DOCT OR AL DISSERT A TION IN ODONT OL OG Y FERN ANDO JOSÉ MO TA DE ALMEID A MALMÖ UNIVERSIT C OMPUTED T OMOGR APHY IN ENDODONTIC DECISION MAKIN G
FERNANDO JOSÉ
MOTA DE ALMEIDA
COMPUTED TOMOGRAPHY
IN ENDODONTIC
DECISION MAKING
C O M P U T E D T O M O G R A P H Y I N E N D O D O N T I C D E C I S I O N M A K I N G
Malmö University, Faculty of Odontology
Doctoral Dissertation 2019
© Copyright Fernando José Mota de Almeida, 2019 Photographer and illustrator: Fernando José Mota de Almeida ISBN 978-91-7104-979-7 (print)
ISBN 978-91-7104-980-3 (pdf) Holmbergs, Malmö 2019
Malmö University, 2019
Faculty of Odontology
Department of Oral and Maxillofacial
Radiology and Department of Endodontics
FERNANDO JOSÉ
MOTA DE ALMEIDA
COMPUTED TOMOGRAPHY
IN ENDODONTIC DECISION
MAKING
This publication is also available in electronic format at: muep.mau.se
TABLE OF CONTENTS
PREFACE ... 9 LIST OF ACRONYMS ... 11 ABSTRACT ... 12 POPULÄRVETENSKAPLIG SAMMANFATTNING ... 15 INTRODUCTION ... 18 Endodontics ... 18Computed tomography in endodontics ... 20
AIM ... 28
MATERIAL AND METHODS ... 29
Influence of computed tomography on decisions regarding diagnosis and therapy plan (Studies I–III) ... 29
Decision to request a CBCT (Study IV) ... 33
RESULTS ... 40
Influence of computed tomography on decisions regarding diagnosis and therapy plan (Studies I–III) ... 41
Decision to request a CBCT (Study IV) ... 46
DISCUSSION ... 51 Discussion of methods ... 51 Discussion of results ... 63 Clinical relevance ... 74 Future ... 76 ETHICAL CONSIDERATIONS ... 77 CONCLUSIONS ... 79 ACKNOWLEDGMENTS ... 80 REFERENCES ... 82 APPENDIX ... 92
PREFACE
This thesis is based on the following studies, which are referred to in the text by their Roman numerals:
I Mota de Almeida FJ, Huumonen S, Molander A, Öhman A,
Kvist T. Computed tomography (CT) in the selection of treat-ment for root-filled maxillary molars with apical periodontitis. Dentomaxillofac Radiol. 2016;45(5):20150391.
II Mota de Almeida FJ, Knutsson K, Flygare L. The impact of
cone beam computed tomography on the choice of endodontic diagnosis. Int Endod J. 2015;48(6):564-72.
III Mota de Almeida FJ, Knutsson K, Flygare L. The effect of
cone beam CT (CBCT) on therapeutic decision-making in en-dodontics. Dentomaxillofac Radiol. 2014;43(4):20130137.
IV Mota de Almeida FJ, Flygare L, Knutsson K, Wolf E. “Seeing
is believing”. A qualitative approach to studying the use of cone beam computed tomography in endodontics in Sweden. Int Endod J. 2019. doi:10.1111/iej.13144 [Epub ahead of print].
Studies are reproduced with the kind permission of the publishers: the British Institute of Radiology (Studies I and III) and John Wiley and Sons (Studies II and IV).
The author of this thesis participated as follows:
• Study I: substantial contribution to analysis and interpretation of
• Studies II–IV: substantial contribution to conception, designing, acquisition, analysis, and interpretation of data, drafting and revis-ing manuscript, and final approval.
LIST OF ACRONYMS
2D – two-dimensional 3D – three-dimensional
CBCT – cone beam computed tomography CI – 95% confidence interval
EC – European Commission GDP – general dental practitioner
MSCT – multi-slice computed tomography SD – standard deviation
ABSTRACT
Computed tomography has been used in dentistry as a complement to two-dimensional (2D) imaging since the 1980s. The advent of cone beam computed tomography (CBCT) meant a significant development in dento-maxillofacial imaging, due to sharper images, less radiation, and a lower cost than the conventional multi-slice computed tomogra-phy (MSCT). However, CBCT still uses higher radiation doses and is more expensive for the patient than conventional 2D methods. CBCT is generally considered more accurate than intra-oral radiographs in diag-nosing pathologies or conditions of interest in endodontics. Neverthe-less, the diagnostic process is not only about evaluating radiographs, and it is not certain that the use of CBCT will provide a different chain of actions and ultimately result in a health benefit for the patient. There is thus a need to establish whether the added information of computed to-mography has an impact on diagnosis and therapy choice in endodon-tics.
Guidelines based on the best available evidence have been issued to as-sist clinicians in how to use CBCT. However, little is known about the decision process that drives dentists to request computed tomography, and there is a need for more insight into this process.
The aims of this thesis were to assess the influence of CBCT in diagno-sis and treatment choices, and to gain insight into dentists’ decision pro-cesses when requesting CBCT examinations.
Study I
Five decision makers were presented with intra-oral radiographs show-ing asymptomatic root-filled maxillary molars from 34 consecutively included patients, each with the same fictive clinical history, and asked to choose a treatment option for each root of the maxillary molar. After 1–3 months, they were asked to re-evaluate the molars with the addition of MSCT taken simultaneously with the radiographs. The results showed that MSCT did not improve therapy planning agreement among the decision makers, but it did influence therapy changes within each decision maker, often to more aggressive therapies (e.g. more teeth ex-tractions).
Studies II and III
These studies were prospective observational studies. Seven decision makers in two different clinics made diagnostic and therapeutic assess-ments before and after CBCT during normal clinical practice. The cases were authentic clinical scenarios presented to the decision makers, who were also the actual caregivers. The same cases were used in both stud-ies: 53 consecutive patients referred for CBCT using the evidence-based European Commission (EC) guidelines. The results showed that CBCT significantly influenced changes of diagnosis and therapy plan. The therapy changes were often towards more aggressive therapies, and were strongly correlated with changes in diagnosis. CBCT also im-proved the decision makers’ confidence in their assessments. The deci-sion makers felt that CBCT had a positive impact on health in a large number of patients. However, these studies could not be controlled or blinded.
Study IV
Semi-structured interviews were conducted with 14 strategically select-ed dentists practising in Swselect-eden who usselect-ed CBCT for endodontic pur-poses. The informants narrated on their last three CBCT cases, and the interview transcripts were analysed with qualitative content analysis. The results showed that the dentists requested a CBCT when in need of further visualisation, to facilitate tough decisions, and to allocate some of the responsibility to other parties such as the patients themselves, col-leagues, and radiology specialists. The dentists had a clinical common sense that compensated for unfamiliarity with the EC guidelines. On the
other hand, a “better safe than sorry” attitude (e.g. when tackling diffi-cult patients) counterbalanced the restrictions induced by the common sense approach. There was a belief that the national regulatory system worked as a gatekeeper against over-usage.
POPULÄRVETENSKAPLIG
SAMMANFATTNING
Dator tomografi (DT), eller skiktröntgen, är en röntgenteknik som med-ger röntgenundersökning av volymer och avbildning i tre plan. Sedan slutet av 1980-talet har DT använts i tandvården som ett komplement till vanliga tvådimensionella tandläkarröntgenbilder (intraorala röntgenbil-der). Introduktionen i slutet av 1990-talet av Cone Beam Computed Tomography (CBCT) anpassad för tänder och käkar, innebar ett stort framsteg och gav skarpare och mer detaljerade bilder än konventionell DT, med en lägre stråldos och till lägre kostnad. Både DT och CBCT innebär dock en större stråldos och högre ekonomisk kostnad än kon-ventionella intraorala röntgenbilder.
