The clinical success, survival and failure of
titanium-ceramic tooth-supported
constructions submitted to patients at the
Faculty of Odontology, Malmö University
- A retrospective clinical study
Marie Mahlberg
Åsa Blom
Supervisor: Christel Larsson
Master Thesis in Odontology (30p)
Malmö University
Programme of dentistry
Faculty of Odontology
Kliniskt lyckande, överlevnad och
misslyckande av titan-keramiska
tandstödda konstruktioner utlämnade till
patienter på Odontologiska Fakulteten,
Malmö Högskola
- En retrospektiv klinisk studie
Marie Mahlberg
Åsa Blom
Handledare: Christel Larsson
Masteruppsats i odontologi (30p)
Malmö Högskola
Tandläkarprogrammet
Odontologiska Fakulteten
Table of Contents
ABSTRACT ... 4 SAMMANFATTNING ... 5 EXPLANATION OF TERMS USED IN THIS THESIS ... 6 INTRODUCTION ... 7 BACKGROUND ... 7 TITANIUM ... 7 CERAMICS ... 9 VENEERING CERAMICS ... 9 CURRENT STATE OF KNOWLEDGE CONCERNING TITANIUM-CERAMIC FDPS ... 9CALIFORNIA DENTAL ASSOCIATION EVALUATING SYSTEM ... 10
AIM AND RESEARCH QUESTION ... 11 MATERIALS AND METHOD ... 12 PATIENTS ... 12 RESEARCH JOURNAL ... 12 DEFINITIONS ... 13 Surface ... 13 Margin ... 13 Success ... 13 Survival ... 13 Failed ... 13 CALIBRATION ... 14 CLINICAL EXAMINATION ... 14 ETHICS AND SECURITY ... 14 RESULTS ... 15 SINGLE CROWN EVALUATION ... 15 SINGLE CROWN ABUTMENT TEETH ... 16 FIXED DENTAL PROSTHESIS EVALUATION ... 16 FIXED DENTAL PROSTHESIS ABUTMENT TEETH ... 17 THE PATIENT’S EVALUATION ... 18 NON-RESPONSE ANALYSIS ... 18 DISCUSSION ... 19 CHOICE OF MATERIAL ... 19 METHOD ... 20 PATIENTS ... 20 RESULTS ... 20 BIAS NON-RESPONSE ANALYSIS ... 23 ETHICS ... 23 CONCLUSION ... 24 APPENDIX 1: INFORMATION LETTER ... 25 APPENDIX 2: THE ORIGINAL EVALUATION SYSTEM ... 26 APPENDIX 3: RESEARCH JOURNAL ... 27 APPENDIX 4: RESULTS ... 29 APPENDIX 5: NON-RESPONSE ANALYSIS ... 33 REFERENCES ... 35
Abstract
Aim
The aim of this study was to evaluate the clinical success, survival and failure rate of titanium-ceramic single crowns (SCs) and fixed dental prostheses (FDPs) submitted to patients at the Faculty of Odontology, Malmö University.
Materials and Method
To answer the research question, patients with SCs and/or FDPs made in titanium-ceramic at the Faculty of Odontology, Malmö University, between year 2011-2015, were identified and later examined by, two dental students during their eight semester (April 2016), with a visual-tactile method.
Results
The study contained a total of 47 participating patients, this outcome represented 69 % of all the patients found matching the inclusion and exclusion criteria during the patient selection. Out of the 47 participants, 67 restorations were obtained and examined. The 67 restorations that were included in the study had a mean age of 35 months and a median age of 29 months. Out of these, 47 were SCs and 20 were FDPs.
The clinical success, survival and failure rate of the SCs were 55%, 43% and 2%,
respectively. The clinical success, survival and failure rate of the FDPs were 15%, 70% and 15%, respectively.
Conclusion
Within limits of this study the following conclusions were made:
• The titan-ceramic SCs submitted to patients at the Faculty of Odontology, Malmö University had a higher success rate compared to the FDPs.
• The results indicate an overall high and acceptable success and survival rate for the titan-ceramic restorations.
Sammanfattning
Syfte
Syftet med föreliggande studie var att utvärdera kliniskt lyckande, överlevnad och
misslyckande för metal-keramiska singelkronor och broar med underkonstruktion av titan som lämnats ut till patienter på Odontologiska fakulteten, Malmö högskola.
Material och metod
För att svara på den aktuella frågeställningen identifierades patienter som mellan åren 2011-2015 fått fastsittande protetiska konstruktioner i titan-keramik, på Odontologiska fakulteten, Malmö högskola. Patienterna undersöktes av två tandläkarstudenter, under deras åttonde termin (april 2016), med visuell-taktil metod.
Resultat
47 stycken patienter ingick i studien, detta motsvarade 69% av alla patienter som matchade inklusions - och exklusionskriterierna. Hos dessa 47 patienter fanns totalt 67 konstruktioner med en medelålder på 35 månader och en medianålder på 29 månader. Av de inkluderade konstruktionerna var 47 stycken singelkronor och 20 broar.
Den kliniska lyckande, överlevnad och misslyckande frekvensen för singelkronorna var 55%, 43% och 2%, medan den för broarna var 15%, 70% och 15%.
Slutsats
Inom studiens begränsningar har följande slutsatser dragits:
• De titan-keramiska singelkronorna utlämnade till patienter på Odontologiska fakulteten, Malmö högskola, hade en högre lyckandefrekvens än de titan-keramiska broarna.
• Resultatet indikerade en övergripande hög lyckande- och överlevnadsfrekvens för titan-keramiska konstruktioner.
Explanation of terms used in this thesis
• Single crowns are abbreviated as SCs• Fixed dental prostheses are synonymous with bridges and are abbreviated as FDPs • Restoration/constructions are synonymous with single crowns + fixed dental
Introduction
Dental health and appearance areconsidered important in today’s society. Individuals suffering from tooth loss have shown to experience low self-esteem, lower social status, and impaired function. Scientific evidence indicates that people who receive prosthodontics treatment, i.e. replacement of missing teeth, experience increased self-esteem and improved function (1).
Background
There are several ways to replace missing teeth with numerous prosthodontics options such as single-/multiple-unit fixed dental prostheses, removable dental prosthesis, implants etc. In 1907 the lost wax technique was introduced resulting in the casting of for example fixed dental prostheses frameworks. Metal-ceramics were introduced to prosthetic dentistry in the 1960’s (2,3), using different types of gold alloys with fused porcelain. Over time the metal-ceramic metals have undergone major changes. The main influential factors for this
developments are economics, mechanical properties, biocompatibility, and aesthetics (4,5). For example the constant growing gold price led to changes in the Swedish dental care support system. The Swedish government accounted for a large part of patients dental cost including treatments with noble alloys but in 2002 a new dental health care reform was introduced, the so-called “65 plus-reform”. This implied that noble alloys no longer were compensated for by the government resulting in higher cost for the patients. In turn this lead to greater demands for more affordable dental prosthetic materials such as cobalt-chromium (Co-Cr) and titanium (Ti) alloys (3-6). These demands were also easier to meet due to the fact that the constitution from 1991, that prohibited the use of base metal alloys in dentistry, was abrogated in 1999 (7). During this time the use of Co-Cr alloy became more common which resulted in a more affordable material and a material with better mechanical properties (Co-Cr alloys exhibit an elastic modulus up to 220 GPa, which is about twice as much as gold alloys) (4,5). However, over the years the importance of biocompatibility also became a more central requirement for the materials used in dentistry. Clinicians began to question the
appropriateness of the metals used in metal-ceramic constructions, such as CoCr, and because of this, titanium received considerable attention due to its excellent biocompatibility and high corrosion resistance (3,4,8). Meanwhile gold, cobalt, and chromium have been shown to be potentially allergenic (9).
