Clinical
paper
Changes
over
time
in
30-day
survival
and
the
incidence
of
shockable
rhythms
after
in-hospital
cardiac
arrest
-
A
population-based
registry
study
of
nearly
24,000
cases
Anna
Adielsson
a,*
,
Therese
Dja¨rv
b,1,
Araz
Rawshani
c,
Stefan
Lundin
a,
Johan
Herlitz
da
DepartmentofAnaesthesiologyandIntensiveCareMedicine,SahlgrenskaUniversityHospital,Bla˚ Stra˚ket5,SE-41345Gothenburg,Sweden
b
DepartmentofMedicine,K2,SolnaKarolinskaInstitutet,SE-17177Stockholm,Sweden
cDepartmentofMolecularandClinicalMedicine,UniversityofGothenburg,InstituteofMedicine,SahlgrenskaAcademy,SE-41345Gothenburg,
Sweden
dTheCentreforPre-hospitalResearchinWesternSweden,UniversityCollegeofBora˚s,SE-50190Bora˚s,Sweden
Abstract
Objective:Todeterminechangesovertimein30-daysurvivalandtheincidenceofshockablerhythmsafterin-hospitalcardiacarrest,froma countrywideperspective.
Methods:PatientinformationfromtheSwedishRegistryforCardiopulmonaryResuscitationwasanalysedinrelationtomonitoringlevelofwardand initialrhythm.Theprimaryoutcomewasdefinedassurvivalat30days.Changesinsurvivalandincidenceofshockablerhythmswerereportedperyear from2008to2018.Also,epidemiologicaldatawerecomparedbetweentwotimeperiods,2008 2013and2014 2018.
Results:Inall,23,186uniquepatients(38.6%female)wereincludedinthestudy.Themeanagewas72.6(SD13.2)years.Adjustedtrendsindicatedan overallincreasein30-daysurvivalfrom24.7%in2008to32.5%in2018,(onmonitoringwardsfrom32.5%to43.1%andonnon-monitoringwardsfrom 17.6%to23.1%).Theproportionofpatientsfoundinshockablerhythmsdecreasedoverallfrom31.6%in2008to23.6%in2018,(onmonitoringwards from42.5%to35.8%andonnon-monitoringwardsfrom20.1%to12.9%).Amongthepatientsfoundinshockablerhythms,theproportionofpatients defibrillatedbeforethearrivalofcardiacarrestteamincreasedfrom71.0%to80.9%.
Conclusions:Inan11-yearperspective,resuscitationinin-hospitalcardiacarrestinSwedenwascharacterisedbyanoverallincreaseintheadjusted 30-daysurvival,despiteadecreaseinshockablerhythms.Anincreasedproportion,amongthepatientsfoundinashockablerhythm,whowere defibrillatedbeforethearrivalofacardiacarrestteammayhavecontributedtothefinding.
Keywords:In-hospitalcardiacarrest,Cardiopulmonaryresuscitation,Defibrillation,Survival,Epidemiology
Abbreviations:CPR,cardiopulmonaryresuscitation;IHCA,in-hospitalcardiacarrest;IQR,interquartileranges;OHCA,out-of-hospitalcardiacarrest; SD,standarddeviation;SMD,standardisedmeandifference.
* Correspondingauthor.
E-mailaddresses:anna_adielsson@hotmail.com(A.Adielsson),therese.djarv@ki.se(T.Djärv),araz.rawshani@gu.se(A.Rawshani),
stefan.lundin@gu.se(S.Lundin),johan.herlitz@hb.se(J.Herlitz). 1
Address:DepartmentofMedicine,K2,SolnaKarolinskaInstitutet,SE-17177Stockholm,Sweden.