Europeiska Kommissionen (EK) utfärdade 2012 riktlinjer baserade på bästa tillgängliga bevis för när det är lämpligt att använda CBCT inom tandvård. Det finns dock bristfällig kunskap och därför ett behov av att undersöka huruvida användning av CBCT underlättar diagnostik och terapival gällande sjukdomstillstånd i och omkring tänders rötter (endo-dontiska sjukdomstillstånd) och om det innebär en hälsovinst för patien-ten när man följer EK-riktlinjer för användning.
Syftet med avhandlingsarbetet var att bedöma om undersökning med DT och då speciellt CBCT påverkar val av diagnos och behandling vid sjukdomstillstånd i eller omkring tänders rötter samt att få insikt i tand-läkares beslutsprocess när man efterfrågar en CBCT-undersökning för dessa tillstånd.
Inledningsvis studerades hur användning av DT påverkar terapivalet vid bedömning av rotfyllda tänder med en kvarstående inflammation vid rotspetsen. Dessutom studerades om användning av DT leder till en högre överensstämmelse mellan olika tandläkare om terapival, då detta är en situation där tandläkare ofta har olika uppfattning. DT har i tidi-gare studier visats kunna bidra med potentiellt viktig information, som man inte kan få med vanlig tandröntgen. I vår studie ingick fem tand-läkare som bedömde 34 patientfall med symptomfria tidigare rotfyllda kindtänder med en kvarstående inflammation. Till patientfallen koppla-des en fiktiv standardiserad klinisk historia. Samtliga fall bedömkoppla-des vid två tillfällen av tandläkarna, först utan tillgång till DT-bilder och däref-ter 1-3 månader senare med tillgång till dessa. Resultaten visade att an-vändning av DT, för den enskilde tandläkaren, ofta ledde till mer ag-gressiva terapival. Man valde till exempel oftare att ta bort tanden istäl-let för andra tandbevarande terapier. Användning av DT innebar inte en ökad överensstämmelse mellan olika tandläkare gällande terapival. I andra och tredje delstudien användes 53 autentiska kliniska fall som remitterats för CBCT i enlighet med EK-riktlinjerna. Sju tandläkare från två olika endodontikliniker (specialiserade på rotbehandlingar) bedömde sina egna patientfall i den vanliga kliniska vardagen. Den första bedöm-ningen genomfördes innan CBCT-undersökbedöm-ningen och den andra efter att tandläkaren hade fått tillgång till CBCT-bilderna och remissvar. Re-sultaten visade att information från CBCT-undersökningen i en majori-tet av fallen ändrade val av diagnos, att den påverkade terapivalet och även stärkte tandläkarens tilltro till de egna bedömningarna.
Baserat på resultaten i de tre första studierna uppkom ett behov av en djupare inblick i beslutsprocessen när tandläkare beslutar sig för att ef-terfråga en CBCT-undersökning. En intervjustudie genomfördes invol-verande 14 strategiskt utvalda tandläkare som regelbundet använder in-formation från CBCT-undersökning för diagnostik av och terapiplane-ring vid sjukdomstillstånd i eller kterapiplane-ring tänders rötter. Intervjuer, base-rade på respektive tandläkares tre senaste fall som remitterats för CBCT-undersökning, spelades in och skrevs ut ordagrant. Texten analy-serades och det mönster som framträdde visade att CBCT-undersökning efterfrågades vid ett behov av att se mera, för att underlätta svåra beslut och med en fördelning av ansvar till involverade parter (patient, kollega,
specialist i radiologi). Tandläkarna hade begränsad kunskap om EK-riktlinjerna men använde ”kliniskt sunt förnuft”, vilket begränsade en överanvändning av tekniken. Å andra sidan fanns det en "ta det säkra före det osäkra"-attityd t.ex. vid hantering av patienter som uppfattades krävande, vilket kan leda till onödiga undersökningar. Det fanns dock en övertygelse hos tandläkarna om att de regler som styr användning av röntgen och strålning fungerar som ett filter mot överanvändning av CBCT som undersökningsmetod.
INTRODUCTION
Endodontics
Endodontics is defined by the US National Library of Medicine as “a dental specialty concerned with the maintenance of the dental pulp in a state of health and the treatment of the pulp cavity (pulp chamber and pulp canal)” (1).
Pulp disease is mainly inflammatory (pulpitis) and caused by bacterial irritation in the dentine-pulp complex (2). Bacteria have several routes of entry into the dentine-pulp complex: through caries, enamel cracks, and fractures, as well as restorative and periodontal procedures (3). Pul-pitis ranges from mild to more intense pulp inflammation followed by local necrosis with subsequent infection in a stepwise process which in the absence of treatment can result in full pulp necrosis and root canal infection.
Ørstavik & Pitt Ford defined the biological goal of endodontics as the prevention or cure of apical periodontitis, which is an inflammatory dis-ease of the periapical tissues of the tooth (4). Apical periodontitis usual-ly occurs around the apex where the root canal space communicates with the periodontal ligament; that is, through the apical foramen. The inflammation is induced by an infection in the pulp chamber, or a failed root canal treatment caused by a persistent root canal infection or a rein-fection of the root canal due to an insufficient coronal barrier (5-7). Api-cal periodontitis occurs at the end of the disease spectrum of endodontic pathologies.
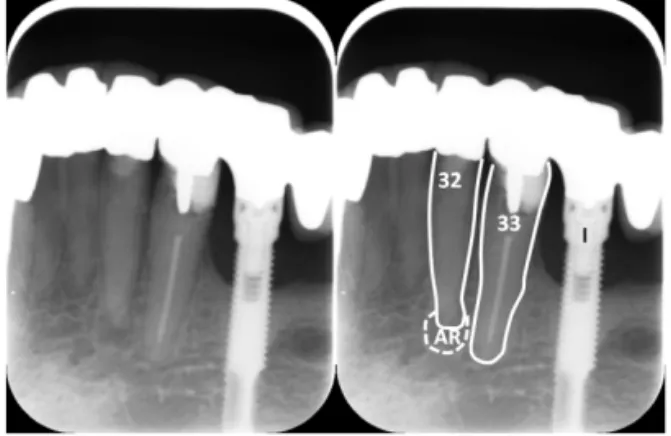
The hard-tissue breakdown which occurs in apical periodontitis allows it to be detected radiologically, as shown in Figure 1 (8). Radiolucencies are uncommon radiographic findings in inflammatory pulp disease (9-11).
Figure 1 – Intra-oral radiograph showing an apical radiolucency that reveals pathological bone destruction. The right picture is the same apical radiograph, with clarifying annotations. The lower left lateral incisor tooth (32) has a crown restoration, as all other teeth. The apical radiolucency (AR) is limited by the dotted line. The lower left canine (cuspid) tooth (33) is root-filled and has a normal apical radio-anatomy. An osseo-integrated dental implant (I) is present. The goal of diagnosis, in endodontics as in general, is to separate health from illness and to understand the patient’s problems in order to offer treatment where relevant. Non-endodontic entities can mimic endodon-tic symptoms, and excluding endodonendodon-tic pathologies is part of diagnos-tics (12). A planned, methodical, and systematic approach is important to the diagnostic process (13).
Endodontic diseases can be asymptomatic, and are sometimes only de-tected as an incidental finding (14, 15). A thorough endodontic exami-nation includes a general and local anamnesis, followed by a physical examination to obtain more information. The physical examination in-volves several diagnostic tests including inspection, palpation of rele-vant structures, and exploring the teeth and gums. Other diagnostic tests such as pulp sensitivity tests are performed when judged suitable. Intra-oral radiographs on indication complete the examination, and provide much useful information which is often essential for the diagnosis. Ten-tative differential diagnoses are created, and then accepted or rejected on the basis of all collected anamnestic, clinical, and radiological data until
a final diagnosis is established (13). More advanced diagnostic auxiliary methods are requested if more information is needed, such as advanced imaging (e.g. computed tomography), histopathological, or microbiolog-ical examinations. Figure 2 depicts some clinmicrobiolog-ical signs that can be found during an intra-oral examination.
