL in a cohort of children at age 11.5 in Swedish dental care.
• To evaluate the impact of malocclusions or orthodontic
treatment need on OHRQoL, with age, gender, socio-economic markers, dental fear and aspects of oral health taken into consideration
HYPOTHESES
Paper I
Malocclusions in the primary dentition are influenced by etiological factors such as prolonged sucking habits and breathing disturbances.
Paper II
The prevalence of malocclusions is higher at age 3 than at age 7 and may be influenced by sucking habits.
Paper III
Malocclusions in the mixed and early permanent dentition are less prevalent than in the primary dentition and may be influenced by sucking habits.
Paper IV
Research published to date provides inadequate or low quality evidence that oral health-related problems influence the quality of life of children.
Paper V
In late childhood, oral health-related problems, including malocclusions, have an impact on self-perceived quality of life.
MATERIALS AND METHODS
SUBJECTS
The study sample was sourced from three Swedish Public Dental Service (PDS) clinics, each located in a small rural community of about 22 000 inhabitants (Figure 1). At study start, in 2003, these clinics had an enrolment of 597 3-year-old children. Forty subjects declined to participate in the study and 29 could not be contacted. Thus, 528 children presented for an initial clinical examination in conjunction with the routine dental examination offered to every child in Sweden at 3 years of age. In order to reduce potential confounding factors such as ethnic differences and environmental conditions, 29 non-Scandinavian children were excluded. Four children with syndromes or developmental disorders (CLP, Cerebral Palsy, Down syndrome) were also excluded. A further 38 children were unable to cope with the examination procedure, resulting in a final sample comprising 457 3-year-old subjects (223 boys and 234 girls). (Figure 1, Paper I)
At the clinical examination at 3 years of age (T0), uncooperative behaviour in a number of children precluded registration of sagittal occlusion or vertical relationships in 5 and 4 cases, respectively. Overjet could not be measured in 18 children.
At 7 years of age (T1), 386 children (187 boys and 199 girls) participated. Because of erupting permanent incisors, measurement of overjet was precluded in 14 children and measurement of overbite in 61.
Finally, at 11.5 years of age (T2), 277 children (128 boys and 149 girls) remained for the second clinical follow-up (Paper III). In the analysis of OHRQoL (Paper V), 13 children were excluded due to on-going orthodontic treatment with fixed appliances and 7 were
excluded due to missing data on the CPQ11-14–ISF:16, giving a final sample of 257 children (121 boys and 136 girls). (Figure 2).
No orthodontic treatment was undertaken in the interval between T0 and T1. Between 7 and 11.5 years (T1-T2), 37 of the 277 (13%) subjects had begun orthodontic treatment and at T2, 13 (4.6%) were still under treatment with fixed appliances.
Figure 1. The study sample was sourced from three Swedish Public Dental
Ethical considerations
The study protocol and informed consent form were approved by the Ethics Committee of the Örebro Health Care region, (Dno: 2003/87/03) and by the regional Ethical Review Board in Uppsala, Sweden (Dno: 2012/273).
METHODS
Papers I – III
The examinations at baseline (T0, age 3) and at first follow-up (T1, age 7) were undertaken by one experienced clinician, the author (LD), between 2003 and 2009. At the final follow-up (T2, age 11.5 years), two experienced clinicians carried out the clinical examinations (the author and B. Lennartsson), between 2012 and 2013. The examiners used a mouth-mirror and probe, and followed a specific protocol. Radiographic examination was not included. Every child was given at least two opportunities to attend the examinations at T0, T1 and T2 respectively.
Clinical examination
Malocclusion was registered in centric occlusion. At T0, the sagittal occlusion was determined by the relationship between the maxillary and mandibular primary canines, according to Foster and Hamilton.4
At T1, sagittal occlusion was registered as at T0, and the relationship between maxillary and mandibular first permanent molars was also registered, according to Björk et al.3 The same method was then used
for registration at T2.
Occlusal measures
Primary canines• Class I (Normal occlusion)
The tip of the maxillary primary canine tooth is in the same vertical plane as the distal surface of the mandibular primary canine tooth
• Class II (Postnormal occlusion)
The tip of the maxillary primary canine tooth is in anterior relationship to the distal surface of the mandibular primary canine tooth
• Class III (Prenormal occlusion)
The tip of the maxillary primary canine tooth is in posterior relationship to the distal surface of the mandibular primary canine tooth
First permanent molars
• Class I (Normal occlusion)
Normal, up to or equal to ½ cusp postnormal or prenormal relation.
• Class II (Postnormal occlusion)
More than ½ cusp postnormal relation.
(At T2 Class II (Postnormal occlusion) was also stratified into division 1 (proclined maxillary incisors) and division 2 (retroclined maxillary incisors).
• Class III (Prenormal occlusion)
More than ½ cusp prenormal relation.
• Overjet was measured at the most protruding maxillary incisor and was classified as normal in the range of 0-4 mm, increased between 4-6 mm and excessive when >6 mm.
• Anterior crossbite was registered if one or more maxillary incisors occluded lingually to the mandibular incisors and checked for anterior shift in the retruded position.
• A deep bite was registered when more than 2/3 of the heights of the mandibular incisors were covered by the maxillary incisors on full closure. At T2 signs of gingival or palatal trauma were also noted.