https://doi.org/10.1016/j.resuscitation.2020.10.015
Received23April2020;Receivedinrevisedform7October2020;Accepted13October2020 Availableonlinexxx
0300-9572/©2020TheAuthor(s).PublishedbyElsevierB.V.ThisisanopenaccessarticleundertheCCBYlicense(http://creativecommons.org/licenses/
Available
online
at
www.sciencedirect.com
Resuscitation
Introduction
Asubstantialproportionofdeathsrelatedtocardiacdiseaseoccurin hospitals.Themortalityrateinpatientsaffectedbycardiacarrestin healthcareunitsishigh,andsurvivalisstronglydependentonthe locationoftheeventwithinthehospital.1,2Thesurvivalrateofpatients
onwardswithmonitoringfacilitiescanbeuptotwiceashighasitison wards without monitoring facilities.3 More advanced surveillance facilitatesthepromptrecognitionofcardiacarrest,resultinginalarger proportion of witnessed cardiacarrests and a shorter time from collapsetotreatment.4
Inapreviousstudyconductedinasingletertiaryhospital,we concludedthat thetreatment ofin-hospital cardiacarrest (IHCA) was characterised by a more rapid start of treatment, over 20 years.3Therewas asignificantincreasein 30-daysurvival,from 44%to56%,onwardswithmonitoringfacilities.Onwardswithout these facilities, there was a substantial decrease in shockable rhythmsovertime,from46%to26%.Thereisaknowledgegapwith regardto changesincharacteristicsand outcomeafter IHCAon monitoring and non-monitoring wards in recent decades from a countrywideperspective.
Theaimofthisstudywasthereforetoexplorefurtherwhether similar changes had taken place in a countywide perspective in Sweden.Theprimaryobjectivewastodescribechangesin30-day survivalandchangesintheproportionofpatientsfoundinshockable rhythmsafterIHCAinSwedenbetween2008and2018.
Inordertoexplorepossiblemechanismsbehindeventualchanges in survival, we also describe patient characteristics and various aspects of resuscitation during twotime periods.The latterdata represent secondary objectives and should only be regarded as hypothesis-generating.
Methods
TheSwedishRegistryforCardiopulmonaryResuscitationstartedin 2005andisanationalqualityregisterwith thehighestdegree of certification, including IHCA and out-of-hospital cardiac arrests (OHCA).TheregistryemploysstandardisedUtstein-styledefinitions forallvariablesandoutcomes.5Atparticipatinghospitals,designated
personnel are responsible for the registration of the information associatedwithcardiacarrest,inasecureonlinesystem.Thedataare collectedintwosteps,attheinitialcardiacarresteventandmorethan 30dayslater.Inthefirststep,baselineinformation,e.g.locationand timeoftheevent,initialrhythm,delaystovariousactions,treatment givenandsurvivalafterresuscitation,isprospectivelyrecordedbya nurseorphysicianattendingtheevent.Inthesecondstep,follow-up data,e.g.co-morbidities,probableaetiologyofthecardiacarrestand 30-daysurvival data,are retrospectively recorded bya nurse or physicianassociatedwiththeregister.
Studydesignandpopulation
We analysed all IHCA registered in the Swedish Registry for CardiopulmonaryResuscitation,from1January2008to31December 2018.Inall,71of73(97%)hospitalswithcardiacarrestteamsin Swedenparticipated.Thenumberofparticipatinghospitalsincreased from45in2008to71 in2018.Thehospitalsrangedinsize from generalprimary-levelhospitalswithfewerthan50bedsto
tertiary-levelhospitalswithmorethan800beds.Theinclusioncriterionwasa cardiacarrestinwhichCPRordefibrillationwasattempted.Patients youngerthan18yearsofagewereexcluded.
Thestudypopulationwassubdividedintofourgroupsaccordingto monitoringfacilitiesontheward(non-monitoringvsmonitoringwards) andinitialrhythm(shockablevsnon-shockablerhythm)atthetimeof the cardiac arrest. Each groupwas furtherstratified in twotime periods,2008 2013and2014 2018inordertogettwogroupswith equal sizeintermsofthenumberofparticipants.Epidemiological data, includingage, gender,co-morbidities (myocardialinfarction, heartfailure,stroke,diabetes,respiratoryinsufficiency,cancerand renaldysfunction),time,locationandcircumstances ofthearrest, treatmentgivenanddelays,survivalimmediatelyafterthe resuscita-tionattempt,survivalat30days,oneyearandduringlongterm follow-up,wereanalysedandcomparedbetweengroups.