Figure 2 – Clinical signs suggesting endodontic pathology which was later con-firmed: sinus tract (arrow on the left picture); and single tooth with acquired blue-grey discolouration after trauma (right picture).
Endodontic treatments will often involve invasive procedures commonly known as a root canal treatment. The majority of treatments are per-formed via coronal access to the pulp space (orthograde treatment) to root-fill the teeth. Sometimes, and particularly in retreatment cases, cli-nicians can choose an apical surgical approach (retrograde treatment) that requires a mucosal flap. The objective of endodontics is to save teeth, although this is not always possible. Prognosis and therapies are heavily dependent on and influenced by the diagnosis.
Computed tomography in endodontics
Intra-oral radiography is the prevailing first-line radiographic technique in endodontics. It is of utmost importance in both diagnostics and the planning of endodontic treatment. Although the technique has a high spatial resolution, it does have some drawbacks, as it magnifies, distorts, superimposes, misrepresents, and compresses the anatomical structures in a single two-dimensional (2D) picture. Moreover, patient compliance is not always optimal due to the intra-oral nature of the technique. Three-dimensional (3D) methods could overcome some of the disad-vantages of intra-oral radiography (16). Computed tomography was in-troduced in the 1970s, and rapidly evolved in the following decades to a
more sophisticated technology such as multi-slice computed tomogra-phy (MSCT), which depicts 3D images. MSCT scanners use a wide fan-shaped ionizing radiation beam in a helical progression. Despite the availability of MSCT, it has seen limited use in endodontics due to con-siderations of cost, access, and radiation dose. The first reported use of computed tomography in endodontics dates back to the late 1980s (17, 18).
The advent of cone beam computed tomography (CBCT) meant a revo-lution in dento-maxillofacial imaging which some have described as a paradigm shift (16). CBCT is a more modern computed tomography technique, and also produces 3D images (Figure 3). CBCT scanners use a narrow cone-shaped beam with one complete rotation or less, resulting in a more limited field of view. The technique provides smaller images of higher spatial resolution with less radiation and at a lower cost than MSCT (16). Computed tomography techniques generally enable better patient cooperation, due to their extra-oral nature.
Figure 3 – Tomograms of a CBCT examination requested pre-surgically for a first right maxillary root-filled molar with an unresolving palatal sinus tract, showing the extent of an apical radiolucency around the palatal root fenestrat-ing the cortical bone. A) axial slice, B) coronal slice, C) sagittal slice.
CBCT does have some limitations. Even with small fields of view, CBCT exposes the patient to a higher effective dose (5–652 microsie-verts) than intra-oral radiographs (0.6–5 microsiemicrosie-verts) (19-21). Arte-facts related to the beam, patient, or scanner can be produced (16). The presence of metal fillings and even root filling materials can cause arte-facts which potentially produce false positive findings (22). There is im-age noise (due to scattered radiation) and partial volume averaging (the
voxel1 does not represent the tissues, but an average of different values), and in comparison to MSCT it has poor soft tissue contrast (16). In Sweden in 2019, the reference prices for a small volume CBCT were 13–18 times more expensive than for an intra-oral radiographic exami-nation of one tooth (23).
The first report on CBCT use in dentistry is from the late 1990s, but the generalised use in dentistry began 5–10 years later (24).
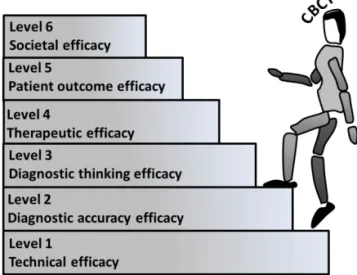
Evidence of efficacy of computed tomography in endodon-tics
The benefit of medical procedures should ultimately be assessed by the effect on health outcome. The hierarchical framework created by Fryback & Thornbury is the most well-known framework for evaluation of studies applied to diagnostic methods (25, 26). The ultimate goal of using a diagnostic test is to improve the patient’s health. The efficacy should be proved stepwise from the base levels towards the top. The dif-ferent levels are shown in Figure 4 and described below with a brief re-view of the evidence of diagnostic efficacy of computed tomography in endodontics.
Figure 4 – Fryback & Thornbury’s hierarchical framework (26).
Technical efficacy (level 1)
Technical efficacy in imaging diagnostic tests is concerned with produc-ing better pictures with less radiation that can enable diagnosis. Some typical measures are resolution and sharpness. This level was not the fo-cus of the present thesis.
Diagnostic accuracy efficacy (level 2)
Diagnostic accuracy is concerned with how good a test is at inde-pendently, accurately, and precisely diagnosing different pathologies or conditions. The test should be compared to a reference standard that de-picts the pathology or condition as exactly as possible. Imaging methods always involve human examiners who have to interpret the images, and it is the joint function of images and examiners that is assessed. Some typical measures are sensitivity and specificity1.
The accuracy of CBCT for endodontic pathologies or conditions of in-terest has been determined by several studies (Appendix 1). CBCT has better overall accuracy than intra-oral radiographs, but the accuracy rate drops when assessing root-filled teeth (27-33). Computed tomography is more accurate and reliable in displaying anatomical landmarks and de-termining measurements than conventional radiography (34-36). Intra-examiner and inter-Intra-examiner agreements are higher for CBCT than for intra-oral radiographs (28, 33, 37-41). However, researchers do not agree on all aspects; although Hiebert et al. found the oral microscope to be better for the detection of a second mesiobuccal (or mesiocentral) ca-nal of maxillary molars than CBCT, De Carlo Bello et al. found the op-posite (42, 43).
Diagnostic thinking efficacy (level 3) and therapeutic efficacy (level 4) While levels 1 and 2 assess the efficacy of the diagnostic test by itself, at higher levels the test is evaluated in conjunction with other diagnostic methods, and when appropriate even with chosen therapies.
Attributing improvements in patients’ health to the use of diagnostic tests should be a consequence of the ability to change clinical decisions (44). As such, the impact of the information provided by those tests in
1 Sensitivity is the proportion of true positives, and specificity is the probability of correctly determining the
choosing diagnoses (level 3) and therapies (level 4) can be used as an empirical proxy measure for the patient outcome (26). Some typical out-come measures for levels 3 and 4 are thus the proportion of times in which imaging contributed to a change in diagnosis or planned man-agement in a case series. Such studies can be also used to measure other secondary outcomes such as confidence, or agreement among decision makers. Improved confidence or reassurance regarding diagnostics or therapy plans has been argued to be a relevant outcome (26).
Prior to the publication of Studies I–III in this dissertation, only one study had examined the therapeutic efficacy of CBCT in endodontics (45). The use of CBCT did not change endodontic therapies significant-ly, but the authors only included cases referred to a specialist clinic in which there was a visible apical radiolucency of at least 3mm in diame-ter.
Patient outcome efficacy (level 5) and societal efficacy (level 6)
Changes in diagnostic and therapeutic decisions do not guarantee per se a positive health effect. The ultimate goal of any imaging test is that its use will improve the patient’s health (level 5) or produce important so-cietal benefits which could be of interest to policymakers charged with allocating funds (level 6).
Studies that randomise endodontic imaging tests with the aim of as-sessing health benefits are rare and generally difficult to perform. One study randomised two groups according to the radiographic examina-tions in order to assess apical surgery via a vestibular approach, but the results of the CBCT examinations were not permitted to influence ther-apeutic decisions, and so the authors could not demonstrate any differ-ences in health outcome from using CBCT (46).
Studies on societal efficacy (so-called cost-effectiveness studies) focus on the economic resources of society and whether those resources are being well used. Assessing the societal efficacy of CBCT depends on knowledge of the impact of CBCT use in patient outcome. Currently, there are no cost-effectiveness studies on computed tomography in en-dodontics.