• Negative vertical overlap was recorded as an anterior open bite. Incisors in edge-to-edge relationship were not considered to be in open bite, nor was lack of overlap due to incomplete eruption of the incisors.
• Posterior crossbite and scissorsbite were recorded if at least two teeth were involved. They were also stratified as unilateral or bilateral and checked for lateral shift in the retruded
position.
In Paper III, following variables were also registered
Anterior space discrepancies
• Contact point displacement was registered at 11.5 years of age (T2): a displacement of 2-4 mm was defined as moderate and >4 mm as severe.15
• Spacing was also recorded at T2, as general spacing and diastema (> 2 mm) between maxillary incisors.
Single tooth anomalies
Impacted, supernumerary, and congenitally missing permanent teeth were recorded.
Orthodontic treatment need
Assessment of treatment need was based on the Dental Health Component of the Index of Orthodontic Treatment Need (IOTN-DHC).2
(Appendix, pages 87-88)
Interview measures
Semi-structured interviews were conducted with both parent and child at the T0, T1 and T2 clinical examinations, using preset questions about sucking habits, breathing pattern including nocturnal breathing disturbances, allergy and dental trauma.
(Appendix, Questionnaire 1- 3, pages 78-80)
New registrations reported in the frame story
Occlusal stage
In order to obtain information on occlusal development at 11.5 years of age, the occlusal stage, as described by Björk et al3 was also
recorded.
Anterior teeth
• DS01 = Primary teeth erupting • DS02 = Primary teeth fully erupted
• DS1 = Early mixed dentition, incisors erupting
• DS2 = Intermediate mixed dentition, incisors fully erupted • DS3 = Late mixed dentition, canines or premolars erupting
• DS4 = Adolescent dentition, canines and premolars fully erupted
• DS5 = Adult dentition
Molars
• M0 = First molars not fully erupted • M1 = First molars fully erupted • M2 = Second molars fully erupted • M3 = Third molars fully erupted
Paper IV – systematic review
Definition of search question and search strategy
The literature review was systematically conducted according to Goodman´s model.48 To identify all studies involving oral
health related quality of life (OHRQoL) and malocclusions and/ or orthodontic treatment need, the following search question was formulated: Do malocclusions have an impact on OHRQoL in children and adolescents?
Five electronic databases (MEDLINE via PubMed, EMBASE, Psychinfo, CINAHL, and the Cochrane Library) were searched for articles published between 1960 and January 2014. The following search syntax was used: “quality of life” [MeSH term] OR “self concept” [MeSH term] OR “patient satisfaction” [MeSH term] OR “personal satisfaction” [MeSH term] OR “well being” [text word] OR “wellbeing” [text word] AND “malocclusion” [MeSH term] OR “orthodontics” [MeSH term] OR “dental esthetics” [MeSH term]. A filter for “child 6-12 years and adolescent 13-18 years” was applied. The computerized search was undertaken with the assistance of a specialist in informatics at the Medical Library, Orebro University, Sweden.
Selection criteria
The following inclusion criteria were preset for the titles, abstracts, and articles.
• Child or adolescent study population
• Healthy study participants without syndromes such as cleft lip/ palate or severe illness
• No previous or ongoing orthodontic treatment among participants
• A focus on malocclusions and quality of life
• Controlled or subgrouped according to presence/absence of malocclusions
• Malocclusions and/or orthodontic treatment need assessed by professionals using standardized measures
• Self-assessed OHRQoL estimated using validated questionnaire instruments
• Full-text articles published in English or the Scandinavian languages
The reference lists of the retrieved articles were also manually searched for additional studies. Three independent researchers (K. Arnrup, L. Bondemark and the author) assessed all the articles with respect to the inclusion criteria. Interexaminer disagreement was resolved by discussion of each article to reach consensus.
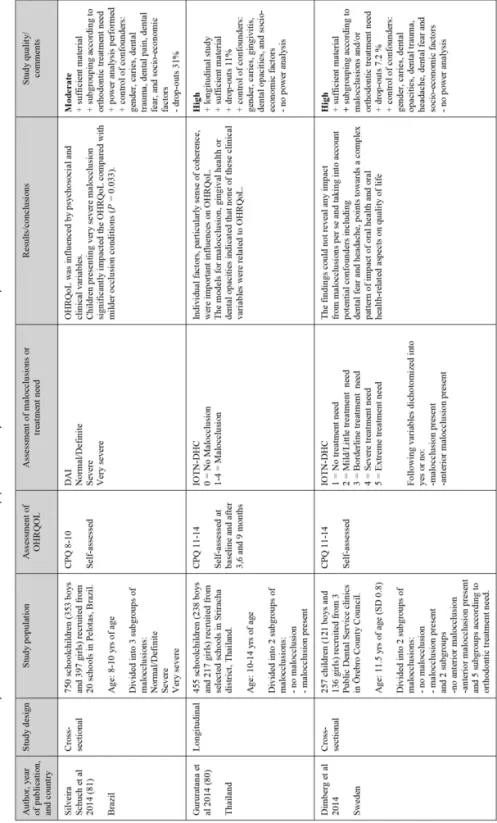
Data collection and analysis
The quality of evidence was classified as high, moderate, or low according to the GRADE system.49 To qualify as high quality, the
articles had to meet the following parameters: sufficient material, relevant stratification, power analysis performed, attrition rate presented and not >30% and the following important confounders controlled: caries, dental trauma, ethnic group, socio-economic factors, age and gender. If any of the above criteria was lacking, the quality of the article was downgraded to moderate. Further reasons for downgrading the quality rating included shortcomings in study design, study limitations, inconsistency of results, imprecision, and reporting bias. Consequently, studies which failed to include data on caries (an important confounder), attrition > 30%, or with no analysis of attrition presented, were classified as low quality. Data from studies assessed as high or moderate quality were tabulated according to the following: author, year of publication, study design, study population, assessment of OHRQoL, assessment of malocclusions or treatment need, results/conclusions, and then assessed. (Table 2, in Paper IV).