Definitionofvariables
“Cardiacarrest”wasdefinedastheneedforCPRordefibrillation.The term “in-hospital” refersto allcardiac arrest occurring within the hospitalperimeter.“CPR”,includingbasiclifesupportandadvanced lifesupport,isperformedaccordingtotheEuropeanResuscitation Councilguidelines.6Whenacardiacarrestisidentified,medicalstaff
callanemergencytelephonenumberandacardiacarrestteam,ledby trainedhealthcareprofessionals,isimmediatelyactivated.
Healthcare facilities were defined as “academic” or “non-academic”hospitalsdependingonwhethertherewasaffiliationtoa medicalschooloradegree-grantinguniversity.Tenofthe participat-inghospitalswereacademichospitals.Healthcareunitsweredivided intowardswith“monitoring”and“non-monitoring”facilities,depending on the availability of continuous surveillance. Monitoring wards includeintensivecareunits,coronarycareunits,coronary angiogra-phy laboratories,operatingtheatres andemergencydepartments. Theremainingwards,includingintermediatewards,aredefinedas non-monitoringwards.Thefirstdocumentedrhythmofthecardiac arrestisdividedinto“shockable”and“non-shockable”rhythm,based ontheindicationfordefibrillationornot.7Previousmedicalhistorywas obtained from the patients’ medical records, based on formerly specifieddefinitions.Apriorhistoryofmyocardialinfarctionreferstoa myocardial infarctionpreceding thearrestby72hormore.Heart failureincludesallformsofheartfailure,exceptforpulmonaryoedema withinonehourbeforethearrest.Previousstrokecomprisesboth haemorrhagicandischaemicstrokebeforethecurrenthospitalisation period.Diabetesincludesbothtype1andtype2diabetes.Respiratory insufficiency includes all typesof respiratory insufficiency withor withouttheneedforaventilator.Cancerreferstoanypreviousor presentmalignancy,regardlessofseverity.Renaldysfunctionwas definedasanestimatedglomerularfiltrationrate(eGFR)of<60mL/ minusingtherevisedLund-Malmoformula.8
Validationofthereporteddata
Validationhasbeenperformedat34hospitals,comprisingatotalof 1338patients,whereregisterdatawerecomparedwithhospitalcase recorddata.Fromthepremisesofthisvalidation,informationabout theplaceofIHCAandsurvivalwasconsistentwithsourcedatain99% ofcases.Similarly,informationaboutwitnessedstatuswasconsistent withsourcedatain96%ofcases,aswellasinformationonthetypeof thefirstrhythm,whichwasconsistentwithsourcedatain94%of cases.
Statisticalmethods
Baseline characteristics are reported usingmeans and medians, alongwithstandarddeviations(SD)andinterquartileranges(IQR), respectively. Standardisedmeandifferences (SMD)wereusedto comparegroups,andlogisticregressionwasusedtocalculatethe adjustedprobabilityof30-daysurvival.Adjustmentwasmadeforage, sexand calendaryear.TheKaplan-Meierestimatorwas usedfor delineatingsurvivalcurvesinrelationtocalendaryear,andthe log-ranktestwasusedtotestfordifferences insurvivalinrelationto calendaryear.Duetoarelatively lowfrequency ofmissingdata, completecaseanalyseswereperformedthroughoutthestudy.Data onage,sex,calendaryearandtypeofwardwascomplete.Dataon initialrhythmwasmissingin7.6%,whichwedeemedasacceptable. Also,previousqualitycontrolshavenotrejectedtheassumptionthat dataaremissingatrandom.AllanalyseswereperformedinRversion 4.0.2(RFoundationforStatisticalComputing).
Ethicalapproval
ApprovalwasobtainedfromtheethicalreviewboardattheUniversity ofGothenburg,Sweden,2017-11-06,referencenumber692-17.