Titanium
Titanium is today used for dental implants as well as for all-metal and metal-ceramic
prostheses. Titanium has a melting point at 1668 °C and is also an allotropic, which means it has the property of being able to appear in different phases with different characteristics. The allotropic transformation occurs at 882 °C (4,8,11), the material then converts from α-phase, a hexagonal close-packed crystal structure, to β-phase, a stronger and more ductile
body-centred crystal structure. By incorporating stabilizers, the temperature of which phase
transformation occurs will be altered. For example, incorporation of vanadium, which is a β – phase stabilizer, will cause the transformation from β to α phase to occur at a lower
temperature on cooling. Incorporating aluminium, which is a α-phase stabilizer, will cause transformation from α to β phase to occur at a higher temperature on heating. A combination of α and β phase stabilizers will result in an alpha-beta alloy, which is the most used titanium alloy in tooth-supported dental constructions (4,12).
These alloys are low priced and have good mechanical properties, which make them a suitable alternative in dentistry (4,11,13). The elastic modulus, 110 GPa, is slightly higher than the elastic modulus for unalloyed gold. The metal has low density, 4.5 g/cm-3
, which makes it 4 times lighter than gold resulting in light dental prostheses. However, the greatest advantage is titanium’s excellent biocompatibility (4,9,11,13).
Corrosion of metal and release of ions cause a biological response and depending on duration and quantity of exposure the biological response can result in mutations, system toxic, local toxic, or allergic effects. Titanium is a highly reactive substance with especially high affinity to oxygen and reacts spontaneously and rapidly with it at room temperature, creating an oxidized surface (9,11,14). Despite this and because of this titanium has excellent
biocompatibility. The oxide surface protects the metal from corrosion and release of metal ions making it very stable. At the same time the oxide layer can complicate the binding between porcelain and titanium. An oxide layer that is too thick can result in compromised bonding strength leading to fractures between the oxide layer and the titanium or within the oxide layer. To avoid this it is important to control the oxidation process and thereby limit its thickness (11-13).
The production techniques used for producing titanium prosthetics are casting, milling, spark erosion, and a combination of the last two techniques with laser welding (9,11). The casting procedure of titanium has several problems, such as titanium’s high melting temperature, high affinity to components in the investment material (resulting in an reactive layer on the casting surface), phase transformation and high affinity to oxygen and nitrogen (8,12). When titanium is heated up to temperatures above 500°C the oxygen and nitrogen diffuses through the
titanium surface and become layered into the crystal network making the metal hard, brittle, and difficult to process (12). Therefor it is necessary to minimize the exposure of substances that can react with titanium during the manufacturing process. Thus, a special casting
investment is used consisting of oxides, such as MgO, ZrO2, or Y2O3, which are more stable
than titanium oxide and therefor do not react with the titanium. Furthermore casting is done under the protection of an inert gas, argon or helium (4,12). Through development of the other production techniques such high temperatures are not needed and therefor these problems during casting are avoided and phase transformation is reduced (9).
Ceramics
Ceramics are a group of materials characterized by their biocompatibility, aesthetic potential, chemical inertness, wear resistance, and high hardness. They are essential to obtain tooth like appearance and good aesthetics when using metal framework. They are also considered brittle because of their inability to deform plastically. Ceramics can be divided into three main groups, porcelains, ceramics, and oxide ceramics. Ceramics normally consist of a glass-phase and a crystal-glass-phase. The glass-glass-phase contributes to the materials aesthetics meanwhile the crystal-phase gives the material its good mechanical properties, these properties apply to porcelains and glass-ceramics. Oxide ceramics on the other hand consists of only crystal-phase giving it its excellent mechanical properties but the aesthetic properties do not come close to the other two ceramics (3,15).
Veneering ceramics
To veneer metal-ceramic dental constructions porcelain and glass-ceramics are used (3,15). Veneering titanium is difficult due to excessive oxidization at 800 °C and phase
transformation at 882 °C of the metal. This oxidization causes the formation of a darkened layer, which makes aesthetics challenging, and weakens the bond between the porcelain systems and titanium, whiles the phase transformation alters the original properties of the metal. Therefore, a ceramic sintering temperature below 800 °C is desirable to minimize oxidation and to avoid conversion of the alpha phase to the beta phase (4,8,9). Furthermore, when veneering titanium, special low expansion ceramics are needed to adapt to the relatively low thermal expansion coefficients of titanium. If these factors were not taken into
consideration the consequence would be veneering chip off fractures.
When binding ceramics to a metal framework, bond strength is based on three factors: chemical bonding, mechanical bonding, and thermal stress bonding (3,4,9). The chemical bonds are acquired through the oxide layer of the titanium consisting of covalent and ionic bonds. These integrate with the glass-phase of the ceramic forming Si-O bridges. Mechanical bonding is gained through physical locking between the two surfaces microstructures.
Ceramics can withstand high compressive stress but is relatively sensitive to tensile stress, which causes fractures. The thermal stress bonding is obtained through a slight mismatch of the titanium and the ceramics thermal expansion coefficients resulting in a residual
compressive force in the ceramic veneer, preventing crack formation. Specifically the ceramic must have a slightly lower thermal expansion coefficient compared to the metal in order to develop surface compression upon cooling (4,16).
Current state of knowledge concerning titanium-ceramic FDPs
Today’s research on the success, survival, and failure of titanium-ceramics FDPs show various outcomes. Several studies indicate a higher success and survival rate for conventional metal-ceramic prostheses however others imply that titanium-ceramic restorations are equal to conventional metal-ceramics (8,9,17). Many studies also indicate that the main complication for titanium-ceramic prostheses is ceramic fractures. Some studies even stated that the risk for ceramic fractures is high (8,17,18). Despite all this, titanium-ceramics have shown to have
acceptable clinical performance, which applies to both single crowns and bridges. However, one can see differences in success and survival rates between single crowns and multiple unit constructions, but in general single crowns have a higher success and survival rate than bridges (8,18).
California Dental Association evaluating system
During the 1970, on behalf of the California Dental Association (CDA), Professor G. Ryge and associates drafted guidelines for quality assessment of dental fillings, amalgam and resin restorations. The aim was to create a more objective evaluating system. The quality of
“Surface and Colour”, “Anatomic shape” and “Margin integrity” were assessed by using four sub-classifications “Alfa”, “Bravo”, “Charlie” or “Delta” with specific criteria and
corresponding key words. Based on the sub-classification the fillings were overall rated as “Satisfactory” or “Nor acceptable”. This rating system has since then been reevaluated and redrafted to fit evaluation of other dental constructions. Professor G Ryge and associates encourages the use of their operational approach in a system for evaluating the quality of other types of restorative work, but points out that appropriate characteristics, criteria and key words would need to be identified for it to be useful (19,20).
Aim and Research Question
The aim of this study was to evaluate the clinical success, survival and failure rate of titanium-ceramic single crowns (SCs) and fixed dental prostheses (FDPs) submitted to patients at the Faculty of Odontology, Malmö University.
This led to the research question: What is the clinical success survival and failure rate of titanium-ceramic SCs and FDPs submitted to the patients at the Faculty of Odontology, Malmö University?
The hypothesis were:
The clinical success and survival rate for titanium-ceramic SCs and FDPs produced at the Faculty of Odontology is acceptable
The success rate for titanium-ceramic SCs and FDPs at the Faculty of Odontology, Malmö University, is lower than the survival rate due to complications in the ceramic veneer.
Materials and Method
To answer the research question, patients with SCs and/or FDPs made in titanium-ceramic at the Faculty of Odontology, Malmö University, between the years 2011-2015, were identified and later examined by, two dental students during their eight semester (April 2016), with a visual-tactile method.