Supplementary search
To cover the period between January and September 2014, a new search was conducted of the four databases MEDLINE via PubMed, Psychinfo, CINAHL, and the Cochrane Library, using the same MeSH terms and the same selection criteria, data collection and analysis as described above.
Paper V
Questionnaire measures
To assess the oral health related quality of life (OHRQoL), the children were asked to fill in the Swedish version45 of the Child Perceptions
Questionnaire 11-14 Impact Short Form (CPQ11–14–ISF:16).46
(Appendix, pages 80-85). This short form containing 16 items was used in conjunction with the clinical follow-up examination at 11.5 years of age (T2).
The items of the CPQ11–14–ISF:16 are grouped into four subscales (four items each): oral symptoms, functional limitations, emotional, and social well-being, and also summed up for a total scale score. Each item is related to symptoms associated with the teeth, lips, jaws and mouth during the past 3 months. Response alternatives range from 0 (“never”), 1 (“once or twice”), 2 (“sometimes”), 3 (“often”) to 4 (“every day or almost every day”), with a total score range of 0–64 (subscale scores range from 0 to 16) higher scores correspond with poorer status. The questionnaire also contains two global self-ratings of oral health (using a 5-point scale ranging from “excellent”, “very good”, “good”, “fair” to “poor”) and overall well-being (using a 5-point scale ranging from “not affected at all”, “very little”, “some”, “ a lot” to “very much affected”).
At the same visit, the children rated their dental fear on the Children’s Fear Survey Schedule–Dental Subscale (CFSS–DS).50 (Appendix page
86). The CFSS–DS is a commonly used questionnaire comprised 15 items, with responses ranging from 1 (“not afraid at all”), 2 (“very little afraid”), 3 (“moderate fear”), 4 (“pretty much afraid”) and 5 (“very afraid”), giving a possible score range of 15–75. The CFSS–DS has been validated in several countries, including Sweden.51
The children had the opportunity to ask questions about the questionnaires and, if needed, to get support reading the questions (B. Lennartsson and the author). A separate room at the clinic was
provided for the children to answer the questionnaires. Questionnaires with >25% missing data on any subscale or in total were excluded from the analyses.52 In some of the analyses, scale scores were
dichotomized using the respective medians as cut-off values.
Psychometric evaluation (Supplementary evaluation only in the frame
story)
Subjects for test-retest analyses
Of the 277 subjects, the first 30 children presenting for examination were asked to fill in the CPQ11–14–ISF:16 a second time within 2–4 weeks. Three children failed to respond and the test–retest analysis was therefore based on 27 children.
Interview measures
In conjunction with the clinical examination a semi-structured interview was undertaken with both parent and child using preset questions about dental trauma, headache and socio-economic factors.
Dental trauma, headache and socio-economic factors
The children were asked about their experience of dental trauma and headache. Reported experience of dental trauma was also confirmed by checking the dental records and dichotomized in the analyses into trauma experience or not. Frequency of headache was rated on a 5-point scale from: 0 (“never”) to 4 (“every day”);53 in the analysis,
this parameter was dichotomized into “no” (“never”/“a few times a year”) and “yes” (“every month”/“week”/“day”).
As socio-economic markers, the parents’ educational levels and present occupations were used. In cases where at least one parent was unemployed and/or none of the parents had been educated beyond high school, this was recorded as low socio-economic level. Cohabitation status (child living with both parents or not) was also registered.
Clinical examination
MalocclusionsMalocclusions were recorded as described for Papers I-III (see page 28-30) and thereafter recorded as present or not. The data were then stratified as “any malocclusion” (yes/no), “at least two malocclusion
types (yes/no)” and “anterior malocclusion”, i e. malocclusion in the aesthetic zone (yes/no).
Caries
In the permanent teeth, manifest caries was recorded as decayed missing or filled surfaces (DMFS). A manifest caries lesion was defined as caries detected by probing, or visible on bite-wing radiographs from the most recent scheduled recall visit to the child’s regular clinic dentist. An approximal manifest caries lesion was defined as a lesion clearly extending into the dentine.
Enamel defects
Enamel defects were recorded for permanent teeth and dichotomized in the analysis as either present, in the form of: quantitative loss of enamel (hypoplasia) or qualitative change in translucence (opacity) or as absent: no enamel defect.
Statistical analysis
Sample sizeThis was a convenient sample size for the purpose of a total examination. Therefore no sample size calculation was undertaken.
Descriptive statistics
All data were analyzed using IBM SPSS Statistics (SPSS, Chicago, IL, USA) versions 15.0 (paper I), 17.0 (Paper II) and 22.0 (Paper III and V).