Implementation of computed tomography in endodontics When new diagnostic imaging methods are being introduced, they should be properly evaluated before implementation to see whether they are better than previous methods. The question is: are they worth im-plementing? This was not done before the introduction of CBCT, as is often the case in radiography, where implementation of new methods frequently precedes adequate evaluation (47).
Nevertheless, the decision to request a computed tomography examina-tion should be based on the best available evidence, as with all medical decisions. The literature on CBCT in endodontics has increased steadily, with hundreds of articles published to date. Guidelines can provide a framework to justify which cases to select, hopefully with the least in-fluence of individual opinion and bias, and they should be valid and fea-sible to put in place (48).
The main European and North American professional endodontic asso-ciations have published separate guidelines concerning the use of CBCT in endodontics to guide clinicians when to use CBCT in different clini-cal scenarios (49-51). However, a review on the quality of existing guidelines concluded that the reporting of these guidelines is poorly pre-sented and that they were mainly developed on the basis of expert opin-ions (48).
In 2012, the European Commission (EC) issued evidence-based lines after a thorough review of the literature (52). Briefly, these guide-lines state that the use of CBCT in endodontics may be indicated only in complex cases for diagnostic purposes as well as for treatment planning, when a thorough clinical and radiological examination has provided in-adequate information to tackle the clinical case. Basic radiological prin-ciples were used as the basis for the recommendations when evidence was lacking (53, 54). Many of the endodontic guidelines were based on “good practice”; that is, they were based on the “clinical expertise of the guideline group and consensus of stakeholders” (52).
Guidelines are means of standardising and improving care quality, but there is usually a gap between evidence and practice (55, 56). The use of diagnostic tests such as computed tomography can be examined by
sur-vey studies, but few such studies have described how CBCT is being used in clinical praxis (57-59). One American survey study found that CBCT was widely used by endodontists, and utilized for several diag-nostic and therapy planning applications in endodontics, including iden-tifying apical lesions, planning non-surgical or surgical retreatments or intentional reimplantations, finding missing or calcified canals, resorp-tions, and assessing healing (57). The responding endodontists com-mented in a general section of the survey that availability influenced the use of CBCT and that the more frequent on-site use might be explained by cost amortization for the device.
Looking at survey studies alone could lead to missing the overall picture and omitting significant information. A qualitative data analysis which takes the context into consideration could explore in greater detail a wider array of factors in the decision process. Researchers might miss these factors because of preconceptions (60, 61).
Knowledge gaps
There is a lack of evidence on the efficacy of computed tomography in endodontics at higher levels than diagnostic accuracy efficacy, and hence a need for studies investigating the impact of the additional in-formation provided by computed tomography both in diagnosis and therapeutic decision making in relation to different endodontic indica-tions.
The feasibility of the evidence-based EC guidelines should be assessed in clinical environments. Other potential interesting indications not cov-ered by the guidelines could warrant a closer look. One such clinical scenario is the root-filled maxillary tooth. It is rather difficult to assess the apical status of maxillary molars on apical radiographs, mainly due to anatomical superimpositions of structures, and sensitivity pulp tests are also useless in such situations. MSCT has been shown to provide po-tentially important information for the process of deciding on the re-treatment of root-filled teeth with apical periodontitis in maxillary mo-lars (62). There is a potential benefit of computed tomography that war-rants further investigation.
Confidence in the assessments and agreement among different clinicians are relatively important when making decisions. Hypothetically, the use of computed tomography could both decrease the variations between different clinicians and increase the confidence in the assessments. This hypothesis could be worth closer inspection.
Little is known about the decision process of requesting computed to-mography in normal clinical praxis. There is a lack of studies delving deeper into this issue, particularly those using qualitative data.
AIM
The aim of this thesis was to improve knowledge on:
• the influence of the additional information provided by computed
tomography when deciding diagnoses and therapies in endodontics (Studies I–III); and
• dentists’ decision-making process when requesting a CBCT
MATERIAL AND METHODS
Influence of computed tomography on decisions
regarding diagnosis and therapy plan (Studies I–III)
Decision makers and patient cases
In Study I, four specialists and one postgraduate student in endodontics participated in the study as decision makers. None of them had any con-tact with or relation to the patients. All cases were presented to all deci-sion makers.
In Studies II and III, three board-certified specialists in endodontics and four postgraduate residents participated in the study as decision makers (and caregivers). They represented all the caregivers practising in two endodontic specialist clinics in Sweden (Luleå and Uppsala), which are the only referring clinics in their respective counties (North Bothnia and Uppsala). Each decision maker was responsible for their own patients, whom they examined, included in the study, assessed, treated, and re-viewed. Each patient was assessed by one and the same decision maker throughout the study.
In Study I, 34 patients (39 teeth) referred in 2005 to a specialist clinic in Gothenburg, Sweden, with a preliminary diagnosis of apical periodonti-tis in root-filled maxillary molar were consecutively included. The pa-tients were the same as in a previous study (62). Only the radiographic material was used in the study. All cases were presented with the same fictive clinical history of asymptomatic apical periodontitis.
In the prospective studies (II and III), the population was selected from consecutive patients attending both clinics (Luleå and Uppsala) from October 2011 to December 2012. The population and the included pa-tients were the same in both studies. All papa-tients (n=1459) referred to the specialist clinics were thoroughly examined clinically and radio-graphically at the endodontic clinics. After the initial examination, all consecutive patients who needed a CBCT examination in accordance with the EC guidelines were included (52). The cases were the authentic clinical scenarios as presented to the decision makers. Patients could have more than one tooth with a related endodontic problem in need of CBCT examination, and 53 patients (81 teeth) were included in the final analysis. Studies II and III are best described as prospective observa-tional before-and-after (computed tomography) studies, as they followed and observed normal clinical praxis.
Radiographic examinations
In Study I, two intra-oral periapical radiographs were taken at the pre-liminary clinical examination in the specialist clinic. Immediately after the intra-oral radiographs, MSCT was performed using the four-channel LightSpeed® QX/I CT system (GE Medical System, Milwaukee, WI, USA). When the data collection was performed in 2005, CBCT was not in general use among dentists in Sweden.
In Studies II and III, intra-oral radiographs were obtained at the endo-dontic clinics as part of the clinical examination before including the pa-tients in the study. Different intra-oral digital radiograph systems were used. CBCT examinations were performed after the clinical examina-tion. Referrals to CBCT had to be in written format, which led to a wide range in time elapsed between the intra-oral radiographs and CBCT ex-aminations (mean 38 days, range 0–196 days). The CBCT exex-aminations took place at two separate radiological clinics, Luleå and Uppsala, Swe-den. Both radiological clinics used the same CBCT model; a 3D-Accuitomo 170 (J. Morita Mfg. Corporation, Kyoto, Japan). The radiol-ogists wrote detailed reports which were used in the assessments. In Studies I–III, the decision makers had access to the whole imaging datasets.
Before-and-after computed tomography assessments
Diagnoses and therapy plans
In Study I, the decision makers initially had access to the presented fic-tional clinical history and the intra-oral radiographs only; the MSCT re-ports were not presented in the first assessment. They then chose a treatment option independently for each root of the maxillary molar in question, selected from the following increasingly invasive options: no treatment, orthograde root canal treatment, retrograde root canal treat-ment, root resection, and extraction (if all roots were to be resected). After 1–3 months, each decision maker re-evaluated each case with the added results of the MSCT. They were blinded regarding their first as-sessment. The available treatment options were the same.
In Studies II and III, the decision maker responsible for the patient as-sessed the cases based on the information obtained by themselves from the clinical and intra-oral radiograph examinations. The decision maker wrote down the best available diagnosis (Study II) and the best available therapy plan (Study III), after the decision to refer to CBCT but before the CBCT examination was performed, in an attempt to reflect the deci-sions that would have been made in the pre-CBCT era.