Results
Duringthestudyperiod,23,186uniquepatientssufferedatotal of 23,950IHCA.Atotalof54.9%ofIHCAoccurredonwardswithout monitoringfacilities.Ashockablerhythmattheinitialelectrocardiogram recordingwasfoundin26.3%ofthetotalcases.Mencollapsedmore ofteninashockablerhythmcomparedwithwomen,withaproportionof 69.5%.Overall30-daysurvivalfortheentirestudypopulationwas30.0 %, with highersurvivalfor men(31.3 %) comparedwithwomen (27.9%). Theoverallmeanagewas72.6,SD13.2years,withpatientson non-monitoringwardsbeingolder;74.0,SD13.0years,comparedwith; 70.9,SD13.3years,onthemonitoringwards.Patientsfoundina shockablerhythmwereyounger;70.6,SD12.6years,thanthosefound inanon-shockablerhythm;73.3,SD13.3years.
VariousaspectsofIHCAaredescribed,trendchangesyearby yeararedemonstratedforadjustedsurvivalat30days,overalland
depending on the monitoring level of the ward and the initially registered rhythm, includingthe proportionofpatients foundin a shockablerhythm.Furthermore,changesinpatientcharacteristics andvariousaspectsofresuscitationbetweentwotimeperiodsare compared dependingon themonitoringlevelofthewardandthe initiallyregisteredrhythm.
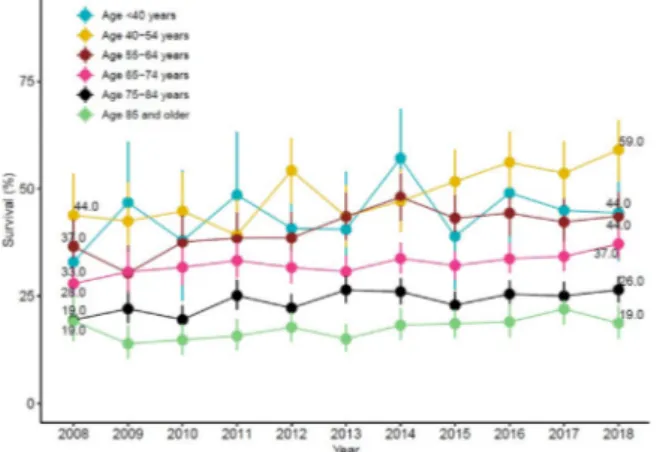
Survival
Theoveralladjusted30-daysurvivalincreasedfrom24.7%in2008to 32.5% in2018. Amongpatientssuffering anIHCAon monitoring wards,theadjusted30-daysurvivalincreasedfrom33.5%in2008to 43.5% in 2018, and among patients suffering an IHCA on non-monitoringwards,theadjusted30-daysurvivalincreasedfrom17.6% in 2008to 23.1% in 2018(Fig.1). Theadjusted 30-day survival increasedmarkedlybothamongpatientswithashockableanda non-shockablerhythm,from53.7%in2008to64.9%in2018forshockable rhythm,andfrom14.2%in2008to22.0%in2018fornon-shockable rhythm(Fig.2).Also,theadjusted30-daysurvivalinbothacademic and in non-academichospitals increased (Fig.3). Theincreased adjusted30-daysurvivalappearedtobemoremarkedinyounger Fig.1–Adjustedtrendsoftheproportionofpatientswho
werealiveat30days,distributedbymonitoringlevelof thewards.
*Unfilledsymbolsdepictunadjustednumbers.
Fig.2–Adjustedtrendsoftheproportionofpatientswho werealiveat30days,distributedbyshockableand non-shockablerhythms.
Fig.3–Adjustedtrendsoftheproportionofpatientswho werealiveat30days,inrelationtothetypeofhospital; academicandnon-academic.
patientsthanintheelderly,andamongpatients>85yearsofage,the adjusted30-daysurvivaldidnotchangeatall(Fig.4).
Finally,notincludedintheoriginalaimandthuspresentedas supplementarydata,inafollow-upupto10years,itwasdemonstrated that among patients suffering an IHCA, the long term survival prognosisispoorregardlessofcalendaryearofcardiacarrestand evenworseforpatientssufferingthearrestonnon-monitoringwards (SupplementaryFig.1).