Frequencies, means, standard deviation (SD), and medians for numerical data. Differences with probabilities of less than 5% (P < 0.05) were considered to be statistically significant.
Differences between groups
Student’s t-test (two groups) or one-way analysis of variance (ANOVA) was used to assess differences in numerical data in Papers I-III and V.
Chi-square analysis (Papers I-III and V) and Fisher´s exact test (Paper I) were used to determine intergroup differences in categorical data. The Odds Ratio (OR) with a 95 % confidence interval (CI) was calculated to measure the strength of associations of binary
variables (Papers I-III). In Papers II and III, McNemar´s test was used to compare the same child at two different times.
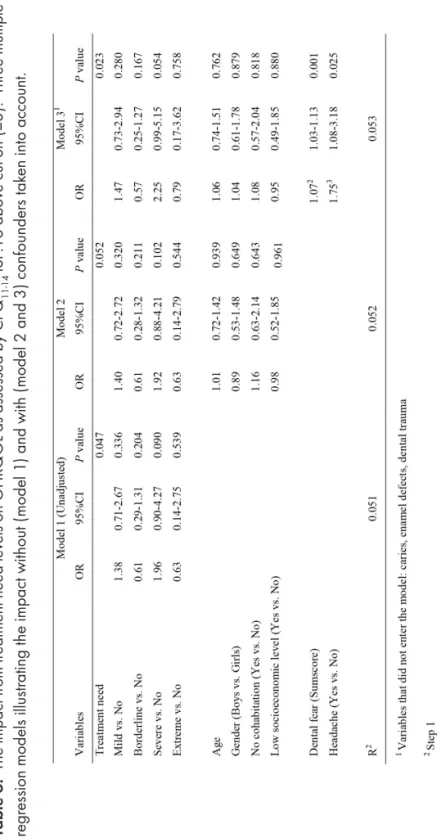
Multivariate analysis
Logistic regression analyses were undertaken in Paper V, using a total CPQ score above cut-off (i.e. above median 8) as the dependent variable, and a significant malocclusion/treatment need variable as the independent discriminant, with possible confounders systematically entered. Age, gender and socioeconomic markers were forced to enter the model, while oral health aspects were added in a forward conditional step-wise selection. The Odds Ratio (OR) with a 95% confidence interval (CI) was calculated as the estimate of the logistic regression.
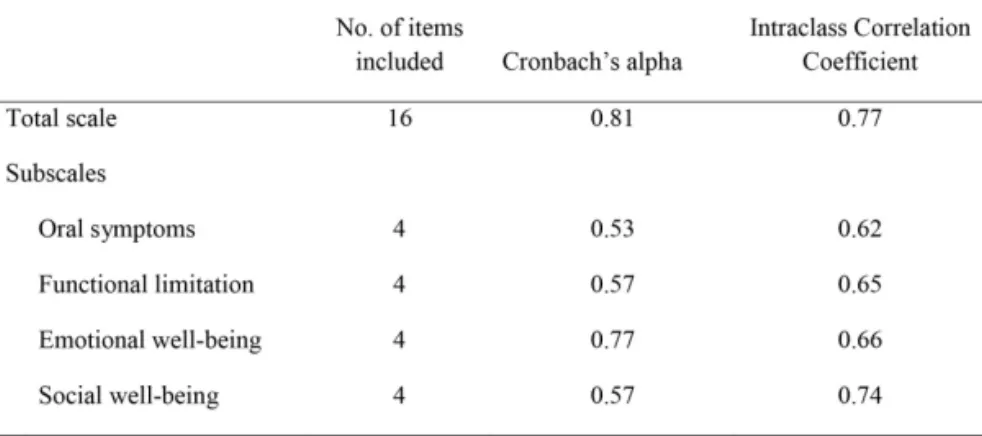
Psychometric analysis
Psychometric analyses were performed and for evaluation of internal consistency, Cronbach’s alpha was used. Alpha values of ≥ 0.70 were considered adequate.54
Method error analysis
In Paper III an inter-examiner test was carried out (20 children participated) using kappa statistics: the kappa values ranged from 0.84 to 1.00.
Additional psychometric analysis (only in the frame story)
For test–retest reliability, the intraclass correlation coefficient (ICC) was computed.54, 55 An ICC > 0.75 represented excellent reliability,
an ICC between 0.60 and 0.75 good, 0.40–0.59 fair, and < 0.40 poor reliability.56 Construct validity was evaluated using Spearman’s
correlation coefficient to correlate CPQ scale scores with global ratings of oral health and overall well-being.
RESULTS
General results
Gender differences, Papers I-III and V
Papers I and V disclosed no significant gender differences associated with any of the variables used in the studies. In 7 year-old children (Paper II), posterior crossbite was more prevalent in girls than in boys (OR = 1.87; P = 0.023) and deep bite was more prevalent in boys than in girls (OR = 10.7; P = 0.006). At age 11.5 years, (Paper III), contact point displacement of more than 2mm was more common in girls than in boys (40% vs. 20%; P = 0.0001). In Paper V, more girls than boys had enamel defects (19 % vs. 10%, P = 0.009) and more boys than girls had experienced dental trauma (18% vs. 14%, P = 0.024). No other gender differences emerged. Consequently, other data for boys and girls were pooled for analysis.