After the results from the CBCT examination were acquired, the same decision makers reviewed the diagnoses (Study II) and therapy plans (Study III) for their own patient cases. The decision makers again had access to all available clinical and radiological information, including the newly added information from CBCT examination. The evaluation was performed before any further contact with the patient, and so the only difference between the two assessments (before and after) was knowledge of the outcome from the CBCT examination.
Confidence in the assessments – diagnoses and therapy plans
Each decision maker in Studies II and III used a visual analogue scale (VAS) to record their confidence in both the diagnosis and the best available therapy plan proposed for each tooth before and after receiving the CBCT results, concomitantly with performing those assessments. The VAS was a 100 millimetre line with two end-marks; 0 millimetres represented the point “not confident” and 100 millimetres the
end-point “very confident”. The decision maker’s confidence was measured to the nearest millimetre.
The VAS score after CBCT was recorded with the decision maker blinded to their previous score.
Assessments after patient discharge
In Studies II and III, the decision maker reviewed the case after dis-charging the patient and filled out a form (Figure 5) to assess the useful-ness of the CBCT. This form was an adaptation of a form previously used by Wittenberg et al. (63). The decision makers reported changes, if any, between the performed therapy and the initial therapy plan.
Analysis
In Studies I–III, the results were expressed at tooth and patient levels; that is, in different units. In Study I, the treatment reported for each tooth or patient was determined by the more invasive treatment option of the roots involved. In Studies II and III, data were presented for the main problematic tooth in each patient (patient-level) and for all teeth with related endodontic problems requiring a CBCT examination (tooth-level). The main problematic tooth was defined as the tooth in which a change in diagnosis or therapy was noted.
In Study I, descriptive statistics and Cohen’s kappa coefficient were used to analyse the inter-decision maker variation (64). The agreement was analysed at the patient level for all pairs of decision makers (e.g. decision maker 1 vs. 2, 1 vs. 3, 1 vs. 4, and so on) for the assessments before MSCT, and then repeated for the assessments after MSCT. In Studies I–III, differences in diagnoses and therapy plans between be-fore and after assessments were analysed with descriptive statistics. The relation between changes in diagnoses and therapy plans was ana-lysed with chi-square tests (analysis not previously reported).
Differences in confidence measured in VAS scores were analysed for diagnoses and therapy plans using a paired (before-and-after CBCT) samples t-test. The results were reported as a poster presentation at the
16th ESE (European Society of Endodontology) Biennial Congress, Lisbon, Portugal, 12–14 September 2013, but were not part of the pub-lished versions of Studies II and III (65).
Diagnostic understanding:
For this tooth the CBCT exam…
Choice of therapy
For this tooth the CBCT exam…
D1 … confused my understanding
of the patient’s disease and led to investigations I would not otherwise have done.
T1 … led me to choose therapy which
in retrospect was not in the pa-tient’s best interest.
D2 … confused my understanding
of the patient’s disease but did not lead to any additional inves-tigations.
T2 … did not influence my choice of
therapy.
D3 … had little or no effect on my
understanding of the patient’s problem.
T3 … did not change my choice of
therapy but INCREASED MY CONFIDENCE in the chosen ther-apy.
D4 … provided information which
significantly improved my un-derstanding of the patient’s problem.
T4 … contributed to a change in the
chosen therapy but other factors such as (write down)___________ were more important.
D5 … provided THE ONLY
infor-mation for my understanding of this patient’s problem.
T5 … was very important in
compari-son to other factors in the therapy change.
Figure 5 – The questionnaire regarding the usefulness of the CBCT examina-tion, inspired by the original work of Wittenberg et al. (63).
Decision to request a CBCT (Study IV)
Authors’ pre-understandings and contextualisation
FMA (the author of the present thesis) and EW are endodontists, and LF and KK are both dento-maxillofacial radiologists. The authors’ preun-derstandings of potentially important factors that influenced the decision to request a CBCT examination and were more important than adhering to current guidelines were the following: a wish for economic benefit, availability of the equipment, interaction with the patient, and profes-sional curiosity.
In Sweden, endodontists, other specialists, and general dental practition-ers (GDPs) work in different settings. GDPs do not have restrictions
concerning endodontics; they can decide independently whether to treat the patient themselves or refer to endodontic specialists (endodontists), depending on their judgment of difficulty concerning complex diagnos-tic scenarios or technical difficulties. Research has shown that Swedish GDPs perceive endodontic treatments as difficult to perform (66). Phy-sicians, specialists from other odontological disciplines, and GDPs refer patients to diagnose complex clinical scenarios of suspected endodontic origin, among other reasons.
The availability of the CBCT equipment varies. Dentists often need to write referrals when prescribing CBCT examinations, and the patients generally have to wait to be scheduled. In some instances, these tasks are performed by dentists by proxy from a radiologist in accordance with Swedish legislation. The radiologist is always ultimately responsi-ble for quality control and setting up local examination criteria. Non-radiologists cannot independently operate CBCT equipment (67). New regulations have entered into force since Study IV was performed, main-taining though the strict requirements concerning CBCT use (68). Decision makers (informants) and patient cases – data collection
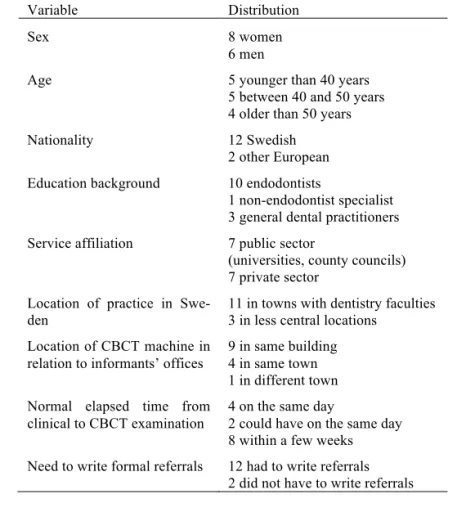
The absolute inclusion criteria were that the decision maker (informant) was a dentist working in Sweden who in recent months had requested CBCT examinations due to endodontic reasons. The purposive selection of informants further aimed to get as much diversity and breadth as pos-sible in order to fulfil a maximum variation sampling strategy (Table 1). Fourteen informants were interviewed. Two more dentists were invited but refrained from participation: one was not interested and the other did not reply. The informants were given written and verbal information about the study, and an interview was scheduled.
The informants were contacted a few days before the interview and asked to go through the records of the last three patients for whom they had requested a CBCT examination due to endodontic reasons. These anonymised cases served as the basis for the interview.
FMA interviewed all informants in Swedish between June 2015 and November 2016 at their own practices. A signed consent to participation
was collected at the same time. The interviews were individual and semi-structured, and all interviews (and cases) began with the same opening question: “Can you tell me how it was decided that the patient needed a referral for a CBCT examination?” The final part of the inter-view concerned guidelines, and was introduced by asking the following question: “There are guidelines issued by various authorities. There are guidelines from the European Society of Endodontology, but also from the European Commission. The guidelines are fairly similar, but in our opinion the authorities have not had much success in spreading the in-formation and as a result few care providers are actually aware of them. Are you familiar with the guidelines?” Open follow-up questions were asked to clarify, deepen, and expand when needed. All interviews were recorded and transcribed verbatim.