Proportionofpatientsfoundinshockablerhythms
Theproportionofpatientsfoundinshockablerhythmsdecreased overallfrom31.6%in2008to23.6%in2018.Amongpatientssuffering anIHCAonmonitoringwards, theproportionofpatientsfoundin shockablerhythmsdecreased from42.5% to 35.8%,and among patientsufferinganIHCAonnon-monitoringwards,theproportion decreasedfrom20.1%to12.9%(Fig.5).
Patientcharacteristicsandvariousaspectsofresuscitation
Whenlookingatchangesinrelationtomonitoringleveloftheward, twochanges of presumed clinicalrelevance (standardised mean
difference(SMD)moreorequalto0.1)appeared;(1)therewasan increaseintheprevioushistoryofrespiratoryinsufficiencyon non-monitoringwardsovertime.(2)Therewasalsoadecreaseintheuse ofbufferingagentsonbothtypesofwards(SupplementaryTable1). Whenlookingatchangesinrelationtothefirstrecordedrhythm,we foundthattheproportionofpatientsfoundinshockablerhythmsand defibrillatedbeforethearrivalofthecardiacarrestteam,increased over time from 71.0% to 80.9%. Furthermore, the proportion of patientswith aprevioushistoryofheart failuredecreasedamong patients foundinashockablerhythm.Incontrast,patientswitha previoushistoryofrespiratoryinsufficiencyincreasedamongpatients foundinanon-shockablerhythm.Finally,theuseofbufferingagents decreasedovertime,independentoftheinitialrhythm (Supplemen-taryTable2).
Discussion
Inthisstudyofallin-hospitalcardiacarrestsintheSwedishRegistryof CardiopulmonaryResuscitationbetween2008and2018,themost crucial finding was the increased30-day survival in all facilities, regardless ofmonitoring levelof theward andtheinitial rhythm, despite shockable rhythms decreasing over time. An increased proportionofpatientsdefibrillatedbeforethearrivalofthecardiac arrestteam,whenfoundinashockablerhythm,mayhavecontributed totheimprovedsurvivalrates.Presumably,othercausesareinvolved aswell.
Theentirestudygroupwascharacterisedbyarelativelyhighage (meanage>70yearsofage)attheoccurrenceofcardiacarrest,even though“donotattemptresuscitation”ordershavebeenreportedtobe relatively high among the elderly.9 In agreement with previous studies,10,11wefoundaninverserelationshipbetweensurvivaland age. Several studieshave indicateda clearassociation between increasing age and poor outcomeand vice versa.11,12 However,
recentresearchsuggeststhatbiologicalratherthanchronologicalage mightbeabetterpredictorofmortality.2,13
Ourstudyisnotthefirsttoreportonanincreaseinsurvivalafter IHCA in a countrywide perspective. From the Get With The Guidelines-Resuscitation(GWTG-R)registry,itwasrecentlyreported thatthesurvivalafterIHCAhadincreasedovertimeina17-year perspective.14Similarlytoourfindings,theirresultssuggestedamore
markedincreaseinsurvivalinyoungerpatients.
It is only possible to hypothesise about the mechanisms accountableforanincreaseinthe30-daysurvivaltrend.Apossible explanationcouldbeachangeinthepatientsco-morbidity.However, theonlyrelevantchangesinco-morbiditywasadecreaseinheart failureamongthepatientsfoundinashockablerhythm,aswellasan increase in thehistory ofrespiratory insufficiencyamongpatients foundin anon-shockablerhythmorsufferinganIHCAona non-monitoringward.Although,inpreviousstudies,ahistoryofrespiratory insufficiencyhasbeenstronglyassociatedwithreducedsurvivalafter IHCA.15,16Conversely,thechangeinco-morbidityobservedinour studywould,atleastinoneaspect,tendtodecrease ratherthan increasethesurvivalrateafterIHCA.Thedecreaseinheartfailure overtimewould,ontheotherhand,tendtoimproveoutcome.