Attrition; reasons and analysis
The rate of attrition between T0 and T2 was 39.4%: 64 children had left the district and 116 declined to participate. At T1, the attrition rate was 15% and the sample was tested for homogeneity by analysing participants and nonparticipants with respect to gender, sucking habits, breathing disturbances or types of malocclusion. The analysis disclosed that at 3 years of age, more boys than girls in the nonparticipant group had sucking habits (OR = 1.7; P = 0.015) or nocturnal breathing disturbances (OR = 3.6; P = 0.040). At T2 the attrition rate was 28%; the most common reason was that the subjects declined to participate (Figure 2). There were no differences in gender, clinic, and prevalence of malocclusions or sucking habits at
3 years of age between those who participated in the final follow-up and those who did not.
Cross-sectional and longitudinal studies on malocclusion
(Paper I-III)
Cross-sectional perspective, Papers I-III
MalocclusionsAt 3 years of age (T0) the prevalence of one or more malocclusions was 70%: the most common were anterior open bite (50%), Class II relationship (26%), increased overjet (23%) and posterior crossbite (19%). (Table 1, Paper I). At 7 years of age (T1) the prevalence of one or more malocclusion had decreased to 58%: the most prevalent were Class II relationship (28%), increased overjet (17%), posterior crossbite (17%) and anterior open bite (10%). (Table 1, Paper II). At T2 (11.5 years of age), one or more malocclusions were recorded in 71% of the subjects: the most common were contact point displacement (31%), increased/excessive overjet (24%), deep bite (18%) and spacing (16%). (Table 1, Paper III).
Occlusal stage and correlation with age
At 11.5 years of age (T2), in more than 80% of the subjects, all the permanent teeth anterior to the first molars were under eruption or in occlusion. (Table 1).
Sucking habits
At 3 years of age (T0), 66% of the children had a sucking habit. The corresponding figures at 7 (T1) and 11.5 years of age (T2) were 4% and 0.4% respectively. Dummy-sucking was the most common sucking habit in both 3 and 7 year-olds. At 11.5 years of age one child had a thumb sucking habit while no one had a dummy-sucking habit.
Ectopic eruption, congenitally missing and supernumerary teeth At 11.5 years of age, ectopic eruption of maxillary canines was diagnosed in 4 (1.4 %) children and hypodontia in 15 (5.4 %). The most commonly affected tooth was the mandibular second premolar (8 children), followed by the maxillary second premolar (6 children) and the maxillary lateral incisor (5 children). One child had two supernumerary teeth in the maxillary midline and another
exhibited a germinated tooth (mandibular left lateral incisor). Finally, transposition of 23 and 24 was observed in one child.
Orthodontic treatment need
At 11.5 years of age (T2) the orthodontic treatment need was distributed as follows: extreme need 3.6%, severe need 18.4%, moderate or borderline need 23.5%, mild/little need 31.4 % and little or no need 23.1%. (Table 3, Paper III).
Table 1. Occlusal stage at 11.5 years of age (T2)
Occlusal stage n % DS 2 M1 53 19.1 DS3 M1 98 35.4 DS 3 M2 1 0.4 DS4 M1 69 24.9 DS4 M2 56 20.2 Total 277 100
Longitudinal perspective from 3 to 11.5 years of age (Paper II and III)
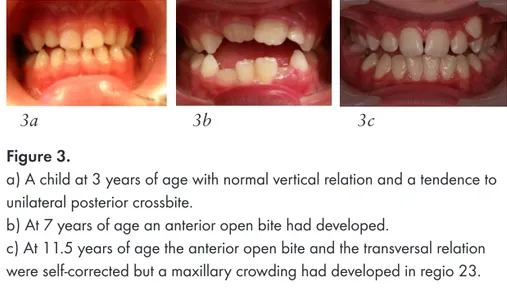
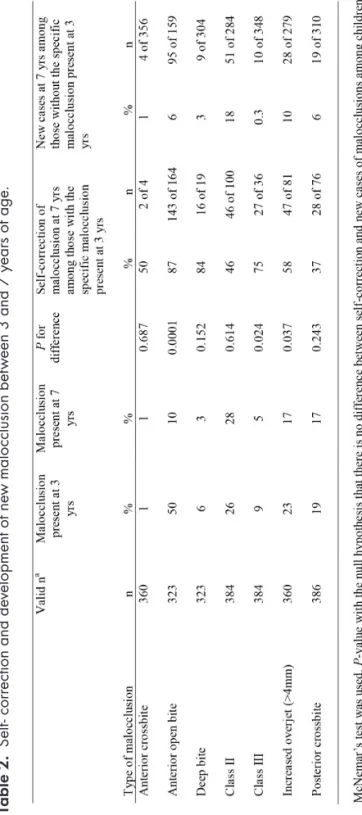
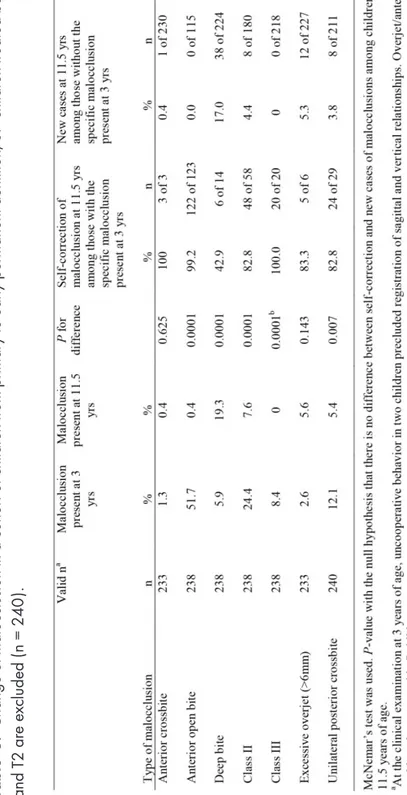
Self-correction and development of new malocclusionsSelf-correction was observed in all types of malocclusion between 3 and 11.5 years of age, but new malocclusions also developed. Between 3 and 7 years of age the rate of self-correction was significantly greater than the development of new malocclusions with respect to Class III malocclusion, increased overjet and anterior open bite. However, the rates of self-correction and the development of new malocclusions were similar for Class II malocclusion, anterior crossbite, deep bite, and posterior crossbite. (Table 2; Figure 3 and 4).