Patients
The patient base for the clinical study was selected from all dental technician bills regarding titanium-ceramic SCs and FDPs, performed by dental students and teachers at the Faculty of Odontology, Malmö University. Patients who matched the inclusion and exclusion criteria; having received titanium-ceramic restorations more than 10 months ago, at the Faculty of Odontology, Malmö University, were eligible for the study. All the bills between the years 2011-2015 were scanned and the potential patients were manually listed in a patient registry. The data received from the technican bills were cross-checked with the information in the patient's dental record. SCs and FDPs that were never cemented were excluded from the study and those that were either lost or removed due to pathology were included as failed without any clinical examination. These findings were noted in the patient registry. The patient's dental records were also scanned with the purpose of finding other titanium-ceramic SCs and FDPs that were not present among the technician bills.
The patients were then contacted viaphone and informed about the project, the clinical
examination, risks with participating, management of patient data, the patient’s right to say no and their right to cancel the examination at any time during the study. An appointment was booked and a timecard together with a letter, containing the same information that had been given verbally, was sent via post to all concerned. The information letter can be viewed in appendix 1. Patients who weren't willing to participate or did not answer were marked red in the patient registry. These are further presented and discussed in the Results and Discussion.
Research journal
Prior to the clinical examination a research journal was developed to evaluate the SCs, FDPs and the abutment teeth. The journal was based on the California Dental Association (CDA) evaluation system and modified according to the present research questions. The original evaluation system is presented in appendix 2 and the modified version can be viewed in appendix 3.
Based on this modified evaluation system the surfaces and marginal adaption of the SCs and FDPs where examined, visually and tactile with an explorer. The abutment teeth were evaluated by presence of caries, gingivitis/periodontitis, and fractures. When FDPs abutments were evaluated all of the teeth were combined and viewed on as one abutment unit. Caries and fractures were examined by visual-tactile methods using a dental explorer. By using a periodontal probe on four surfaces of each abutment tooth, periodontal conditions were
assessed. Probing depth (4-5 mm or ≥ 6 mm) and bleeding on probing were registered. The same elements were also examined and registered for the contralateral. If the contralateral also had a SC or an FDP another equivalent tooth was chosen to represent the contralateral.
Definitions
The restorations surfaces and margins were assessed using the sub classification “Romeo”, “Sierra”, “Tango” and “Victor”.
Surface
• Romeo indicated that the surface was smooth and the surrounding soft tissue was unharmed.
• Sierra indicated a pitted surface or a mild roughness, easily adjusted, and/or small fractures within the ceramic.
• Tango indicated a gross roughness, still adjustable and/or fractures causing metal exposure.
• Victor indicated unadjustable defects. Margin
• Romeo indicated no visible gap between abutment tooth and crown margin. The explorer dose not engage with the margin
• Sierra indicated a visual and/or tactile marginal discrepancy.
• Tango indicated a margin discrepancy were an explorer can penetrate. • Victor indicated a partial or complete detachment of the SC or FDP.
By compiling the subclassification of the surface and the margin an overall rating; success, survival and failed, was established for each SC and FDP.
Success
Classification “Romeo” on both surface and margin gave an overall assessment of success. A restoration was also assessed as success when the margin was downgraded to “Sierra”, since the priority of the study was to evaluate the materials quality and function in the oral cavity.
Survival
When the surface was judged to be “Sierra” the assessment was considered to be survival. Furthermore when the subclassification ”Tango” was the poorest grade, the overall assessment of the restoration was considered to be survival.
Failed
When the subclassification ”Victor” was the poorest grade the overall assessment of the restoration was considered to be failed. If the restoration wasn’t present at the time of the examination the margin was automatically graded with the subclassification “Victor”
Calibration
Two weeks before the clinical examination the two dental students were calibrated according to the research journal. The research journals sub-classifications and criteria were discussed until fully understood. After this the students examined six restorations, following the research journal, on patients that were not part of the study, under supervision of Doctor Christel Larsson, prosthetic specialist.
Clinical examination
In the beginning of the examination, information about the study was once again given the to patients, who then signed a form of consent. All participants were asked if they were satisfied with their titanium-ceramic restoration or if they thought it was necessary to implement any adjustments or even remake the construction. Deviant and/or negative response was noted in the research journal.
“Student 1” completed the visual-tactile examination following the research journal, excluding the periodontal conditions, to avoid bleeding during “Student 2’s” examination. Throughout this procedure, “Student 2” was not present. Right after the first examination, the second examination performed by “Student 2” followed, also according to the research journal and this time including the periodontal conditions. “Student 2” was not aware of “Student 1’s” grading of the restoration and abutment tooth/teeth. If the two students’ grading did not correlate a mutual agreement was reached after a discussion and a joint
re-examination. The patients were informed of any clinical findings. If pathology or other conditions that needed attention were present the patients were directed to further care. As a gesture of gratitude all participating patients were offered a professional tooth cleaning at the end of each session.
Ethics and security
Before the project started a consultation with Lars Bondemark, chairman of ethical council, at the Faculty of Odontology, Malmö University, concerning an ethical review took place. Because the examination was not considered to be invasive and did not involve any risks for the patient, no ethical review was needed. Throughout the project all personal data was handled according to the Personal Data Act (1998:204). All documents were stored in a secure and fireproof locker and the research journals were decoded and could therefore not be tied to any specific patient.
Results
The study contained a total of 47 participating patients, this outcome represented 69 % of all the patients found matching the inclusion and exclusion criteria during the patient selection. Out of the 47 participants 67 restorations were obtained and examined. The loss, 31%, was due to patients who the students were not able to contact, patients that were contacted but did not want to participate and patients who had an appointment but did not attend. This is further presented in a non-response analysis later in the results. The 67 restorations that were
included in the study had a mean age of 35 months and a median age of 29 months (range of 10 to 84 months). Out of these, 47 were SCs and 20 were FDPs.
Single crown evaluation
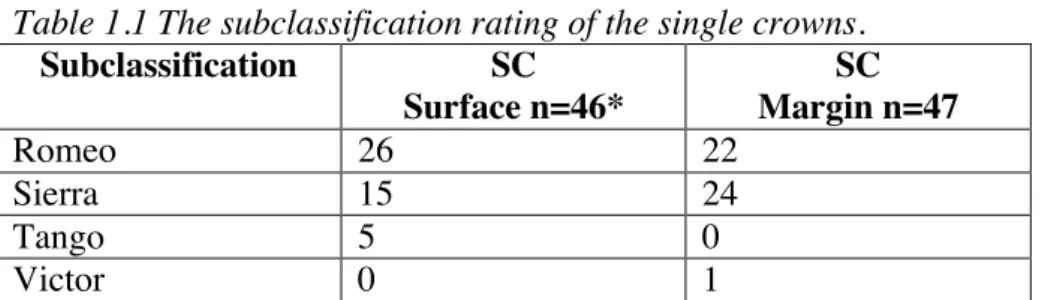
The 47 single crowns examined during the study had a mean age of 36 months and a median age of 29 month (range 10 to 83 months). Table 1.1 lists a summary of each subclassification given to the crowns. Overall, the results showed that the surfaces and margin held a high standard, 89% of the crowns had the surface subclassification “Romeo” or “Sierra” and 98% had the margin subclassification “Romeo” or “Sierra”. Table 1.2 lists the overall assessment of the single crowns, 55 % had the overall assessment “successful”, 43 % had the overall assessment “survival” and 2% had the overall assessment “failed”.
Eight of the crowns that were assessed as “survival” had superficial chip off fractures located in the veneering porcelain and two had major fractures/mechanical wear exposing the
underlying metal. One crown accounted for the 2% assessed as “failed”, this was due to loss of retention. The crown was recemented at two occasions without successful results. The responsible clinican hence decided to remake the crown.
Table 1.1 The subclassification rating of the single crowns.
Subclassification SC Surface n=46* SC Margin n=47 Romeo 26 22 Sierra 15 24 Tango 5 0 Victor 0 1
*One SC was never clinically examined, because the patient stated that the construction had been removed due to caries. Therefore the margin was automatically assessed as Victor and the surface was never examined.
Table 1.2 Summary of the number success, survival and failed single crowns.