ThedelayfromcollapsetothestartofCPRandtodefibrillationis bothcrucialandinverselyproportionaltothechanceofsurvivalin cardiacarrest.17,18Wedidnotfindanymarkedchangesovertime, neitherintheproportionofpatientsreceivingCPRbeforethearrivalof thecardiacarrestteamnorinthedelayfromcollapsetostartofCPR. Fig.4–Adjustedtrendsoftheproportionofpatientswho
werealiveat30days,inrelationtoage.
Fig.5–Trendsoftheproportionofpatientswithaninitial shockablerhythmdistributedbymonitoringlevelofthe wards.
However,theproportionofpatientsfoundinashockablerhythmand defibrillatedbeforethearrivalofthecardiacarrestteamincreased, whichmayhavecontributedtotheincreasedsurvival.Webelievethe bestexplanationforthisimprovementisgreaterawarenessandCPR trainingofthestaff.19However,thedelayfromcollapsetodefibrillation didnotchangeovertime.
Onenotableandtosomeextentpuzzlingobservationwasthe markeddecreaseinshockablerhythmsintheeventofcardiacarrest, primarilyonnon-monitoringwards.Asimilarfindinghasbeenreported inasingletertiaryhospital,3andithasmoreoverbeenrepeatedly observedamongpatientswithOHCA.20Theunderlyingmechanism remains unexplained, but it is possible to speculate about an association with a decreased cardiacaetiology in cardiac arrest due to a number of factors, including improved cardiovascular pharmacologicaltreatment,theuseofearlyrevascularisationinacute myocardial infarction and more frequent implantation of internal cardioverterdefibrillators.20
Thesurvivalofpatientsfoundinashockablerhythmwashigh, morethanhalfsurvivedtooneyear(56.8%)inthelatertimeperiod, andiftheeventoccurredonawardwithmonitoringfacilities,afull 64.2%survivedtooneyear.Eveniftheone-yearsurvivalratefor patientssufferinganon-shockablecardiacarrestwassubstantially lower(16.6%),thechanceofsurvivalincreasedconsiderablyduring thestudyperiod.Inthiscontext,itshould berecognised thatthe prognosis after a cardiac arrest with a non-shockable rhythm is significantlyworse,aspreviouslystated.2,21
Taking other results into consideration, we presume that the improved 30-day survival after IHCA could be explained by the generally better-trained staff, resulting in a higher proportion of patientsdefibrillatedbeforethearrivalofthecardiacarrestteam. EnhancedqualityofCPRandamorepositiveattitudetoCPRamong healthcareprofessionalsmaybeothercontributoryfactors.22Another possibilityisanincreasedselectionofthepopulationthrough“donot attempt resuscitation” orders, excluding an increasing numberof elderly individuals and patients with multiple disorders, from resuscitation. Finally, a more assertive approach to finding and treating reversible causes of the cardiac arrest throughinvasive vascularprocedures,besidesmorerefinedpost-arrestcriticalcare, mightalsobepartofthereason.
Thereported30-daysurvivalin Sweden maybe regardedas relativelyhigh.Therearenotmanynationalreportsregardingsurvival afterIHCAinEurope.AreportfromtheUnitedKingdomfoundan overallunadjustedsurvivaltohospitaldischargeof18.4%23anda recentreportfromtheDanishregistryofIHCAreportedanunadjusted 30-daysurvivalof27.8%.24
Inordertobroadentheperspective,wefinallypresentlongterm survivalof our studygroups. There appear to be relatively even declinesinlongtermsurvival,regardlessofmonitoringlevelofthe ward.Suchafindingshouldberelatedtotherelativelyhighageofthe patientsatthetimeofcardiacarrest.
Studystrengthsandlimitations
Thestudywaspopulation-basedwithwell-definedinclusion/exclusion criteriaandconsiderablesamplesize.Basically,alladult patients sufferinganIHCAinwhomresuscitationwasattemptedinthemajority ofhospitalsinSweden,duringaperiodof11years,wereprospectively andretrospectivelyrecorded. Treatmentinterventionsandsurvival fromIHCAhaveonlybeendescribedfromanationalperspectiveina
fewcountriesinEurope.23,24Allthevariablesincludedintheanalyses
werestrictlydefinedapriori.
Inspiteofthis,limitationtoasinglecountrymakesextrapolationto otherhealthcaresystemsandhospitalsoutsideSwedendifficult.As withallregistrystudies,therewasmissinginformation.Finally,there areuncertaintiesregardingthetimeintervalsthatweremeasured.
Conclusions
Inan11-yearperspective,resuscitationinin-hospitalcardiacarrestin Swedenwascharacterisedbyanoverallincreaseintheadjusted 30-daysurvival,bothonmonitoringandnon-monitoringwards,despitea decreaseinshockablerhythms,particularlyonnon-monitoringwards. Anincreasedproportion,amongthepatientsfoundinashockable rhythm,whoweredefibrillatedbeforethearrivalofacardiacarrest teammayhavecontributedtothefinding.
Authors
’
contributions
Allauthorshavedirectlyparticipatedintheplanningand implementa-tionofthestudy,andintheanalysesandinterpretationofdata.All authorshavereadandapprovedthefinalversionofthesubmitted manuscript.Therearenorelatedmanuscriptsorabstracts,published orunpublished,byanyoftheauthorsofthispaper.
Conflicts
of
interest
Noneoftheauthorshasanyconflictofinteresttodeclare.
Acknowledgements
ThestudywassupportedbytheSwedishstateundertheagreement betweentheSwedishgovernmentandthecountycouncil(theALF agreement;ALFGBG716901,ALFGBG74200),theSwedishHeart andLungFoundation,theSwedishResearchCouncil(2019-02019) andtheGothenburgMedicalSociety.
Appendix
A.
Supplementary
data
Supplementary materialrelatedtothisarticlecanbefound,inthe onlineversion,atdoi:https://doi.org/10.1016/j.resuscitation.2020.10. 015.
REFERENCES
1.SkrifvarsMB,CastrenM,AuneS,ThorenAB,NurmiJ,HerlitzJ. Variabilityinsurvivalafterin-hospitalcardiacarrestdependingonthe hospitallevelofcare.Resuscitation2007;73:73 81.
2.HessulfF,KarlssonT,LundgrenP,etal.Factorsofimportanceto 30-daysurvivalafterin-hospitalcardiacarrestinSweden-a population-basedregisterstudyofmorethan18,000cases.IntJCardiol 2018;255:237 42.
3.AdielssonA,KarlssonT,AuneS,etal.A20-yearperspectiveofin hospitalcardiacarrest:Experiencesfromauniversityhospitalwith
focusonwardswithandwithoutmonitoringfacilities.IntJCardiol 2016;216:194 9.
4.HerlitzJ,BångA,AuneS,EkströmL,LundströmG,HolmbergS. Characteristicsandoutcomeamongpatientssufferingin-hospital cardiacarrestinmonitoredandnon-monitoredareas.Resuscitation 2001;48:125 35.
5.JacobsI,NadkarniV,BahrJ,etal.Cardiacarrestandcardiopulmonary resuscitationoutcomereports:updateandsimplificationoftheUtstein templatesforresuscitationregistries.Astatementforhealthcare professionalsfromataskforceoftheinternationalliaisoncommittee onresuscitation(AmericanHeartAssociation,European
ResuscitationCouncil,AustralianResuscitationCouncil,New ZealandResuscitationCouncil,HeartandStrokeFoundationof Canada,InterAmericanHeartFoundation,ResuscitationCouncilof SouthernAfrica).Resuscitation2004;63:233 49.
6.ZidemanDA,SingletaryEM,DeBuckEDJ,etal.Part9:Firstaid:2015 InternationalConsensusonFirstAidSciencewithTreatment Recommendations.Resuscitation2015;95:e225 61.
7.NolanJP,SoarJ,CariouA,etal.EuropeanResuscitationCounciland EuropeanSocietyofIntensiveCareMedicineGuidelinesfor Post-resuscitationCare2015:Section5oftheEuropeanResuscitation CouncilGuidelinesforResuscitation2015.Resuscitation 2015;95:202 22.
8.NymanU,GrubbA,LarssonA,etal.TherevisedLund-MalmoGFR estimatingequationoutperformsMDRDandCKD-EPIacrossGFR, ageandBMIintervalsinalargeSwedishpopulation.ClinChemLab Med2014;52:815 24.
9.AuneS,HerlitzJ,BangA.Characteristicsofpatientswhodiein hospitalwithnoattemptatresuscitation.Resuscitation2005;65:291
9.
10.MarwickTH,CaseCC,SiskindV,WoodhouseSP.Predictionof survivalfromresuscitation:aprognosticindexderivedfrom multivariatelogisticmodelanalysis.Resuscitation1991;22:129 37.
11.LarkinGL,CopesWS,NathansonBH,KayeW.Pre-resuscitation factorsassociatedwithmortalityin49,130casesofin-hospitalcardiac arrest:areportfromtheNationalRegistryforCardiopulmonary Resuscitation.Resuscitation2010;81:302 11.
12.Al-DuryN,RawshaniA,IsraelssonJ,etal.Characteristicsand outcomeamong14,933adultcasesofin-hospitalcardiacarrest:A nationwidestudywiththeemphasisongenderandage.AmJEmerg Med2017;35:1839 44.
13.LevineME.Modelingtherateofsenescence:canestimatedbiological agepredictmortalitymoreaccuratelythanchronologicalage?J GerontolABiolSciMedSci2013;68:667 74.
14.WibergS,HolmbergMJ,DonninoMW,etal.Age-dependenttrendsin survivalafteradultin-hospitalcardiacarrest.Resuscitation 2020;151:189 96.
15.deVosR,KosterRW,DeHaanRJ,OostingH,vanderWouwPA, Lampe-SchoenmaeckersAJ.In-hospitalcardiopulmonary resuscitation:prearrestmorbidityandoutcome.ArchInternMed 1999;159:845 50.
16.FernandoSM,TranA,ChengW,etal.Pre-arrestandintra-arrest prognosticfactorsassociatedwithsurvivalafterin-hospitalcardiac arrest:systematicreviewandmeta-analysis.BMJ(ClinicalResEd) 2019;367:l6373.
17.HerlitzJ,AuneS,BångA,etal.Veryhighsurvivalamongpatients defibrillatedatanearlystageafterin-hospitalventricularfibrillationon wardswithandwithoutmonitoringfacilities.Resuscitation
2005;66:159 66.
18.SkrifvarsMB,RosenbergPH,FinneP,etal.Evaluationofthe in-hospitalUtsteintemplateincardiopulmonaryresuscitationin secondaryhospitals.Resuscitation2003;56:275 82.
19.AuneS,EldhM,EngdahlJ,etal.Improvementinthehospital organisationofCPRtrainingandoutcomeaftercardiacarrestin Swedenduringa10-yearperiod.Resuscitation2011;82:431 5.
20.KellerSP,HalperinHR.Cardiacarrest:thechangingincidenceof ventricularfibrillation.CurrTreatOptionsCardiovascMed 2015;17:392.
21.NadkarniVM,LarkinGL,PeberdyMA,etal.Firstdocumentedrhythm andclinicaloutcomefromin-hospitalcardiacarrestamongchildren andadults.JAMA2006;295:50 7.
22.KallestedtML,BerglundA,HerlitzJ,LeppertJ,EnlundM.Theimpact ofCPRandAEDtrainingonhealthcareprofessionals’self-perceived attitudestoperformingresuscitation.ScandJTraumaResuscEmerg Med2012;20:26.
23.NolanJP,SoarJ,SmithGB,etal.Incidenceandoutcomeofin-hospital cardiacarrestintheUnitedKingdomNationalCardiacArrestAudit. Resuscitation2014;85:987 92.
24.AndersenLW,HolmbergMJ,LofgrenB,KirkegaardH,GranfeldtA. Adultin-hospitalcardiacarrestinDenmark.Resuscitation 2019;140:31 6.