Between 3 and 11.5 years of age, significant self-correction had occurred for open bite, and Class II and III malocclusions had turned into Class I occlusion (Table 3; Figure 3). The prevalence of unilateral posterior crossbite had decreased from 12.9 to 5.1% between 3 and 11.5 years of age (T2). On the other hand, the prevalence of deep bite had increased significantly, from 5.8% to 18.4%. (Table 1, Paper III).
The influence of sucking habits
In children with sucking habits at 3 years of age (T0), the Odds Ratio (OR) was significantly higher for developing an anterior open bite (OR = 4.6; 95% CI: 1.1-19.8; P = 0.025) and posterior crossbite (OR = 3.1; 95% CI: 1.3-7.5; P = 0.008) at 7 years of age (T1). The rate of self-correction of anterior open bite (P < 0.0001) and increased overjet (P = 0.002) was higher for dummy suckers than for finger or thumb suckers. At 11.5 years of age, no association was found between a sucking habit at 3 years of age and any malocclusion. (Figure 5).
Figure 3.
a) A child at 3 years of age with normal vertical relation and a tendence to unilateral posterior crossbite.
b) At 7 years of age an anterior open bite had developed.
c) At 11.5 years of age the anterior open bite and the transversal relation were self-corrected but a maxillary crowding had developed in regio 23.
3a 3b 3c
4a 4b
Figure 4. A child with unilateral posterior crossbite and anterior open bite
The influence of breathing disturbances and allergy
Mouth breathing was prevalent (19%) at age 3, but had decreased to 8% (P < 0.0001) at age 7. The reported prevalence of snoring was almost the same at 3 and 7 years of age (9% and 10%) but had increased to 20% (P < 0.0001) between 3 and 11.5 years of age. Nocturnal breathing disturbances were reported in 5% of the children at 3 years of age but had decreased to 1.4% (P = 0.049) at 11.5 years of age.
At 7 years of age there were associations between snoring and posterior crossbite (OR = 2.28; P = 0.003) as well as between allergy and Class II malocclusions (OR = 3.19; P = 0.001). Moreover, an interdependence was found between mouth breathing and allergy (OR = 1.78; P = 0.045) and between mouth breathing and snoring (OR = 4.56; P < 0.0001). These associations were not confirmed at 11.5 years of age.
Dental trauma
At 7 years of age (T1) 34% of subjects had experienced dental trauma. The prevalence was no higher among children with increased overjet (>4 mm) than those with normal overjet. At 11.5 years of age (T2), the prevalence had decreased to 30% and was more common among children with increased overjet (44% vs. 26%; (OR = 2.2; 95% CI: 1.23-4.04; P = 0.008). Between 7 and 11.5 years of age, incomplete lip closure increased the risk for dental trauma (54 % vs. 28%; OR = 3.1; 95% CI: 1.32-7.22; P = 0.007).
Figure 5. A child with a dummy-sucking habit at 3 years of age showing
an anterior open bite at 3 (a) but a normal occlusion at 11.5 years of age (b).
Table 2. S elf - c or rec tion and de velopment of ne w maloc clusion be tw een 3 and 7 y ear s of a ge .
Table 3. Change of maloc clusion in a c ohor t of c hildr en fr om pr imar y t o e ar ly per manent dentition , 37 c hildr en t re ated be tw een T1 and T2 ar e e xc luded ( n = 240 ).
Systematic review (Paper IV)
The search of the 5 electronic databases produced 1142 titles and abstracts. After scrutiny, 22 articles remained for the quality analysis.57-78 The main reasons for exclusion were:
• Not following the objective of the review • Cleft/lip/palate syndromes or severe illness • Studies of psychometric properties
• Quality of life measured during orthodontic treatment • Letters
• No control or subgroup categorization
Articles excluded for “not following the objective of the review” did not include malocclusions or oral health related quality of life (OHRQoL); some were studies on adult populations.