Overall assessment SCs n =47
Success 20
Survival 26
Single crown abutment teeth
The results regarding the periodontal status showed that nine SC abutment teeth (20%) had no periodontal pathology and their contralaterals showed similar status.
The majority (54%) of the SCabutment teeth had a positive bleeding on probing with no pathological pockets. Eight of their contralateral had positive bleeding on probing and six even had pathological pockets (with a range of 4-5 mm deep pockets). This demonstrated that 56% of the contralaterals had the same periodontal status or worse compared to the abutment tooth. The remaining contralaterals 44% had no periodontal pathology.
17% of the SC abutment teeth had pathological pockets with a range of 4-5 mm. Five of their contralaterals had positive bleeding on probing but no pathological pockets and three
contralaterals had pathological pockets >4 mm. This demonstrated that 62% of the
contralaterals had a healthier periodontal status compared to their SC abutment teeth and 38% had the same or worse periodontal status.
Four of the SC abutment teeth had pathological pockets ≥6 mm. These four accounted for 9% of the total SC abutment teeth. One of their contralateral had positive bleeding on probing but no pathological pockets and three had pathological pockets with a range of 4-5mm. These results demonstrated that 100% of the contralaterlas had healthier periodontal status compered to the corresponding abutment.
Overall the combined result showed that 43% of the SC abutment teeth had worse periodontal status compared to their contralateral.
Results from examining the cariological activity of the SC abutment teeth showed that none of the teeth had caries and the same results were demonstrated for the contralaterals.
Regarding fractures, all the teeth (abutments and contralaterals) were intact.
Fixed dental prosthesis evaluation
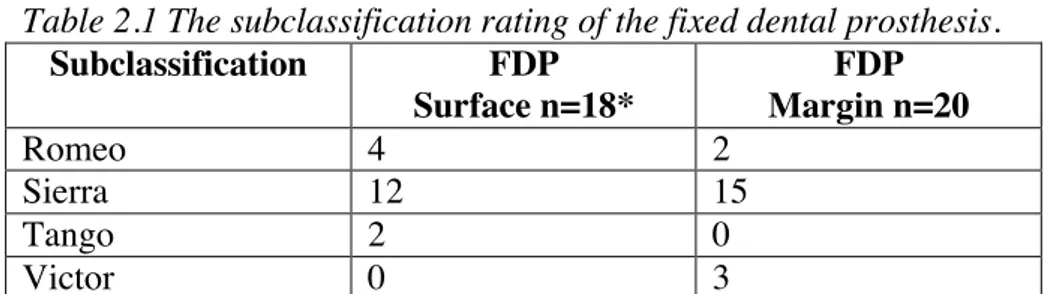
The FDPs represent a minority in this study. The 20 FDPs that where included had a mean age of 35 month and a median age of 35 month (range 16 to 84 month). Table 2.1 lists a summary of each subclassification given to the FDPs, 89% had the surface subclassification “Romeo” or “Sierra” and 85% had the margin subclassification “Romeo” or “Sierra”. Table 2.2 lists the overall assessment of the FDPs, 15 % had the overall assessment “successful”, 70 % had the overall assessment “survival” and 15% had the overall assessment “failed”.
Four of the FDPs that were assessed as “survival” had superficial chip off fractures located in the veneering porcelain and two had major fractures/mechanical wear exposing the
underlying metal. Three FDPs accounted for the 15% assessed as “failed”. This was due to margin discrepancy because of loss of the cement lock causing two FDPs to come off. The third FDP, which was a three-unit bridge with two abutment teeth, was however still in place but mobile. The distal abutment was no longer attached to the FDP but the mesial abutment had an intact cement lock which prevented the FDP from becoming detached completely.
Table 2.1 The subclassification rating of the fixed dental prosthesis. Subclassification FDP Surface n=18* FDP Margin n=20 Romeo 4 2 Sierra 12 15 Tango 2 0 Victor 0 3
*Two FDPs were completely detached and never clinically examined. Therefore the margins were automatically assessed as Victor and the surfaces were never examined
Table 2.2 Summary of the number success, survival and failed fixed dental prosthesis.
Overall assessment FDPs n=20
Success 3
Survival 14
Failed 3
Fixed dental prosthesis abutment teeth
The results regarding the periodontal status showed that two FDP abutment teeth (11%) had no periodontal pathology and their contralaterals showed similar status.
28% of the FDP abutment teeth had a positive bleeding on probing with no pathological pockets. Two of their contralateral had positive bleeding on probing and two even had pathological pockets (with a range of 4-5 mm deep pockets). The remaining 20% had no periodontal pathology, this figure accounted for one of the contralaterals.
The majority of the FDP abutment teeth (56%) had pathological pockets, with a range of 4-5 mm deep pockets. Four of their contralaterals had the same periodontal status or worse and six of their contralaterals had a healthier periodontal status. These contralaterals accounted for 40% and 60% respectively.
One (5%) of the FDP abutment teeth had pathological pockets >6 mm, in this case the contralateral also exhibited a pathological pocket >6 mm.
Over all the combined result showed that 22% of the FDP abutment teeth had worse periodontal status compared to their contralateral.
Results from examiningthe cariological activity of the FDP abutment teeth showed that none of the teeth had caries but four of their contralateras had active caries lesions. Regarding fractures, all the abutment teeth were intact but three of their contralaterals had visual fractures.
The patient’s evaluation
All patients that were clinically examined expressed satisfaction concerning their restoration.
Non-response analysis
Based on the scan of technican bills and the patient's dental records a total of 67 patients were identified as potential participants in the study. From this group 21 individuals did not
participate in the study, this outcome represented 31% of all patients.
In the none-participating group 11 individuals expressed that they were not interested and did not want to take part in the study. Two individuals did not attend their appointments and did not answer when trying to contact them with purpose of booking a new appointment. Four individuals could not be reached by phone and no other phone numbers were found when various web browsers for contact details were used. Four individuals were interested in the study but could not attend during the specified period set for the examinations.
All together the 21 individuals, that did not participate in the study, had 31 restorations. This represented 32% of all restorations matching the inclusion and exclusion criteria.
17 were SCs and 14 were FDPs. From the patient's dental record the following information was obtained: Three FDPs had been modified because of caries, one FDP had to be
recemented and among the remaining 27 restorations there were no further comments in the patient's dental record.
The 31 restorations that were not included in the study had a mean age of 35 month and a median age of 35 month (range of 23 to 53 month). The mean age of the SCs was 34 month and the median age was 35 month (range of 23 to 53 month) while the mean age of the FDPs was 36 month and the median age was 36 month (rang of 23 to 51 month).
Discussion
Choice of material
A good health care means, among other thing, good quality but also affordability and time effectiveness for the dentist and the patient, both direct and indirect. The importance of choosing an optimal material in the clinical situation is of importance for all parties involved; the society, clinic, dentist and the patient. Replacing biological material with artificial
restorations automatically creates a future need of dental health care and by using materials that are not optimal for its purpose the future need of dental health care is likely to be further increased. By choosing sustainable, biocompatible and easily produced SC and FDP
materials, hopefully high efficiency and high success/survival rates can be obtained. Revisits and remakes will be minimized and the patient remains satisfied.
Since the Swedish government subsidies a big part of the treatment and material cost for SC and FDP therapies, a drive to make profitable investments is therefor important from a society perspective. In addition, prolonged treatments due to remakes can lead to increased absence from work or school, with increasing cost for the individual as well as the society.
Trough knowledge of material properties and success rates the dental treatments can be more effective benefitting both the clinic and the dentist. The dentist can also feel more secure during discussions about materials with the patient and the patient can feel that he or she has the knowledge to make a well-informed decision. Seen from a patient-orientated point of view, a bad choice of material could lead to fractured restorations resulting in physical stress, aesthetic dysfunction and/or more bothersome treatment situations at the dentist. Studies like these could facilitate the choice of dental materials for SCs and FDPs in the clinical situations and therefor benefit all parties involved (the society, clinic, dentist and the patient). The Swedish dental health care law emphasizes the fact that the dental health care should be of good quality and under equal conditions for all citizens, therefore, long time follow up studies play an important roll in reaching this national goal through distributing information to the practicing clinician.
The Swedish Dental Association has nine ethical guidelines from year 2014, where the first and second guidelines could be of particular interest concerning studies such as the present. They state the importance of the patients’ health and wellbeing and the dentists’ obligation to work according to science and proven experience. This concludes the importance of the dentist keeping up to date with the current science, in which this study could be a contributing factor.
Many of today’s dentists feel reluctant to use titanium-ceramic SCs and FDPs. This is due to the reputation implying that these restorations easier become a subject of ceramic fractures, so-called chip off fractures, affecting the success, survival and failure rate. According to some studies this reputation could be confirmed (21,22). Depending on the technique used to
produce the titanium-ceramic restorations the quality varies, since the manufacturing process is sensitive due to the titanium’s highly reactive and allotropic properties (23-25). When these parameters are taken into consideration studies have shown that an acceptable bonding
strength between the titanium and the veneering ceramic and satisfying ceramic veneering properties can be accomplished (2,13,16,26-28). This suggest that the choice of the dental technician lab used for producing a titanium-ceramic restoration is of high significance with regards to their experience of working with titanium. Therefor an open dialogue with the
dental technician is believed to be a beneficial approach in order to inquire how they experience working with titanium and what sort of method they use. This way a suitable choice can more easily be made.
Method
The CDA criteria were chosen as a base because a great amount of effort was put into their development, in order to reflect clinical significance. Today they are seen as an established method when evaluating the clinical quality of dental restorations and are therefore frequently used in clinical trials. However, because of the present research question and due to the fact that the criteria’s original purpose was to evaluate the quality of amalgam and resin
restorations a modified version of the CDA criteria was used as a quality evaluation system in this present study (19,20).
Through well elaborated, well written and easily understandable criteria the intention with this method was to develop a quality evaluation system as objective as possible. To further reduce the subjectivity, the examinations were preformed by two students who went through a calibration process prior to the initiation of the project. If their evaluation at some point did not correlate a mutual agreement was reach after a consensus discussion and joint re-examination. However in the end the examinations were performed by individuals, thus the result would always reflect a certain amount of subjectivity.
Patients
The patient clientele at the Faculty of Odontology, Malmö University, is not always
representative for the general population. Because of the time-consuming treatment sessions, multiple appointments and attractive costs, the student clinic attracts a certain range of
individuals, for example the older population that is no longer working. This gives the student clinic a more homogeneous patient group, which dose not represent the same variation seen in the SwedishPublic Dental Service, “Folktandvården”.
A source of possible error could be the fact that the patient base was selected though dental technician bills stored in binders. This limited the material, because there wasno access to dental technician bills from before year 2011 and the fact that there was no guarantee that all dental technician bills were located in their binder.
Results
The results showed that the restorations overall presented high survival rates and good quality. 55% of the SCs and 15% of the FDPs were assessed as successful. Looking only at the success rates, especially for the FDPs, the percentage may seem low, but when the survival rates also are included the picture changes. 43% of the SCs and 70% of the FDPs were assessed as survival. Furthermore, despite the assessments of the research, all the patients with these restorations were satisfied, which in it self should be considered as
success. Even patients with restorations showing metal exposure were satisfied and did not wish for adjustments or remake. Seen from the patients’ point of view the results could instead be interpreted as a success rate of 98% for the SCs and 85% for the FDPs.
Regardless how the results are interpreted it is obvious that the SCs have a higher success rate compared to the FDPs. This could be explained by FDPs being exposed to other loading conditions and the fact that the treatment is more complex. Therefore, more units increase the risks and potentially affect the overall quality. It could also be due to the fact that the
individuals in need of multiple unit FDPs also are in need of a more extensive oral health care. If this extensive need is a result of risk behaviour the FDP will be placed in a more challenging environment, which could impair the overall success and survival rate.
The present success and survival rates are comparable to other previously made prospective studies. According to three different studies the success rate has shown to vary between 63%-76% and the survival rate between 81%-97% after approximately three years (8,29,30). One of these studies also showed that between three and six years the success rate decreased from 76% to 59% (29).
The one SC (2%) and two out of the three FDPs (15%) that were assessed as “failed” where, as mentioned in the “Material and Method”, never examined by the two students. This could be seen as a source of possible error due to the fact that the information that led to the over all evaluation “failed” were obtained only from the patients dental records.
Looking at the results regarding the restorations surfaces, 21% of the SCs and 33% of the FDPs had some kind of fracture in the veneering ceramic (technical complication). More specifically 17% (eight SCs) had chip off fractures within the veneering ceramic and 4% (two SCs) had fractures causing metal exposure while 22% (four FDPs) had chip off fractures within the veneering ceramic and 11% (two FDPs) had fractures causing metal exposure. Similar frequency of chip off fractures can be seen in other studies such as the prospective study by Lövgren et al (17). Another study also reported that the technical complications are the main problem compared to the biological complications (31).
The results indicate an overall high and acceptable success and survival rate for the
restorations, verifying the first hypothesis. The second hypothesis is verified concerning FDPs but only partially verified concerning SCs. The SCs hade a higher success rate than survival rate. But most SCs that were assessed as “survival” received the rating due to complications in the ceramic veneer.
Today there are no criteria defining acceptable survival. A desirable outcome is of course 100% survival, but this is not realistic when different parameters are taken into consideration for a construction in use. Some of the parameters that have to be taken into consideration include; the sort of environment the restoration is installed in together with function and aesthetics, which requires certain material properties and restoration appearances.
Metal-ceramic restorations with the highest survival rates are today those with gold alloys, with a survival rate of 95% after 5 years. This is seen as the golden standard and therefor as excellent survival. This studie’s result do not reach an excellent survival rate but is still considered acceptable due to the advantages achieved when using titanium-ceramic restorations (biocompatibility and costs) and due to the fact that the majority of the
This also tells us that the use of titanium-ceramic constructions in dental care is a
cost-effective treatment for patients and the society. The reason that the SCs results did not classify as excellent survival, were due to the age range of 10 to 83 months (not limited to a minimum of five years).
The clinical examinations were performed by two dental students during their eight semester (April 2016) and because of their lack of experience with the clinical appearance of chip off fractures, the outcome of the surface evaluation could have been affected.
Earlier in the discussion, the importance of choosing a competent dental technician lab in order to achieve successful clinical outcomes is mentioned. This is a variable that has not been taken into consideration in this study, which could reflect on the results for the margin and surface evaluation. The framework can generally be produced using two methods,
CAD/CAM milling or casting. Studies have showed that CAD/CAM milled titanium-ceramic restorations both exhibit a more accurate fit and a higher titan-ceramic bonding (11,26). Studies have also shown that using bonding agents enhances the bond straight between the titanium and ceramic (32).
The present study is a retrospective study involving many different factors (dentists, students and dental technican labs) and only a few inclusion criteria. This could be seen as weaknesses but also as strengths due to the fact that the generous uptake of constructions could reflect the reality from a different perspective, compared to other more controlled studies. Because the patient base was restricted, relatively young constructions were included. The youngest construction hade only been installed for 10 month, resulting in the inclusion criteria used for this study (Patients having received titanium-ceramic restorations more than 10 months ago, at the Faculty of Odontology, Malmö University).
The biological and technical complications that in general are most frequently seen
concerning abutment teeth are endodontic complications, periodontal pathology, caries and fractures (17,31,33).One study by Jokstad A (31) showed that the risk of restoration loss over 10 years caused by caries was 2.6%, abutment fracture 2.1% and periodontitis 0.5%. The same study showed that the most common complications of abutment teeth were caries (9.5%) and/or loss of pulp vitality (10%). In this present study periodontal pathology, caries and fractures were evaluated. Looking at the periodontal status of the abutment teeth, the results showed that 80% of the SCs and 89% of the FDPs had various degree of periodontal pathology. The majority of the SCs had positive bleeding on probing with no pathological pockets while the majority of the FDPs demonstrated worse periodontal status exhibiting pathological pockets, with 4-5mm probing depth. This suggests that it is more technical challenging to keep a good oral hygiene around multiple unit FDPs.
When comparing the periodontal status of the restoration abutment teeth with that of their contralateral the results showed that:
• 43% of the SC abutment teeth had worse periodontal status than their contralateral • 22% of the FDP abutment teeth had worse periodontal status than their contralateral. This could implicate that the dental team has a preconceived idea that oral hygiene around multiple unit FDPs is more difficult and therefor FDP therapy might unconsciously result in more thorough oral hygiene instructions.
Regarding caries and fractures, no significant findings where made. All restoration abutment teeth were intact and caries-free. Three of the FDP contralaterals had caries, four of the FDP
contralaterals had fractures and all of the SC contralaterals were intact. This could corroborate the theory that patients with multiple unit FDPs have an extensive need of oral health care and more often have risk behaviour.
Bias Non-response analysis
The mean age of the SCs in the non-participating group was 34 months and 36 months in the participating group. The FDPs in the non-participating group hade a mean age of 36 months while the FDPs of the participating group had a mean age of 35 months. The mean age of the non-participating group and the participating group slightly differ but the difference is not seen as significant. On the other hand the distribution of SCs and FDPs could be interpreted as more significant. In the non-participating group the SCs represented 55% and the bridges 45% while in the participating group the SCs represented 70% and the FDPs 30%.
After considering these factors and weighing in the fact that the non-participating group only represented 31% of the total patient base, the authors believe that the result in this present study is representative for the patient clientele at the Faculty of Odontology, Malmö University and therefor not bias.
Ethics
As mentioned in the “Material and Method”, no ethical review was needed because of the non-invasive nature of the clinical examination. All patients also signed a form of consent prior to the examination.
Conclusion
Within limits of this study the following conclusions were made:
• The results indicate an overall high and acceptable success and survival rate for the restorations submitted to patients at the Faculty of Odontology, Malmö University. But the single crowns had a higher success rate compared to the fixed dental prostheses.
• Chip off fractures of the veneering porcelain was the single most common
complication noted. But patient satisfaction was high despite chip off fractures of the veneering porcelain
• The success rate for titanium-ceramic fixed dental prostheses, submitted to patients at the Faculty of Odontology, Malmö University, was lower than the survival rate due to complications in the ceramic veneer. Concerning the single crowns the success rate was higher than the survival rate. But most single crowns that were assessed as “survival” received the rating due to complications in the ceramic veneer.
Appendix 1: Information letter
Informationsblad
Klinisk undersökning och kvalitetssäkring av protetiska konstruktioner d.v.s. kronor och broar.
Under de senaste åren har det skett en stor utveckling inom tandersättningar. I samband med utvecklandet av nya material som ingår i tandersättningar som kronor och broar uppkommer ett behov av utvärdering av hur dessa fungerar i munnen. I dagsläget finns det mycket
kunskap om dessa material från laboratoriestudier men begränsad kunskap om hur de fungerar kliniskt över tid. Om du väljer att delta i den planerade studien så bidrar du till ett
examensarbete på tandläkarutbildningen i Malmö.
Vår studie ämnar undersöka och kvalitetssäkra protetiska konstruktioner utförda i titan-porslin på Tandvårdshögskolan i Malmö. Självfallet är undersökning kostnadsfri och dessutom
erbjuds det en kostnadsfri professionell tandrengöring som tack.
Hur går studien till?
Du kommer att bli kallad till Tandvårdshögskolan i Malmö, våren 2016, där du först får fylla i en samtyckesblankett. Därefter utför två tandläkarstudenter (som går termin 8) en klinisk undersökning av din krona/bro. Besöket avslutas med en frivillig professionell tandrengöring. Du som patient informeras om eventuella fynd. Vi erbjuder dock ingen behandling för dessa (eventuell sjukdom/skada vid den protetiska konstruktionen) men hjälper dig vidare till fortsatt vård.
Finns det några risker?
Det finns inga risker med att delta i studien.
Hantering av data
Ansvariga för personuppgifterna är Malmö Högskola. Alla uppgifter kommer att hanteras i enighet med Personuppgiftslagen (1998:204). Dokumentation från undersökningen kommer att avkodas, vilket gör dig som person anonym i studien. Resultatet kommer att presenteras i ett examensarbete. Eventuella fynd som presenteras kommer inte att kunna kopplas till någon enskild individ.
Försäkring
Den vanliga patientförsäkringen gäller för studien.
Valfrihet
Det är frivilligt att delta i studien. Man kan välja att avbryta när som helst utan att ange orsak och utan att det påverkar övrig behandling på Tandvårdshögskolan.
Ansvarig
Huvudansvarig för studien är övertandläkarna Christel Larsson. Tel: 040-665 8506 (receptionen, Oral protetik)
Appendix 3: Research Journal
Forskningsjournal
Klinisk utvärdering av överlevnaden hos mk-konstruktioner baserade på titan
Kodnummer Kron/bro-placering i bettet Dagens datum Insättningsdatum av konstruktion Tandtekniskt lab.
vProtetisk konstruktion
Yta:
Bedömare 1 Bedömare 2Romeo Slät yta, ingen irritation av omgivande vävnad.
Sierra Lätt ytråhet och/eller lätt ojämnhet som kan justeras. Små frakturer som endast ligger i ytkeramen.
Tango Grov ytråhet, gropig, ojämn yta som kan justeras/repareras. Större fraktur som ger metallblotta.
Victor Gropar, ojämnheter eller frakturer som inte kan justeras/repareras.
Marginal anslutning:
Bedömare 1 Bedömare 2
Romeo Inga synliga tecken på spalt mellan tand och krona. Sonden hakar inte upp sig vid sondering.
Sierra Synlig spalt och/eller sonden hakar upp sig vid sondering.
Tango Cementunderskott där sonden kan föras in i spalt mellan tandsubstans och krona.
Victor Cementlås släppt, mobil eller tappad konstruktion.
vStödtand
Kariesförekomst ja/nej, Yta: m-mesialt, d-distalt, p-palatinalt, l-lingualt, b-buccalt
Bedömare 1 Kontralateral Bedömare 2 Kontralateral Karies
Yta
Fraktur ja/nej
Bedömare 1 Kontralateral Bedömare 2 Kontralateral Fraktur
Parodontala förhållanden, fyra ytorja/nej
Bedömare 2 Konralateral Gingivit Fickor >3mm + blödning Fickor >6mm + blödning
Gingivit = Blödning på minst 1 av 4 ytor med fickor under 3mm
Appendix 4: Results
Resultat
Kodnr: Månader: Krona/bro: Labb Yta Marginal Total bedömning
2.1 24 B D-syd R V F Victor - var från början
en bro 34-35-37. Dock har den bakre delen avlägsnas pga karies, cementlåset har även släpt på den nuvarande delen på en av stödtändena.
33.1 53 B D-syd 0 V F Tappad 2016-03-29
7.3 20 B T-dont 0 V F Avl pga porslinsfrakturer.
Porslinsfraktur 150220à lagad. Ny fraktur under endobeh. Bron avl 151013. Ny bro i MK i ti keram. I övrigt inga problem.
21.1 35 B Cervident R S Su
9.3 28 B T-dont R S Su
6.1 37 B D-syd R R Su
18.2 17 B Ö-stad S S Sv
19.2 29 B T-dont S S Sv Chip off, ocklusalt.
27.1 40 B Ö-stad S S Sv
27.2 40 B Ö-stad S R Sv
27.3 40 B Ö-stad S S Sv
30.1 47 B T-dont S S Sv Chip off
ocklusalt/palatinalt.
37.1 16 B T-dont S S Sv
37.2 23 B T-dont S S Sv
44.1 37 B D-syd S S Sv Chip off ocklusalt. Kronförsedd 13 à stort slitage med metallblotta. Generellt parodskadat bett.
46.1 35 B D-syd S S Sv En Chip off buckalt. Kolla Foto med Christel. Pat biter precis här på kontruktionen.
Kronförsedd konralateral 34. Foto taget.
7.2 24 B ?? S S Sv
9.4 23 B T-dont S S Sv
11.1 48 B D-syd T S Sv Tango pga metallblotta, kraftiga attritionsfasetter 43,33
35.2 84 B D-syd T S Sv Tango pga metallblotta, mycket slitage av keramen med
flerametallblottor, samma ses hos bron i Q1.
47.1 10 K T-dont 0 V F Recementering 121204. Recementering 121218. Pga bristande approximala kontakter görs kronan om helt 130906, ny konstruktion i CoCr 12.2 17 K T-dont R R Su 14.2 23 K T-dont R R Su 24.1 23 K T-dont R R Su 25.1 35 K Cervident R R Su 26.1 28 K T-dont R R Su 28.1 13 K D-syd R R Su 28.2 13 K D-syd R R Su 31.1 23 K T-dont R R Su 32.1 36 K T-dont R R Su 36.1 29 K T-dont R R Su 38.1 53 K T-dont R R Su 41.1 26 K T-dont R R Su 8.3 41 K T-dont R R Su 10.1 25 K T-dont R S Su 13.1 24 K Ö-stad R S Su 15.1 28 K T-dont R S Su 16.1 28 K T-dont R S Su 19.1 24 K Cervident R S Su 20.1 48 K D-syd R S Su 22.1 23 K T-dont R S Su 29.1 71 K D-syd R S Su 29.2 65 K D-syd R S Su 36.3 28 K T-dont R S Su 39.1 24 K T-dont R S Su 9.1 40 K D-syd R S Su 36.2 28 K T-dont R S Su 12.1 23 K T-dont S S Sv
14.1 59 K T-dont S R Sv Chip off palatinalt.
17.1 35 K T-dont S R Sv
18.1 25 K Ö-stad S S Sv
23.1 26 K T-dont S S Sv
29.3 54 K D-syd S S Sv Chip off buckalt.
3.1 46 K T-dont S S Sv Chip off buckalt.
35.1 35 K T-dont S R Sv
4.1 41 K T-dont S R Sv
43.1 28 K Ö-stad S R Sv Mkt ytlig chip off i porslinet palatinalt. OBS konstruktionen är en urtagskrona.
Kontralateral: 12 då 13 saknas. Generellt restaurerat bett.
45.1 35 K T-dont S S Sv Distalt Chip off i keram. Foto taget
5.1 52 K D-syd S S Sv
7.1 22 K S S Sv
9.2 37 K D-syd S R Sv
1.1 47 K D-syd T S Sv Liten fraktur som ligger
mesialt, chip off,samt grov ytråhet.
34.1 36 K T-dont T R Sv Tango pga metallblotta, ej fraktur, snarare slitage.
40.1 35 K D-syd T S Sv Tango pga metallblotta som ser ut som slitage.
42.1 27 K T-dont T R Sv Chip off mesioocklusalt, endast i poslinet. Kontralateral: Tand.
8.1 83 K T-dont T R Sv
Total bedömning kronor
Success 26
Survival 20
Failed 1
Total bedömning broar
Success 3
Survival 14
Failed 3
Total bedömning: Alla
Success 23
Survival 40
Failed 4
Alla konstruktioner, ålder Månader: År:
Medel: 35,14925373 2,929104478
Median: 29 2,416666667
Max: 84 7
Min: 10 0,833333333
Kronor, ålder Månader År
Medel : 32,46808511 2,705673759
Median: 28 2,333333333
Max: 84 7
Min: 10 0,833333333
Broar, ålder: Månader År
Medel: 41,45 3,454166667
Median: 35,5 2,958333333
Max: 83 6,916666667
Broar, subklassificering Antal (st) Romeo yta: 4st Sierra yta: 12st Tango yta: 2st Victor yta: 0st Romeo marginal: 2st Sierra marginal: 15st Tango marginal: 0st Victor marginal: 3st Teckenförklaring B-bro K-krona R-romeo S-sierra T-tango V-victor 0-ej us Su-Success Sv-Survival F-failed
Kronor, subklassificering Antal (st)
Romeo yta: 26st Sierra yta: 15st Tango yta: 5st Victor yta: 0st Romeo marginal: 22st Sierra marginal: 24st Tango marginal: 0st Victor marginal: 1st
Appendix 5: Non-response analysis
Non-response analysis
Kodnummer Placering i
bettet /lab.
Varför de ej deltagit Journalanalys Bro/
Kron a
Ålder i månader
B1.1 46-47 / D-syd Åb, utomlands under
aktuell period
inga övriga kommentarer i journalen B 36
B2.1 13-16 /
T-dont
Vill ej delat, ej varit här sedan cementering
ej varit här sedan cementering B 34
B3.1 14-26 /
T-dont
Åb pga av
lunginflammation, vill ej ha ny tid, pat har ingen bil kan ej ta sig in
från början 14-26, 26 dålig prognos från börjar, sedan karies. 150420 separering endast 14-23 kvar.
B 35
B4.1 15 / Ub. Vill ej delta pat nöjd, inga fler kommentarer ang
konstruktionen K 40
B4.2 24-26 Ub. Vill ej delta pat nöjd, inga fler kommentarer ang
konstruktionen B 40
B5.1 12-22 . Utomlands under
aktuell period (mars-juni)
Från början 15-22.14113 är följande reg som
saknad pga av karies 13, 14, 15. B 51
B6.1 36 /ö-stad Vill ej delta inga övriga kommentarer i journalen K 24
B7.1 16 / t-dont Åb. Mkt på jobbet ända
fram till juni
inga övriga kommentarer i journalen K 41
B7.2 36 / t-dont Åb. Mkt på jobbet ända
fram till juni
inga övriga kommentarer i journalen K 40
B8.1 16-12 / ö-stad Vill ej delat inga övriga kommentarer i journalen B 34
B9.1 24 / T-dont Vill ej delta inga övriga kommentarer i journalen K 29
B9.2 12 / T-dont Vill ej delta inga övriga kommentarer i journalen K 35
B9.3 25 / T-dont Vill ej delta inga övriga kommentarer i journalen K 29
B9.4 11-23 /
T-dont
Vill ej delta inga övriga kommentarer i journalen B 35
B10.1 24-26 /
T-dont
Vill ej delta inga övriga kommentarer i journalen B 23
B11.1 14 / T-dont Vill ej delat inga övriga kommentarer i journalen K 24
B11.2 24 / T-dont Vill ej delat inga övriga kommentarer i journalen K 24
B12.1 12 / T-dont Åb pga av sorg. Vill ej
delta
inga övriga kommentarer i journalen K 29
B13.1 44-47 /
T-dont
Ub. Vill ej delta lossnade, recementerades 140213 B 28
B14.1 33-45 /
T-dont
Vill ej delta kronor ök är urtagskronor, 43 chip-off metalblotta 130624, 32b chip-off metallblotta 140618, 45 140922 chip-off, puts, pat ej nöjd --> reparation me komposit, pat nöjd. Bro frakturerar 151127, avlägsnar 41-45 (karies) av bron.
B 40
B14.2 15 / T-dont Vill ej delta kronor ök är urtagskronor, 43 chip-off
metalblotta 130624, 32b chip-off metallblotta 140618, 45 140922 chip-off, puts, pat ej nöjd --> reparation me komposit, pat nöjd. Bro frakturerar 151127, avlägsnar 41-45 (karies) av bron.
B14.3 13 / T-dont Vill ej delta kronor ök är urtagskronor, 43 chip-off metalblotta 130624, 32b chip-off metallblotta 140618, 45 140922 chip-off, puts, pat ej nöjd --> reparation me komposit, pat nöjd. Bro frakturerar 151127, avlägsnar 41-45 (karies) av bron.
K 40
B14.4 22 / T-dont Vill ej delta kronor ök är urtagskronor, 43 chip-off
metalblotta 130624, 32b chip-off metallblotta 140618, 45 140922 chip-off, puts, pat ej nöjd --> reparation me komposit, pat nöjd. Bro frakturerar 151127, avlägsnar 41-45 (karies) av bron.
K 40
B15.1 15 / T-dont Utomlands under
aktuell period
inga övriga kommentarer i journalen K 23
B16.1 33-35 / ö-stad Åb sjuk, ny tid bokad.
Åb igen, sjuk.
inga övriga kommentarer i journalen B 47
B17.1 22 / T-dont Åb inga övriga kommentarer i journalen K 53
B18.1 21 / D-syd Går ej att nå via tel,
troligen ej aktuella nr
inga övriga kommentarer i journalen K 37
B19.1 36 / Tic Går ej att nå via tel
(troligen ej aktuellt nr)
inga anmärkningar vid 1 års kontroll K 24
B20.1 23-26 / D-syd Går ej att nå via tel
(tutar alltid upptaget)
inga övriga kommentarer i journalen B 41
B21.2 45-47 /
T-dont
Går ej att nå via tel (troligen ej aktuellt nr)
inga övriga kommentarer i journalen B 40
B21.1 35-37 /
T-dont
Går ej att nå via tel (troligen ej aktuellt nr)
inga övriga kommentarer i journalen B 30
Bortfall antal individer
Utryckt att de ej vill delta: 11st Åb/Ub: 2st
Går ej att nå via tel: 4st
Kan ej delta under aktuell period: 4st
= Bortfallsanalys totalt 21 individer
Bortfall antal konstruktioner Kronor 17st
Broar 14st
= Totalt antal konstruktioner: 31st
Journalanalys
Inga kommentarer ang konstruktonen sedan cementering: 28st Har modifierats pga karies: 3st (endast broar)
References
(1) Tandförluster: en systematisk litteraturöversikt. Stockholm: Statens beredning för medicinsk utvärdering; 2010.
(2) Persson M, Bergman M. Metal-ceramic bond strength. Acta Odontologica 1996;54(3):160-165.
(3) A textbook of fixed prosthodontics: the Scandinavian approach. 2., [updat] ed. Stockholm: Gothia fortbildning; 2013.
(4) Anusavice KJ. Phillips' science of dental materials. 12th ed. St. Louis, Mo: Elsevier/Saunders; 2013.
(5) Wataha JC. Alloys for prosthodontic restorations. J Prosthet Dent 2002;87(4):351-363. (6) Riksrevisionen. Tandvårdsstöd för äldre. 2006;ISBN 91 7086 076 9.
(7) Bessing C. Cobolt-chromium alloys - excellent alternatives to high-gold alloys intended for metal ceramics / Kobolt-kromlegeringar - utmärkta alternativ till guldlegeringar för metallkeramik. Tandläkartidningen 2003(8):38.
(8) Boeckler AF, Lee H, Psoch A, Setz JM. Prospective observation of CAD/CAM titanium-ceramic-fixed partial dentures: 3-year follow-up. J Prosthodont 2010 Dec;19(8):592-597. (9) Per Haag. Porcelain veneering of titanium: clinical and technical aspects. Faculty of Odontology, Malmö University; 2011.
(10) Socialstyrelsen. Titan för odontologiska applikationer - Biologiska aspekter. 2010. (11) Haag P, Nilner K. Bonding between titanium and dental porcelain: a systematic review. Acta Odontol Scand 2010 May;68(3):154-164.
(12) Nilner K, Haag P. Questions and answers on titanium-ceramic dental restorative systems: a literature study. Quintessence Int 2007(1).
(13) Gilbert JL, Covey DA, Lautenschlager EP. Bond characteristics of porcelain fused to milled titanium. Dent Mater 1994 Mar;10(2):134-140.
(14) Socialstyrelsen. Oädla legeringar för metallkeramik: Basmetallegeringar. 2007;2007-123-39.
(15) Anusavice KJ. Phillips' science of dental materials. 12th ed. St. Louis, Mo: Elsevier/Saunders; 2013.
(16) Esquivel, J.F. ( 1,4,7 ), Chai, J. ( 2,5 ), Wozniak, W.T. ( 3,6 ). The physical properties of low-fusing porcelains for titanium. Int J Prosthodont 1996;9(6):563-571.
(17) Lovgren R, Andersson B, Carlsson GE, Odman P. Prospective clinical 5-year study of ceramic-veneered titanium restorations with the Procera system. J Prosthet Dent 2000 Nov;84(5):514-521.
(18) Boeckler AF, Lee H, Stadler A, Setz JM. Prospective observation of CAD/CAM titanium ceramic single crowns: a three-year follow up. J Prosthet Dent 2009 Nov;102(5):290-297. (19) Ryge G, Snyder M. Evaluating the clinical quality of restorations. J Am Dent Assoc 1973;87(2):369-377.
(20) Ryge G. Editorial: Evaluation of clinical quality and professional performance. J Dent Educ 1975;39(9):582-583.
(21) Moldi AI, Bhandari KS, Nagral S, Kulkarni P, Deshpandey S. Effect of sandblasting on fracture load of titanium ceramic crowns. Journal of Indian Prosthodontist Society
2015;15(3):224-228.
(22) Haag P, Andersson M, Nilner K, Derand T. Porcelain bonding to titanium with two veneering principles and two firing temperatures / Bindning mellan porslin och titan med två olika påbränningsprinciper och vid två olika temperaturnivåer. Swed Dent J 2013(3):143. (23) Adachi M, Mackert JR, J., Parry EE, Fairhurst CW. Oxide adherence and porcelain bonding to titanium and Ti-6Al-4V alloy. J Dent Res 1990 06;69(6):1230-1235.
(24) Low D, Sumii T, Swain M. Thermal expansion coefficient of titanium casting. J Oral Rehabil 2001 03;28(3):239-242.
(25) Togaya T, Suzuki M, Tsutsumi S, Ida K. An application of pure titanium to the metal porcelain system. Dent Mater J 1983;2(2):210-219.
(26) Lee E, Jun S, Park E, Wright RF. Comparative study of the shear bond strength of various veneering materials on grade II commercially pure titanium. Journal of Advanced Prosthodontics 2015;7(1):69-75.
(27) Leinfelder KF. Porcelain Esthetics for the 21st Century. J Am Dent Assoc 2000;131:47S-51S.
(28) Garbelini WJ, Henriques GEP, Troia Junior M, Mesquita MF, Dezan CC. Evaluation of low-fusing ceramic systems combined with titanium grades II and V by bending test and scanning electron microscopy. J Appl Oral Sci 2003 12;11(4):354-360.
(29) Hey J, Bensel T, Boeckler AF, Beuer F. Metal-ceramic-fixed dental prosthesis with CAD/CAM-fabricated substructures: 6-year clinical results. Clin Oral Investig 2012:1-5. (30) Dražić J, Dražić M. A two-year retrospective evaluation of titanium and cobalt-chromium metal- ceramic fixed dental prostheses. 2013.
(31) Jokstad A. After 10 Years Seven out of Ten Fixed Dental Prostheses (FDP) Remain Intact and Nine out of Ten FDPs Remain in Function Following Biological and Technical Complications That Have Been Repaired. Journal of Evidence-Based Dental Practice 2010;10(1):39-40.
(32) Ye J, Ye X, Chang S, Liu L, Lin S, Zhang Y. Effect of silica coating on the bond strength of milled pure titanium to dental porcelain. Eur J Oral Sci 2016;124(5):498-503.
(33) Pjetursson, B.E, Brägger, U, Lang NP, Zwahlen M. Comparison of survival and
complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res 2007;18:97-113.