Table 1 – Distribution of informants according to several variables
Variable Distribution
Sex 8 women
6 men
Age 5 younger than 40 years
5 between 40 and 50 years 4 older than 50 years
Nationality 12 Swedish
2 other European
Education background 10 endodontists
1 non-endodontist specialist 3 general dental practitioners
Service affiliation 7 public sector
(universities, county councils) 7 private sector
Location of practice in Swe-den
11 in towns with dentistry faculties 3 in less central locations
Location of CBCT machine in
relation to informants’ offices 9 in same building 4 in same town
1 in different town Normal elapsed time from
clinical to CBCT examination
4 on the same day
2 could have on the same day 8 within a few weeks
Need to write formal referrals 12 had to write referrals
2 Ta b le 1 – Th e te xt p re p ar at io n p ro ce ss . Ex am p le s of m ea n in g u n it s, t h ei r co n d en se d f or m s, t h e co rr es p on d in g su b ca te go ri es , a n d c at eg or ies Ex am pl e Me an in g un it Co nd en sa ti on Co de Su bc at eg or y Ca te go ry 1 An d to h el p wi th th e di ag no st ic s th er e, r ig ht … So , to s ee … i f I th in k th er e m ig ht b e an ot he r can al , or i f th er e is an y ap ical d est ru ct io n on th e to oth , s o I w an t he lp s ee in g th is b ette r w ith a C B C T . I w an t he lp f ro m C B C T w it h th e dia gn os tic s. T o se e be tte r. Th er e m ay b e an ot he r ca na l, or ap ical d est ru ct io n. CBCT to o bt ai n mo re in fo r-ma ti on . Pe rc ei ve d co m pl ex di agnos ti c sc ena ri os re qu ire m ore in fo r-ma ti on Vi su al iz at io n as a desi re 2 Y ou al re ady se e he re a round the m es iobuc ca l ro ot , fro m th e in tra ora l [ra di og ra ph ], re ally , th at it ’s no t do in g w el l, bu t her e yo u see th at th is is a pic al pe rio do ntitis a nd th at’ s no th in g, not s om et hi ng tha t’ s har d to see, o f co ur se I see it o n th ese im ag es, b ut i t’ s th ese bo rd er li ne cases w her e it’ s ha rd to d ete rm in e ba se d on in tr ao ra l im ag es , th at ’s m y qu est io n, is it easi er to de te rm in e w ith C B C T ? I ac tu al ly don’ t know . O r is i t jus t as ha rd to dr aw t he l ine th er e? Yo u ca n se e on th e in tr ao ra l [ra di og ra ph ] th at th er e is a pic al pe ri odont it is ar ound the m b ro ot . T ha t’ s no t di ff ic ul t, but it ’s th e bo rd er lin e ca se s w he re it is di ff ic ul t to de te rm ine . M y que s-tio n th en is : Is it ea sie r to d e-te rm in e w ith C B C T ? I do n’ t know . O r is i t jus t as ha rd to dr aw the li ne ? La ck o f know le dge a bout th e b ou nd ar y be tw ee n di se as e an d heal th Th e co nt rad ict or y “t ru th ” 3 An d I th ou gh t 27 l oo ke d dr ea df ul . I di dn ’t th in k… T his is n’ t wo rt h th e ef fo rt , s o to s pe ak , it ’s… W el l. It h ad ap ical p er io do nt it is, i t had poor bone a tt ac hm ent , it ha d abnor m al r oot an at om y, it lo ok ed a little re so rb ed an d… We ll , I th ou gh t… d id n’ t th in k th er e w as a ny good pr ognos is for the tr ea tm ent , to put it I th ou gh t 27 [ w he re th e re fe r-ri ng p ro fe ss io na l w an te d a ro ot can al do ne] lo ok ed bad . N ot wo rt h th e ef fo rt . It h ad a pi ca l pe ri odont it is , abnor m al root an at om y, lo ok ed reso rb ed . Th er e w as n’ t a go od p ro gn os is . In it ia ll y co n-de m ne d toot h Po st po ni ng d if fi cu lt de ci si ons – th er a-pi es a nd pr ognos es Fa ci li ta ti ng to ug h d ec i-si on s
3 si m pl y, so … I ’m us ua ll y ve ry … l ib er al o th-er w ise. I ’m a re al t oo th -lo ve r, so to s pe ak , an d re al ly w an t t o sa ve a nd try to f ix th in gs . I’ m us ua ll y li be ra l; I’ m a to ot h-lo ve r an d re ally w an t to sav e th em . 4 So , i f w e ta ke t hi s la st c as e I ta lk ed a bo ut , y ou co ul d say t hat t her e … t her e ar e in di cat io ns, pe rha ps a bove a ll , tha t you sor t of w ant t o … be s u… T o show t he pa ti ent … t ha t you ta ke th is r ea lly , re ally s er io us ly a nd th at, ah , yo u us e the m et hods a va il ab le to m ak e a … a w is e de ci si on be for e you m ake a r ec om m enda ti on, si nce th e pat ien t is un cer tai n, feel s a li tt le… th in ks th at po or w or k w as d on e be fo re , th at it ha s be en … M aybe t ha t you… s om eone t hi nks so m eo ne w as sl op py an d so o n. S o th en y ou don’ t w ant to be lik e th at. T he n th er e’ s… th er e’ s, ah , an i nd ic… I m ean , a… a car e in di-cat io n th at m ig ht b e m issi ng f ro m t hese so rt s of gui de li ne s. In t he l as t ca se , t he i nd ic at io n is th at you wa nt to be su re , to sh ow th e pat ien t t hat you’ re ta k-in g th is se rio us ly , us in g th e me th od s av ai la bl e be ca us e th e pa ti ent t hi nks pr evi ous c ar e w as sl op py . In t hat case, you don’ t wa nt t o be lik e th at. T he re ’s a car e in di cat io n th at i s no t fo un d in th e g uid elin es . Us es C B C T a s to s up po rt a rg u-me nt s in d is cu s-si on s w it h m is-tr us tf ul p atie nts Ta ck li ng d if fi cu lt pa ti ent s/ si tua ti ons
4 Ex am pl e Me an in g un it Co nd en sa ti on Co de Su bc at eg or y Ca te go ry 5 I: We ’ve di sc us se d it . I know , t he l as t ti m e I ta lk ed t o ou r X -ra y sp ec ia li st h e th ou gh t: “W el l, bu t yo u ca n se nd a f ew c as es j us t fo r th e fu n of it .” An d… F MA : Di d he s ay th at ? I: M m hm m , tha t’ s w ha t he s ai d. *La ug hs a li tt le * F MA : O kay . I: An d th en I f el t… M y nur se r ea ct ed too an d th ou gh t… I do n’t know . F MA : A ra di ol og is t… a rad io lo gi st sai d th at ? I: M m hm m . “W el l, bu t yo u ca n… Ju st t o see a li tt le, h ow m uch d est ru ct io n th er e is ro ug hl y,” a nd w e th ou gh t … N o… I’ m no t goi ng to do tha t. F MA : No t ou t of … we a re t al ki ng a bo ut … of pur e cur ios it y on the pa rt of t he ra di ol o-gi st , o r w as it s om e s tu dy , o r? I: No , no , th at I s ho ul d ha ve b ee n cu ri ou s or … N o, I don’ t r ea ll y know . N o. I a m not su re w hat h e m ean t, bu t… *La ug hs a l it-tle * I ta lk ed to ou r X -ra y sp ec ia li st . He th ou gh t yo u ca n se nd a f ew c as es j us t fo r th e fu n of it , ju st t o se e ho w m uc h de st ruc ti on the re is . I ’m no t g oi ng to d o th at. I ’m no t s ur e wh at h e me an t. Ne ga ti ve react io n to th e r ad io lo gis t wa nt in g mo re CBCT Co ns ul ti ng – pe er s uppor t Al lo ca ti on o f re sp on si bi li ty 6 Ah h… it … I ne ve r sa y th at I mu st do so m e… so m et hi ng . In st ead , I can m ak e … I ne ve r sa y th at I m us t do a ny th in g. I can r eco m m en d an d su gg est tr eat m en ts. Co ns id er in g th e pa ti ent ’s de ci si ons In vo lv in g pa-tie nts
5 a re co m m en da ti on an d… an d su gg es t tr ea tm en ts . A nd th en it is n atu ra lly th e pa-tie nt’ s … us ua lly th e pa tie nt’ s ch oic e. So m et im es y ou r ea ll y ca n’ t le av e it u p to th e p atie nt, b ut u su ally y ou c an . It ’s th e pat ien t’ s ch oi ce. S om et im es you can ’t le av e it up to th e pa tie nt, bu t us ua ll y you ca n. 7 An d I fi nd i t ve ry h ar d to b elie ve th at I wo ul d, wh en I ’m se ei ng a p at ie nt , si t th er e an d th um b th ro ug h th ese ki nd s of g ui de-lin es lo ok in g fo r th em . N ow y ou ’re s up-pos ed to… N o, I ha ve … I t… i t… I a ct ua l-ly do n’ t be lie ve th at ’s ho w den ti st ry wo rk s. I fi nd it h ard to b el ie ve th at I ’d go loo k-in g fo r th e gu id elin es wh il e I’ m se ei ng a pat ien t. T ha t’ s no t ho w den ti st ry wo rk s. On e do es n ot c on-su lt g ui del in es in a car e si tu at io n Gu id el in es a s a gu id el in e
Qualitative content analysis
The analysis was performed according to Graneheim & Lundman (69). The first part was conducted by FMA and EW:
1. All transcripts were read to obtain a sense of the whole.
2. The text was divided into meaning units (groups of words or sen-tences with the same content).
3. The meaning units were condensed while retaining the core idea but excluding unnecessary words.
4. Meaning units related to the aim were selected for further analysis. 5. The condensed meaning units were abstracted into codes that
re-flected the central meaning of the unit.
6. All codes were clustered into categories and subcategories in ac-cordance with their similarities and differences (manifest content). The process is shown in Table 2 with several examples.
After reflection on and comparison of the categories, a theme illustrating the interpretative level (latent content) was formulated by all authors (FMA, EW, KK, LF).
RESULTS
Influence of computed tomography on decisions
regarding diagnosis and therapy plan (Studies I–III)
Changes in assessments after computed tomography
Agreement among decision makers
In Study I, the total agreement for the different pairs of decision makers was 43% before MSCT (range 29–74%) and 42% after MSCT (range 21–59%). Cohen’s kappa coefficient between the decision makers was 0.081–0.535 before MSCT and 0.116–0.379 after MSCT. No marked difference in agreement was noted between before and after assess-ments.
Diagnoses and therapies
In Study I, the suggested treatment was modified in 58% of the patient cases (53% of all teeth) for all decision makers after MSCT. The varia-tion among each decision maker ranged from 38% to 77% (36–66% of all teeth). When the treatment plan was changed after MSCT, it was to-wards a more invasive treatment in 68 assessments (71%) and a less in-vasive treatment in 28 assessments (29%). No treatment was chosen in 33 assessments by all decision makers before MSCT and in 16 assess-ments after MSCT.
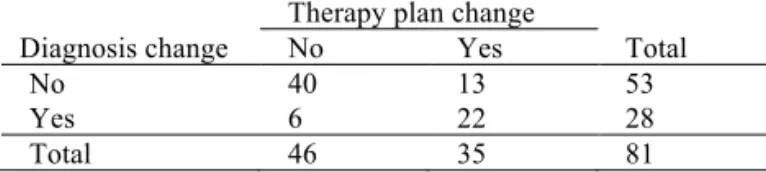
In Studies II and III, 1.3–5.9% of all patients examined by each decision maker were included. The reasons for CBCT referral are shown in Table 3. The diagnosis changed in 22 patients (42%) after CBCT. There were 28 changes of diagnosis among all 81 teeth examined (35%). The thera-py plans were changed in 28 patients (53%) and in 35 of all teeth (43%)
after CBCT. When changing treatment plans, CBCT led to more aggres-sive treatment in 16 patients (57%) and less aggresaggres-sive treatment in 5 patients (18%).
Table 3 – Reasons for referral to CBCT in Studies II and III.
Reasons for CBCT referral Patient’s main
problematic tooth np (%)
All teeth nt (%)
Symptomatic teeth judged healthy 4 (8) 12 (15)
Suspected dental fractures 6 (11) 6 (7)
Suspected or established resorptions 3 (6) 3 (4)
Differentiating pathology from normal anatomy 25 (47) 39 (48)
Pre-surgical aid 13 (25) 19 (23)
Location of foreign body structures 2 (4) 2 (2)
Total 53 (100) 81 (100)
np, number of patients; nt, number of examined teeth.
The relationship between diagnostic and therapy plan changes for all teeth is shown in Table 4. The chi-square test indicated a strong relation between changes in therapy and changes in diagnosis (p<0.001)
Table 4 – Distribution of changes of diagnosis and therapy plans after CBCT for all teeth (Studies II and III).
Diagnosis change
Therapy plan change
Total
No Yes
No 40 13 53
Yes 6 22 28
Total 46 35 81
There were reasonable explanations for the 19 teeth in which changes were not congruent. Where therapies did not change despite different diagnoses (n=6), there were diagnoses of necrotic pulp that after CBCT were transformed to apical periodontitis, for which the treatment is the same. In some patients, the therapy changed even though the diagnosis did not (n=13). In these cases, CBCT provided diagnostic information that led to different therapy despite the lack of change in the general di-agnosis. For example, CBCT could assist decision makers in deeming teeth untreatable, or lead them to perform an orthograde treatment of an untreated canal instead of previously planned surgery, to change a watchful approach to more aggressive therapy, or to refer patients to a pain clinic.
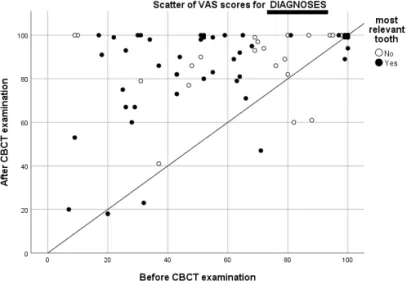
Confidence in diagnosis
For all teeth, the mean score for diagnostic confidence before the CBCT examination was 62mm (standard deviation [SD]: 30). After CBCT, the mean of the changes in diagnostic confidence for all teeth was +24mm (95% confidence interval [CI] of the difference: +18–30mm, SD: 27, p<0.001). Results are plotted in Figure 6.
In each patient, the mean change in confidence after CBCT examination was higher for the main problematic tooth than for the other less prob-lematic teeth, except when there were no changes in diagnosis after CBCT. For the main problematic tooth, 13 of 26 teeth with a prelimi-nary diagnosis of apical periodontitis scored over 95mm in VAS. Many of these teeth were referred for CBCT examination for pre-assessment before endodontic surgical therapy, and the diagnosis did not change. These teeth lowered the mean difference in VAS scores for the diagnos-tic confidence of teeth with no change in diagnosis, as the mean score before CBCT examination was high. In contrast, the mean confidence score for a preliminary diagnosis of healthy main problematic teeth was just 39mm (n=7, SD: 19).
Figure 6 – VAS scores for confidence in diagnosis before and after CBCT for all teeth. The patient level (the main problematictooth for each patient) is rep-resented with black dots. The line represents no changes in VAS score after CBCT. Dots above the line represent increases in VAS score, and dots below the line represent decreases in VAS score.
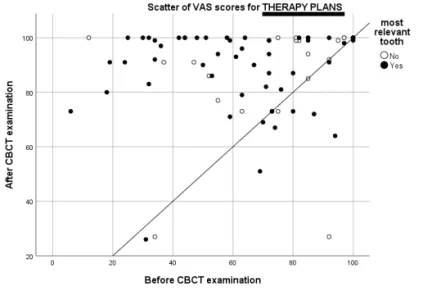
Confidence in the therapy plans
The final analysis count was of 52 patients (78 teeth) due to a protocol breach. The mean therapeutic decision confidence score before CBCT was 67mm (SD: 25) for all teeth. The mean of the changes in therapeu-tic decision confidence after CBCT for all teeth was +22mm (CI of the difference: +16–28mm, SD: 28, p<0.001). Results are plotted in Figure 7.
The mean change in confidence after CBCT examination was higher for the main problematic tooth than for the other less problematic teeth, ex-cept when there was no change in diagnosis after CBCT. The differ-ences for the other teeth were smaller as the initial VAS scores were higher, but these results were not statistically significant.
Figure 7 – VAS scores for confidence in therapy plans before and after CBCT for all teeth. The patient level (the main problematictooth for each patient) is represented with black dots. The line represents no changes in VAS scores af-ter CBCT. Dots above the line represent increases in VAS score, and dots below the line represent decreases in VAS score.
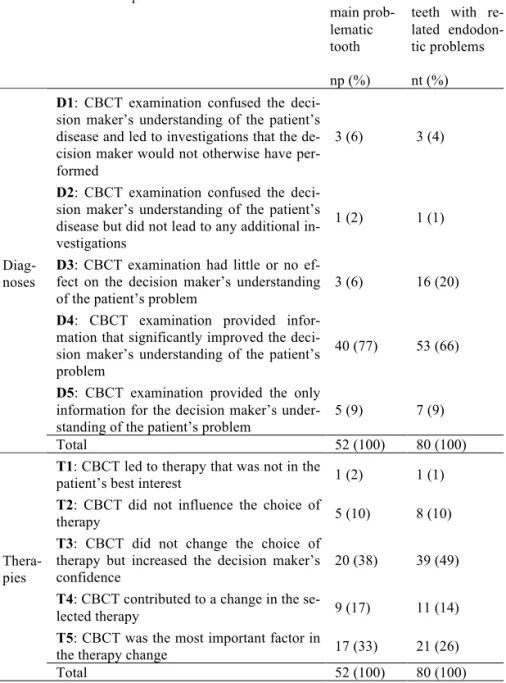
Assessments after patient dismissal
The responses to the retrospective questionnaire regarding the effect of CBCT examination on patient care modified after Wittenberg et al. are presented in Table 5 (63). One patient (1 tooth) dropped out due to a protocol breach.
The therapy plans were executed as planned in 45 of the 52 patients who reached patient dismissal stage.
Table 5 – Estimated usefulness of CBCT examination after patient dismissal, using a retrospective questionnaire adapted from the original questionnaire of Wittenberg et al. (63).
Decision maker’s response Patient’s
main prob-lematic tooth np (%)
All examined teeth with re-lated endodon-tic problems nt (%)
Diag-noses
D1: CBCT examination confused the
deci-sion maker’s understanding of the patient’s disease and led to investigations that the de-cision maker would not otherwise have per-formed
3 (6) 3 (4)
D2: CBCT examination confused the
deci-sion maker’s understanding of the patient’s disease but did not lead to any additional in-vestigations
1 (2) 1 (1)
D3: CBCT examination had little or no
ef-fect on the decision maker’s understanding
of the patient’s problem 3 (6) 16 (20)
D4: CBCT examination provided
infor-mation that significantly improved the deci-sion maker’s understanding of the patient’s problem
40 (77) 53 (66)
D5: CBCT examination provided the only
information for the decision maker’s under-standing of the patient’s problem
5 (9) 7 (9)
Total 52 (100) 80 (100)
Thera-pies
T1: CBCT led to therapy that was not in the
patient’s best interest 1 (2) 1 (1)
T2: CBCT did not influence the choice of
therapy 5 (10) 8 (10)
T3: CBCT did not change the choice of
therapy but increased the decision maker’s
confidence 20 (38) 39 (49)
T4: CBCT contributed to a change in the
se-lected therapy 9 (17) 11 (14)
T5: CBCT was the most important factor in
the therapy change 17 (33) 21 (26)
Total 52 (100) 80 (100)
Decision to request a CBCT (Study IV)
The informants in Study IV, who were all dentists working in Sweden, requested a CBCT when in need of further visualisation or to facilitate tough decisions, sometimes after allocating some of the responsibility to others such as the patients themselves, colleagues, and radiology spe-cialists. To illustrate the pattern identified in their responses, seven dif-ferent subcategories were organized into three categories, revealing the manifest content (Table 6). The interpretation of the latent content re-vealed a theme describing the process of deciding to request a CBCT for endodontic reasons: A balance between clinical common sense and a “better safe than sorry” attitude guides the use of CBCT in endodontic settings in Sweden. The national regulatory system was perceived to work as a slightly porous gatekeeper against over-usage. The theme is represented in Figure 8.
Figure 8 – The theme revealed by the analysis of CBCT use in endodontic set-tings: A balance between clinical common sense and a “better safe than sorry”
attitude guides the use of CBCT in endodontic settings in Sweden. The national
regulatory system was perceived to work as a slightly porous gatekeeper against over-usage.
Categories
A condensation of the informants’ narratives is presented in the respec-tive categories below.
CBCT was not part of the normal daily routine, but was preceded by a thorough clinical evaluation. In the clinical situation, the informants conducted a thorough examination comprising a general and local an-amnesis and the external and internal status including inspection of hard and soft tissues; palpation of muscles, teeth, and alveolar process; teeth percussion; teeth and pocket probing; and sensitivity tests. CBCT, and radiography in general, were thus considered as supplementary tools to-gether with other clinical information:
“Now, the radiology is not the only thing that matters – you must have the clinical picture, after all.”
Available radiographs were examined, and new ones were taken if needed. Some informants always took two new eccentric intra-oral radi-ographs.
Table 6 – The categories and their respective subcategories.
Categories
Visualization as a
desire Facilitating tough deci-sions Allocation of respon-sibility
Subcat-egories
Perceived complex diagnostic scenarios require more infor-mation
Postponing difficult de-cisions -therapies and prognoses
Consulting – peer support
The contradictory
“truth” Tackling difficult pa-tients/situations Involving patients
Guidelines as a guide-line
Visualization as a desire (category)
When cases appeared difficult because traditional methods were not enough, there was a need to “see” what was happening (Table 2, Exam-ple 1). Radiographs could raise suspicions, but achieving near-certainty with conventional methods was not always possible. Other diagnostic tests, such as sensitivity tests, did not necessarily help, as they were sometimes neither trustworthy nor easy to perform. Clinically difficult scenarios included repeated periods of pain and swelling, long periods of unclear pain, persistent problems after treatment (e.g. sinus tracts, pain); clinical information that indicated non-endodontic pain,
incon-sistent clinical and radiographic findings and symptoms, the need to ex-clude pathology (e.g. inadequate root-fillings without clear signs of api-cal destruction and informants not wanting to “miss anything”), root re-sorptions, a need to know if there was communication of the lesion to sinus in cases where perforations were found, possible additional un-treated canal with visible lumen, and geminated teeth. Unclear symp-toms were also seen to present difficulties:
“It was actually myofascial pain … But at the same time … the symptoms were so vague, I still wanted to do this … CBCT exam to really confirm that it looks okay.”
In some situations, the informants trusted that the previous evaluation by a referring colleague had been adequate. In these cases, they acted as a “central coordinator”.
CBCT was believed to be the “answer key”, substantiated by positive experiences where the use of CBCT was perceived to be beneficial for the patient (e.g. resorption cases). However, some contradictory views were stated, including fear of misjudging the CBCT images, problems with artefacts, and negative experiences such as missed canals which were later found using the oral microscope (Table 2, Example 2). Facilitating tough decisions (category)
Decisions were sometimes difficult to make. CBCT could help in select-ing the strategic option when several scenarios were possible, or it could be an interim solution, preventing the informants from taking therapeu-tic actions in which they did not believe, or letting them be sure they had not missed anything important before judging teeth as unsalvageable. Although informants had to ask themselves whether treatment would be worth the effort, they did not want to miss possible treatments in im-portant teeth before extraction, particularly as their colleagues could have trusted in their skill to save important teeth (Table 2, Example 3). Aside from the objective odontological situation, patients could be a demanding problem in themselves. Patients perceived as difficult, con-frontational, uncomfortable, or distressed about previous treatments could infect the informants with uncertainty. When this happened, there was a need to “raise the diagnostic bar”, show the patients that they