Six studies were included in the final evaluation of evidence, four with high levels of quality59-62 and two with moderate levels.57, 58 The
remaining 16 studies were assessed as being of low quality; none considered all the important confounders, some utilized insufficient statistical analysis, used selected material, or did not declare the attrition rate.63-78 All six studies included in the final analysis were
of cross-sectional design.57-62 Five were carried out in Brazil,57-61, and
one in New Zealand.62
In four studies the population was based on schoolchildren58,
60-62. In another, a group of schoolchildren served as a control group
for comparison with a group of children awaiting orthodontic treatment.57 Finally, one study had a study population nested in a
birth cohort.59
One of the studies57compared two separate groups, while the
remaining five58-62 allowed subgrouping according to types of
malocclusions and/or orthodontic treatment need.
In five studies,58-62 malocclusion or treatment need was assessed
with the Dental Aesthetic Index (DAI)23 and the other57with the
dental health component and/or aesthetic component of the Index of Orthodontic Treatment Need (IOTN).2 OHRQoL was evaluated
with the Child Perception Questionnaire (CPQ 11-14 or 8-10)44 in
four studies,58, 60-62, the Oral Health Impact profile (OHIP-14)42 in
one study,57, and the Oral Impact on Daily Performance (OIDP)79 in
Impact of malocclusions on OHRQoL
Four studies reported that severe malocclusions, predominantly anterior crowding, spaced dentition, or increased overjet had a negative impact on OHRQoL.59-62 Two studies concluded that
increased orthodontic treatment need had a negative impact on OHRQoL.57, 58 Moreover, two studies revealed that malocclusions
predominantly affected emotional and social well-being.61, 62
In five of the studies, the samples included subjects in pre- or early adolescence; in all these studies, the associations between malocclusions or treatment need were confirmed by multivariate analyses with confounders taken into account.57-59, 61, 62 The sixth
study reported a negative effect of malocclusion on OHRQoL, in particular in terms of anterior spacing or overjet, in even younger children (8-10 years).60
Evaluation of evidence
There was a high level of underlying scientific evidence supporting the negative effects of severe malocclusions on OHRQoL in children and adolescents.59-62 Two studies also confirmed this association
for specific malocclusions in the aesthetic zone: anterior crowding, diastema between incisors, and increased overjet.59, 60 There was
a moderate level of scientific evidence to support the association between severe or moderate treatment need and an impact on OHRQoL.57, 58
In all six studies57-62 the sample size was adequate implying a
sufficient study population, although the birth cohort study, could not include a prior estimate of sample size.59
Attrition rates were disclosed in five studies,57, 59-62, and ranged
from 5% to 19.5%. Moreover, the four studies judged as high quality had taken into account all the most important confounders (caries, gender, age, and socio-economic factors) in their final presentation of the results.59-62
Two studies were downgraded to moderate quality. In one58, no
presentation of attrition was presented and caries was not considered as a confounder. In the other57 caries was the only confounder
Supplementary search
The new literature search covering the period Januari 2014 to September 2014 yielded a further 176 articles but only two met the inclusion criteria. The reasons for exclusion and the number of excluded articles are listed in Table 4. One of the two articles was considered to be of high quality80 and one of moderate quality.81
The study by Schuch et al81 found that OHRQoL was influenced
by psychosocial and clinical variables. Very severe malocclusion had a significant impact on the OHRQoL compared with milder malocclusion (P = 0.033). The other study by Gururatana et al80
showed that individual factors, particularly sense of coherence, were important influences on OHRQoL but the models for malocclusion, gingival health or dental opacities indicated that none of these clinical variables were related to OHRQoL. (Table 5).
Finally, Paper V was evaluated and it was judged to be of high quality. The OHRQoL of the cohort was good and the effect of malocclusions or orthodontic treatment need on OHRQoL was limited and inconsistent. However, dental fear and headache emerged as more distinct impact factors on OHRQoL than malocclusions or orthodontic treatment need. (Table 5).
After considering the articles from supplementary search, Paper IV and V, the scientific evidence is still strong for malocclusions having negative effects on OHRQoL but the impact may be complex.
Table 5. Summar y of OHR QoL s tudie s in t he supplement ar y se ar ch and also P aper V .
Impact of malocclusions on oral health related quality of
life (OHRQoL) - (Paper V)
OHRQoL
The mean total score on the CPQ11–14–ISF:16 was 9.31 (SD 6.24; range 0–33), with no difference between genders. Subscale mean scores were 3.89 (oral symptoms), 2.22 (functional limitation), 1.94 (emotional well-being), 1.26 (social well-being) and ranged from 0 to 10 or 0 to 11.
The mean CPQ scores and proportions above cut-off (using the median for each scale as the respective cut-off value) for children with or without malocclusion, with or without at least two types of malocclusion and with or without anterior malocclusion varied only slightly and no significant differences were found. With respect to the five levels of treatment need, CPQ total and subscale mean scores were highest for severe and extreme treatment need levels (although non-significant; Table 1, Paper V). The proportions above cut-off (CPQ total score) differed significantly between treatment need levels (P = 0.042), with the highest proportions for mild/little and severe treatment need. No significant differences in proportions above cut-off were found for any of the CPQ subscales. There were no significant differences between genders with respect to CPQ mean score, SD or proportions above cut-off.
Descriptive data on caries, enamel defects, dental fear, experiences of dental trauma or headache and socio-economic markers (possible confounders) are presented in Table 2, Paper V.
The logistic regression analyses, presented in Table 6, revealed some impact of treatment need (IOTN level) on OHRQoL (CPQ). There was no clear association between higher severity and higher impact. There were no significant effects of age, gender or socioeconomic markers. When possible confounders, including oral health aspects, were taken into account, the impact of treatment need on OHRQoL remained stable. Dental fear appeared to discriminate for poorer OHRQoL, (OR 1.07; 95% CI 1.03–1.13; P = 0.001). Frequent headache had an impact on OHRQoL, (OR 1.75; 95% CI 1.08-3.18; P = 0.025), while no impact was detected with respect to such variables as not cohabitating with both parents, low socioeconomic level, caries, enamel defects or dental trauma.
Table 6. T he im pac t fr om t re at ment need le vels on OHR QOL a s a sse ssed b y CP Q11-14 -ISF :16 abo ve cut -of f ( ≥8 ). T hr ee multiple lo gis tic re gr
ession models illus
tra ting t he im pac t w ithout ( model 1 ) and w ith ( model 2 and 3 ) c onf ounder s t ak en int o ac count .
Psychometric evaluation - supplementary results only in the frame story
Additional analyses were performed for validation of the Swedish version of CPQ11-14 ISF:16. The internal consistency was sufficient, with Cronbach’s alpha being 0.81 for the 16-item total scale and 0.53–0.77 for the subscales. (Table 7). Test-retest reliability was excellent with ICC (using a two-way random model, absolute agreement and single measures) 0.77 for the total scale and good (ICC 0.62–0.74) for the subscales. (Table 7). Construct validity was tested by correlating the CPQ total score with the two global ratings of oral health (r = 0.41; P < 0.001) and overall wellbeing (r = 0.37; P < 0.001). Significant correlations were also observed between subscale scores and the global ratings of oral health and overall well-being (Table 8). With respect to the effect of malocclusions on overall well-being, rated from “little” to “very much” the mean CPQ total score was significantly lower for subjects who did not consider that they were affected at all than for those who perceived an effect on their overall well-being (6.88 vs. 11.08; P = 0.0001). The frequency of a total score of zero was 2.3% and no child reached the maximal possible score.Table 7. Psychometric characteristics for the Child Perceptions
Questionnaire-Impact Short Form (CPQ11–14-ISF:16) in terms of internal consistency (n = 257) and test-retest reliability (n = 27).
Table 8. Construct validity – rank correlation between Child Perceptions
Questionnaire-Impact Short Form (CPQ11–14-ISF:16) and global ratings of oral health and overall well-being (n = 257).
DISCUSSION
This thesis presents a unique longitudinal study of the prevalence of malocclusions and changes in malocclusion occurring from the primary dentition, through the mixed dentition stage, to the early permanent dentition. The main finding was that while the overall prevalence of malocclusions was similar in the primary and the early permanent dentition, at an individual level, several changes occurred during this period. Self-correction was common in all malocclusions, but new malocclusions also developed, in some cases at similar levels. Thus the overall prevalence remained unchanged.
A further finding, following a systematic review of the literature, was that there was strong scientific evidence that malocclusions in the aesthetic zone have negative effects on OHRQoL, especially at emotional and social levels. However, this thesis revealed that in a cohort of children in the Swedish Public Dental Service system, OHRQoL was high and the effect of malocclusions or orthodontic treatment need was limited and inconsistent. An important finding was that dental fear and headache were shown to have a more distinct impact on OHRQoL than malocclusions or orthodontic treatment need.
Methodological aspects
Papers I-III
To achieve the highest possible level of evidence for a prevalence study, the selected approach was an observational study of prospective longitudinal design, following an age cohort from the primary to the early permanent dentition. The prospective design implies that baseline characteristics, habits, and treatments can be controlled and accurately observed.
The longitudinal design is both a strength and a challenge: the strength is the unique opportunity to follow a cohort over time; the challenge is to limit attrition over time. In order to minimize attrition, all children were given at least two opportunities to attend each examination. The subjects were also given the opportunity to undergo examination at their local Public Dental Clinic. Although total attrition was 39.6%, analysis of the data for those who participated in the final study sample and those who failed to complete the study disclosed no differences with respect to gender, clinic, or prevalence of malocclusions or sucking habits at 3 years of age. Another challenge was that 37 participants had undergone orthodontic treatment between 7 and 11.5 years of age. These subjects were excluded from the analysis of self-correction and development of new malocclusions. Moreover, these subjects had functional disturbances and it would have been unethical to postpone treatment of such anomalies as a functionally disturbing posterior crossbite or excessive overjet. However, these 37 subjects were included in the analysis of orthodontic treatment need: to be under orthodontic care the children had to have presented with a malocclusion categorized as at least severe treatment need.
A method error analysis was performed. Twenty randomly selected children were examined by the two examiners before the final examination (Papers III and V). The measurement error was low. In the first and second examinations (Papers I and II) there was only one examiner: no intra-examiner test was undertaken because it was not possible to arrange for a relevant number of participants to attend for re-examination.
Systematic review (Paper IV)
In health care, the evidence-based approach means that decisions and knowledge are based on the best available scientific evidence. However, because so many articles are published annually it can be difficult for the clinician to sift through and evaluate all the available information. The systematic review is widely acknowledged as an excellent tool for providing the clinician with knowledge in a specific field.
The systematic literature review (Paper IV) was conducted according to Goodman´s model48 and comprised four steps: