MALMÖ UNIVERSITY 205 06 MALMÖ, SWEDEN isbn 978-91-7104-603-1 (print)
isbn 978-91-7104-604-8 (pdf) issn 0348-6672
GUDRUN
EDMAN TYNELIUS
ORTHODONTIC RETENTION
Studies of retention capacity, cost-effectiveness
and long-term stability
GUDRUN EDMAN T YNELIUS MALMÖ UNIVERSIT Y 20 ORTHODONTIC RETENTION
Swedish Dental Journal, Supplement 236, 2014
SWEDISH DENT AL JOURN AL, SUPPLEMENT 236, 20 1 4. DOCT OR AL DISSERT A TION IN ODONT OL OG Y
Swedish Dental Journal, Supplement 236, 2014
© Copyright Gudrun Edman Tynelius, 2014
Illustrations: Gudrun Edman Tynelius och Lars Leonardsson ISBN 978-91-7104-603-1 (print)
GUDRUN EDMAN TYNELIUS
ORTHODONTIC RETENTION
Studies of retention capacity, cost-effectiveness
and long-term stability
Department of Orthodontics
Faculty of Odontology
Malmö University, Sweden 2014
This publication is also available at: www.mah.se/muep
CONTENTS
PREFACE ... 9 ABSTRACT ... 10 Papers I and II ...10 Paper III ...11 Paper IV ...11Key conclusions and clinical implications ...11
POPULÄRVETENSKAPLIG SAMMANFATTNING ... 13
Avhandlingen baseras på fyra studier: ...13
Konklusioner av delarbete I och II: ...13
Konklusion av delarbete III: ...14
Konklusion av delarbete IV: ...14
Klinisk betydelse ...14
ABBREVIATIONS AND DEFINITIONS ... 16
INTRODUCTION ... 17
Background ...17
Prevalence ...18
Evidence-based healthcare ...18
Methodology ...19
Economic evaluation in healthcare ...19
Retention methods ...20 SIGNIFICANCE ... 22 AIMS ... 23 Paper I ...23 Paper II ...23 Paper III ...23 Paper IV ...23 HYPOTHESES ... 24 Paper I ...24 Paper II ...24 Paper III ...24 Paper IV ...24
MATERIALS AND METHODS ... 25
Subjects ...25
Papers I, II, III and IV ...25
Ethical considerations and consent ...27
Randomization ...27 Methods ...28 Papers I, II and IV ...28 Paper III ...31 Statistical analysis ...33 RESULTS ... 34
Paper I – one year of retention ...34
Paper II – two years of retention ...35
Paper III – Cost-minimization analysis ...37
Societal costs for scheduled appointments ...38
Paper IV – Long-term effects and stability ...38
Maxilla T0-T3 (Table 4) ...40
Mandible T0-T3 (Table 5) ...42
Overbite and overjet T0-T3 (Table 6) ...44
DISCUSSION ... 46 Relapse ...46 Methodological aspects...49 Papers I, II and IV ...49 Paper III ...52 Retention methods ...53 Vacuum-formed retainer (VFR) ...53 Positioner (P) ...54 Canine-to-canine retainer (CTC) ...54 Stripping (S) ...55 Late adolescence ...55 Success or failure? ...56 Ethical considerations ...56 Future studies ...57 CONCLUSIONS ... 58 ACKNOWLEDGEMENTS ... 59 REFERENCES ... 61
PREFACE
This thesis is based on the following papers, which are referred to in the text by their Roman numerals:
I. Edman Tynelius G, Bondemark L, Lilja-Karlander E. Evaluation
of orthodontic treatment after 1 year of retention – a randomized controlled trial. Eur J Orthod 2010; 32: 542-7.
II. Edman Tynelius G, Bondemark L, Lilja-Karlander E. A rando-mized controlled trial of three orthodontic retention methods in Class I four premolar extraction cases – stability after 2 years in retention. Orthod Craniofac Res 2013; 16: 105-15.
III. Edman Tynelius G, Lilja-Karlander E, Petrén S. A cost-minimization analysis of an RCT of three retention methods. Eur J Orthod August 2014; 36: 436-441.
IV. Edman Tynelius G, Petrén S, Bondemark L, Lilja-Karlander E. Five-year postretention outcomes of three retention methods – a randomized controlled trial. Eur J Orthod 2014; doi:10.1093/ ejo/cju063.
These papers are reprinted with kind permission from the copyright holders.
ABSTRACT
Retention strategies, cost-effectiveness and long-term stability of treatment outcome are essential aspects of orthodontic treatment planning.
The overall aim of this thesis was to compare and evaluate three different retention strategies, with special reference to short- and long-term clinical stability and cost-effectiveness. The approach was evidence-based, hence randomized controlled methodology was used in order to generate high levels of evidence.
This thesis is based on four studies:
Papers I and II are based on randomized controlled trials, evaluating the stability of treatment outcome after one and two years of retention, using three different retention strategies: a maxillary vacuum-formed retainer combined with a mandibular canine-to-canine retainer; a maxillary vacuum-formed retainer combined with stripping of the mandibular anterior teeth and a prefabricated positioner.
Paper III presents a cost-minimization analysis of two years of retention treatment.
Paper IV is based on a randomized controlled trial documenting the results five years post-retention.
The following conclusions were drawn:
Papers I and II
• From a clinical perspective, asssessment after one year of retention disclosed that the three retention methods were
• After two years of retention, all three retention methods were equally effective in controlling relapse at a clinically acceptable level.
• Most of the relapse occurred during the first year of retention; only minor or negligible changes were found during the second year.
• The subjects were grouped according to the level of
compliance (excellent or good). After two years of retention there was a negative correlation between growth in body height and relapse of mandibular LII in the group of subjects with excellent compliance. The group with good compliance showed a positive correlation (Paper II, Figure 3).
• After two years of retention, growth in body height, initial crowding and gender had no significant influence on mandibular LII (Paper II, Figure 4 and Table 4).
Paper III
• The cost minimization analysis disclosed that although the three retention methods achieved clinically similar results, the associated societal costs differed.
• After two years of retention, the vacuum-formed retainer (VFR) in combination with a canine-to-canine retainer (CTC) was the least cost-effective retention appliance.
Paper IV
• After five years or more out of retention, the three retention methods had achieved equally favourable clinical results.
Key conclusions and clinical implications
This study compared the short- and long-term outcomes of orthodontic retention by three different methods: a maxillary vacuum-formed retainer combined with a mandibular canine-to-canine retainer; a maxillary vacuum-formed retainer combined with stripping of the mandibular anterior teeth and a prefabricated positioner. All methods gave equally positive clinical results in both the short-term, i.e. after one and two years of retention, and in the long-term, five years or more post-retention.
After two years of retention, the level of compliance affected the retention treatment result. However, no such effect was shown for body height, the severity of initial crowding or gender.
Today, there is increasing emphasis on the importance of economic aspects of healthcare. Of the three methods evaluated in this study, the least cost-effective, after two years of retention, was a vacuum-formed retainer combined with a bonded canine-to-canine retainer.
The clinical implication of this finding is that in patients meeting the inclusion criteria, interproximal stripping of the mandibular anterior teeth, or the use of a prefabricated positioner, are highly appropriate alternatives to a mandibular bonded canine-to-canine retainer.
The overall conclusions are that there are a number of effective retention methods available and the clinician is not limited to routine use of a bonded mandibular canine-to-canine retainer. The most appropriate retention method should be selected on an individual, case to case basis, taking into account such variables as orthodontic diagnosis, the expected level of patient compliance, patient preferences and financial considerations.
POPULÄRVETENSKAPLIG
SAMMANFATTNING
Olika ortodontiska retentionsmetoders kapacitet att retinera ett behandlingsresultat, kostnadseffektivitet och långtidsstabilitet är viktiga delar när man planerar ortodontisk retentionsbehandling.
Det huvudsakliga syftet med denna studie var att jämföra tre retentionsmetoder med avseende på klinisk stabilitet på kort och lång sikt samt att göra en jämförande kostnadseffektivitetsanalys. För att göra en studie med en så hög evidens som möjligt så valdes en randomiserad, kontrollerad studieteknik.
Avhandlingen baseras på fyra studier:
Delarbete I och II baseras på randomiserade, kontrollerade studier och beskriver stabiliteten efter ett respektive två år efter retentionsbehandling med en av tre retentionsmetoder: vakuumpressad plåt i överkäken kombinerad med kuspidretainer i underkäken, vakuumpressad plåt i överkäken kombinerad med stripsning av underkäksfronten och prefabricerad positioner.
Delarbete III visar en kostnadseffektivitetsanalys efter två års retentionsbehandling.
Delarbete IV baseras på en randomiserad kontrollerad studie efter fem år efter utsatt retentionsbehandling.
Konklusioner av delarbete I och II:
• Ur ett kliniskt perspektiv och på kort sikt efter ett års retention retinerade de tre metoderna behandlingsresultatet väl.
• Efter två års retention var de tre retentionsmetoderna lika effektiva i att kontrollera och motverka recidivet till en kliniskt acceptabel nivå.
• Större delen av recidivet inträffade under det första året medan endast smärre förändringar inträffade under det andra året. • Patienterna indelades i två grupper med utgångspunkt från hur kooperationen bedömdes vara, utomordentlig eller bra. Efter två års retention uppvisade gruppen med utomordentlig kooperation en negativ korrelation mellan längdtillväxt och recidiv i uk-fronten. Gruppen med god kooperation däremot uppvisade en positiv korrelation (Delarbete II, Figur 3). • Efter två års retention hade inte längdtillväxt, initial
trångställning eller kön någon signifikant påverkan på LII i mandibeln (Delarbete II, Figur 4 och tabell 4).
Konklusion av delarbete III:
• Kostnadseffektivitetsanalysen visade, att trots att de tre metoderna uppvisade likartade kliniska resultat så skiljde de sig i kostnader.
• Efter två års retention var behandling med den
vakuumpressade plåten (VFR) i ök och kuspidretainer i uk den minst kostnadseffektiva apparaturen.
Konklusion av delarbete IV:
• Efter fem år efter utsatt retention uppvisade de tre retentionsmetoderna likvärdiga kliniska resultat.
Klinisk betydelse
Denna studie jämförde resultaten på kort och lång sikt av tre ortodontiska retentionmetoder: vakuumpressad plåt i överkäken kombinerad med kuspidretainer i underkäken, vakuumpressad plåt i överkäken kombinerad med stripsning av underkäksfronten och prefabricerad positioner. Alla tre metoderna gav likvärdiga kliniska resultat på kort sikt över ett och två år samt långsiktigt över fem år eller mer.
Efter två års retention påverkade graden av kooperation behandlings resultatet. Däremot visade det sig att varken längdtillväxt, initial trångställning eller kön påverkade behandlingsresultatet.
Idag ökar kraven på den enskilde klinikern att väga in ekonomiska aspekter i vårdplaneringen. Av de tre utvärderade metoderna var, efter två år, den vakuumpressade plåten i överkäken i kombination med kuspidretainer i underkäken den minst kostnadseffektiva retentions metoden.
Den kliniska betydelsen av dessa resultat är att på patienter som motsvarar inklusionskriterierna är stripsningsbehandling och prefabricerad positioner mycket goda behandlingsalternativ till bondad kuspidretainer.
Sammanfattningsvis kan sägas att de tre retentionsmetoderna är likvärdiga och att klinikern därför inte är begränsad till det rutinmässiga användandet av kuspidretainern. Lämplig retentionsmetod bör alltid väljas individuellt, från fall till fall, med utgångspunkt från ortodontisk diagnos, förväntad patientkooperation, patientens önskemål samt ekonomiska hänsynstaganden.
ABBREVIATIONS AND DEFINITIONS
CBA Cost-Benefit Analysis CEA Cost-Effectiveness Analysis
CI Confidence Interval
CMA Cost-Minimization Analysis CTC Canine-To-Canine retainer CUA Cost-Utility Analysis GET Gudrun Edman Tynelius
ITT Intention-To-Treat
LII Little’s Irregularity Index
NHS National Health Service
P Prefabricated positioner covering upper and lower teeth
PP Per Protocol
RCT Randomized Controlled Trial
S Interproximal enamel reduction/stripping of mandibular
incisors and canines
SBU The Swedish Council on Health Technology Assessment
T0 Pretreatment
T1 End of active treatment and start of retention treatment
T2 End of two years of retention treatment
T3 End of five or more years’ postretention
VFR Vacuum-formed retainer covering the maxillary anterior teeth and the palate
INTRODUCTION
Background
A major challenge in orthodontic treatment is to minimize relapse and ensure long-term stability of outcome (1-4). Relapse most commonly occurs in the mandibular anterior segment. This is also usually the site of initial relapse (5).
Most of the relapse after orthodontic treatment occurs quite soon after debonding: half is seen within days, due to stretching of the gingival tissues (6-8). The periodontal membrane fibres have a turnover rate of weeks, while remodelling of supragingival fibres takes months (6, 9, 10). Thus, a retention method must have the capacity to stabilise the orthodontic result during all of these tissue-remodelling phases.
In the latter part of the 20th century, treatment philosophies were considered decisive for orthodontic outcome: it was assumed that using a specific orthodontic technique, for example, Edgewise, Begg or Straight Wire Appliance, would give better long-term stability than others. This was too simplistic a response to a much more complicated problem. The current broad consensus on how to retain to long-term stability is based largely on retrospective studies. Study designs have progressed through retrospective and prospective studies to the current gold standard, the randomized controlled study, which offers a higher degree of evidence. There are several short-term studies of orthodontic retention (11-14), but few studies of long-term stability.
A review by the Cochrane group in 2006 concluded that to date there was insufficient evidence to single out any particular retention strategy as the preferred method (15); it was concluded that future studies should include true randomization, reporting of dropouts,
adequate sample size calculation and a minimum follow-up period of three months.
Prevalence
Between 43 and 78 % of all children and adolescents have some kind of malocclusion. The widely varying reported prevalence is attributable to variations in the age groups examined and the diagnostic methods applied (16). In Sweden, approximately one-third of all children and adolescents are offered orthodontic care free of charge (17). General practitioners are responsible for the preliminary orthodontic diagnosis and selection of subjects. Decisions on orthodontic treatment are made in consultation with orthodontists (18).
Evidence-based healthcare
Evidence-based healthcare may be defined as the precise and systematic implementation of evidence in clinical decision-making, thereby offering the greatest patient benefit while utilizing resources in the most effective way. However, factors of importance in determining treatment outcome include not only the scientific evidence, but also the patients’ preferences and the clinicians’ experiences. One of the primary goals of evidence-based healthcare is to support the rapid adoption of effective methods and to discourage the dissemination of ineffective methods. From a scientific perspective, the evidence-based approach is a valuable instrument for identifying knowledge gaps and clarifying the need for clinical trials.
The randomized controlled trial or the RCT is the gold standard for clinical trials and is used to test the effectiveness of one or several interventions: included in the trial is a control group, comprising subjects who receive no treatment. Eligible subjects are randomly assigned to a treatment or control group before implementation of the intervention to be studied. The advantage of proper randomization is that it minimizes allocation bias, balancing both known and unknown factors.
In some clinical trials an untreated group of control subjects would be unethical, and is therefore not included in the study design. Under certain circumstances, a control group may consist of a group of subjects treated with a previously tested treatment.
However, there are some misconceptions about evidence-based healthcare, such as the concept that all evidence which has not been scientifically evaluated should be dismissed. Lack of evidence is not necessarily synonymous with lack of effect. It is important to acknowledge that well-designed prospective and retrospective studies may also provide valuable evidence.
Methodology
Analyzing subjects according to the Intention To Treat (ITT) principle means that all subjects are included in the results whether they participated or not. Nonparticipants are considered to be failures or are allocated estimated measurements. Another avaliable principle is the Per Protocol (PP) principle, whereby results are presented for those who attended and the unavailable subjects are described as missing.
Little’s irregularity index (19), intercanine and intermolar widths, arch lengths, overbite and overjet are all standard measurements made on dental casts.
Economic evaluation in healthcare
The sciences of evidence-based healthcare and economic evaluation in healthcare developed in the latter part of the 20th century, in acknowledgement of the principle that high quality healthcare should be equally available to all citizens, according to need (20-25). New and existing healthcare systems and procedures should be evaluated by evidence-based research to ensure good ’value for money’ (26).
Economic evaluation in healthcare is defined as ’the comparative analysis of alternative courses of action in terms of their costs and consequences’ (27). There are four types of economic evaluations: • A ’cost-effectiveness analysis’ (CEA) is based on both costs and
outcomes, where outcomes of alternative methods might differ in magnitude.
• A ’cost-minimization analysis’ (CMA) may be undertaken when the outcomes are equal (e.g. three retention methods achieve the treatment goal irrespective of which treatment is applied) and the aim is to determine which treatment has the lowest cost.
• A ’cost-utility analysis’ (CUA) deals with the health outcome following treatment and can be used in health-related quality of life studies.
• A ’cost-benefit analysis’ (CBA) is used to evaluate distribution of resources to different areas of healthcare.
To determine the economical effects, calculations are usually separated into direct, indirect and societal costs.
• Direct costs comprise material costs and treatment time costs. Treatment time costs are the costs of staff, premises, dental equipment, maintenance and cleaning.
• Indirect costs are defined as loss of time at school and in travelling to and fro the orthodontic clinic. In this study the majority of patients were adolescents and came to the clinic for their retention controls on their own, unaccompanied by parents.
• Societal costs are defined as the sum of direct and indirect costs.
Retention methods
In Sweden, the commonly used retention appliances are bonded maxillary and mandibular retainers, bonded either to all the anterior teeth or to the canines only. The bonded retainers are often combined with different removable appliances for full-time or night-only wear, e.g. Hawley retainer, Jensen retainer, Essix retainer and vacuum-formed retainers. The length of time patients are required to continue using their retainers varies from clinician to clinician, from never to forever, with a mean time of a couple of years.
Several removable retention appliances have been studied in the short-term (11-14, 28). The results indicate that Essix retainers and vacuum-formed retainers are superior in retaining treatment results and that night-only wear is as effective as full-time wear.
The positioner is an eruption guidance appliance used in the early mixed dentition (29). There is to date no published research showing the effectiveness of prefabricated positioners in retaining orthodontic treatment results.
A retrospective 3-year follow-up study has shown that interproximal stripping of the mandibular anterior teeth in combination with overcorrection of rotated teeth is sufficient to prevent relapse (8).
Canine-to-canine retainers may be bonded to canines only, or in combination with one or several incisors. There are many incidents of broken retainers of either type, causing inconvenience for patients and clinicians alike (30, 31). Among important aspects of retention treatment which have not been fully investigated are the long-term dental and periodontal health implications of bonded retainer therapy (32).
SIGNIFICANCE
The background of this thesis is the lack of evidence to support current orthodontic retention treatments. In 2006 a meta-analysis by The Cochrane Collaboration Group concluded that there was lack of evidence as to how best to retain stability after orthodontic treatment (15).
It is important that the clinician provides highly qualified orthodontic treatment including retention, and informs patients about the expected long-term effects of treatment. Patients demand a stable treatment result and society expects good value for money. When two or more treatments have shown similar clinical outcomes, a cost-minimization analysis is the appropriate method of analysing cost-effectiveness.
Although the need for this kind of research has long been apparent, such studies are very demanding in terms of planning, patient recruitment and follow-up. The four studies on which this thesis is based were designed to evaluate short- and long-term stability after orthodontic treatment, from an evidencebased perspective. Strict inclusion criteria were applied. Treatment planning included extractions of four premolars, a fixed straightwire appliance and retention treatment with one of three retention methods.
AIMS
The specific aims of Papers I-IV were:
Paper I
using RCT methodology, to evaluate and compare the capacity of three different retention methods to retain orthodontic treatment results on a short-term basis, i.e. after one year of retention.
Paper II
to analyse and compare the three retention methods evaluated in Paper I after two years of retention, in a randomized clinical trial and to evaluate the retention capacity in relation to compliance, growth, initial crowding and gender.
Paper III
to evaluate and compare the costs of the three retention methods studied in Papers I and II. Paper II showed that the clinical results for the three methods were similar, hence the material was appropriate for a cost-minimization analysis.
Paper IV
to evaluate the effects of the three different retention strategies in Papers I and II in maintaining stability at least five years post-retention.
HYPOTHESES
Paper I
After one year of retention, there is no difference in retention capacity among any of the three retention methods.
Paper II
After two years of retention, there is no clinical difference in retention capacity among the three retention methods, in compliant patients.
Paper III
The three retention methods are equally cost-effective.
Paper IV
MATERIALS AND METHODS
Subjects
Papers I, II, III and IV
The study subjects comprised patients referred to a Swedish National Health Service (NHS) specialist orthodontic clinic in Ystad, Sweden. This clinic accepted referrals and treated malocclusions in patients in the southeast County Council of Scania. The same experienced orthodontist (GET) treated all the study participants between 2001 and 2007.
The following inclusion criteria were met:
• No previous experience of orthodontic treatment • Permanent dentition
• Normal skeletal sagittal, vertical and transverse relationships • Class I molar relationship or a maximum of 3 mm anterior or
posterior deviation
• Space deficiencies in both jaws
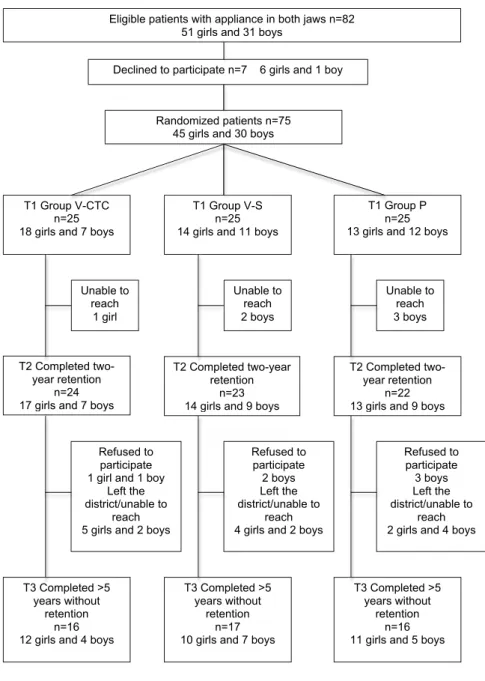
• A treatment plan involving extraction of four premolars followed by fixed straightwire appliances in both jaws (33, 34) Out of 82 patients invited to participate, 7 declined. The remaining 75 patients were randomized into three groups of 25 subjects each (Figure 1). A different retention strategy was applied to each group: Group V-CTC, ”maxillary vacuum-formed retainer and bonded mandibular canine-to-canine retainer”; Group V-S ”maxillary vacuum-formed retainer and mandibular interproximal enamel reduction (stripping)” and Group P: ”prefabricated positioner”.
T3 Completed >5 years without
retention n=17 10 girls and 7 boys T3 Completed >5
years without retention
n=16 12 girls and 4 boys
T3 Completed >5 years without
retention n=16 11 girls and 5 boys T2 Completed
two-year retention n=24 17 girls and 7 boys
T2 Completed two-year retention
n=23 14 girls and 9 boys
T2 Completed two-year retention
n=22 13 girls and 9 boys T1 Group V-CTC
n=25 18 girls and 7 boys
T1 Group V-S n=25 14 girls and 11 boys
T1 Group P n=25 13 girls and 12 boys Randomized patients n=75
45 girls and 30 boys
Declined to participate n=7 6 girls and 1 boy Eligible patients with appliance in both jaws n=82
51 girls and 31 boys
Unable to reach 1 girl Unable to reach 2 boys Unable to reach 3 boys Refused to participate 1 girl and 1 boy
Left the district/unable to
reach 5 girls and 2 boys
Refused to participate 2 boys Left the district/unable to reach 4 girls and 2 boys
Refused to participate 3 boys Left the district/unable to reach 2 girls and 4 boys Completed
Figure 1. The flow diagram of the trial. Maxillary vacuum-formed retainer (VFR) and bonded mandibular canine-to-canine retainer (Group V-CTC), maxillary VFR and mandibular interproximal enamel reduction (S) of anterior teeth (Group V-S), and prefabricated positioner (Group P).
Paper I
After exclusion of two subjects for non-compliance, the study material at the end of the first year of retention treatment comprised 73 subjects.
Paper II
After 2 years of retention treatment, 69 subjects remained in the trial: four subjects failed to present for the 2-year follow-up and 2 boys in group P were excluded during the first year as they never used their retainers.
Paper III
After 2 years of retention treatment, the societal costs were estimated for 75 subjects, regardless of whether or not they presented for the 2 year follow-up.
Paper IV
Of the original 75 subjects enrolled in the study, 49 were followed for five years or more. Twenty-six failed to complete the trial.
Ethical considerations and consent
The Ethics Committee of Lund/Malmö University, Sweden, approved the protocol and the informed consent form (LU515-01). Each patient and parent received verbal as well as written information. Signed, written consent was required before inclusion in the trial. As the patients were not of age at the start of retention (most were aged between 14 and 15 years) their parents had to give written consent but no patient was included in the study against their will. The Swedish Ethical Review Act states that in the case of under-aged subjects, verbal consent must be requested (35).
Randomization
Sequence randomization was generated in blocks of 15 to ensure that equal numbers of subjects were allocated to each of the three retention groups. A ballot system was used for allocation, in lots of fifteen: five ballots were labelled “maxillary vacuum-formed retainer and bonded mandibular canine-to-canine retainer”, five were labelled “maxillary vacuum-formed retainer and mandibular interproximal
enamel reduction (stripping)”, and five were labelled “positioner”. The fifteen ballots were placed in a basket by an independent observer. The patient was then allocated to one of the three groups by picking a ballot from the basket shortly before debonding. When the first basket was empty, a second lot of ballots was prepared, and as patients were recruited to the study, these 15 ballots were extracted successively. In all, this procedure was repeated five times, for randomization of the 75 patients.
Methods
Papers I, II and IV
Retention methodsThe three retention methods investigated were:
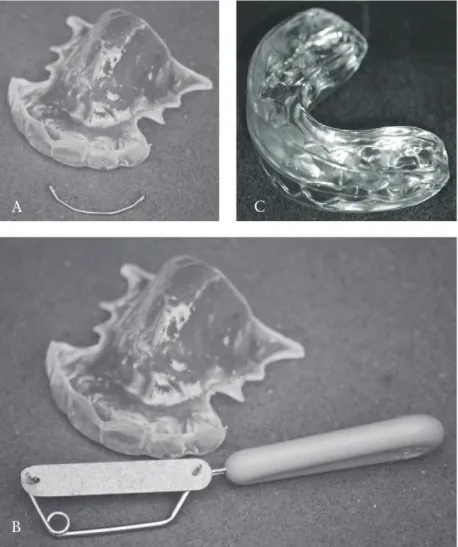
• A removable vacuum-formed retainer covering the palate and the maxillary anterior teeth from canine-to-canine and a bonded mandibular canine-to-canine retainer (Group V-CTC) (Figure 2)
• A maxillary vacuum-formed retainer identical to that in Group V-CTC, combined with interproximal stripping of the mandibular anterior teeth (Group V-S) (Figure 2) (9, 10, 36) • A prefabricated positioner covering all erupted maxillary and
mandibular teeth (Group P) (Figure 2) (29)
The vacuum-formed retainers were made of 2 mm Biolon (Dreve Dentamid GmbH, Unna, Germany) in a Scheu Ministar press (Scheu-Dental GmbH, Iserlohn, Germany). The canine retainers consisted of 0.7 mm spring hard wire (Dentaurum noninium, Dentaurum, Ispringen, Germany) bonded to the mandibular canines with Transbond LC (3M Unitek Orthodontic Products, Monrovia, USA). Mechanical stripping of the mandibular incisors and canines was carried out either by hand, with single sided medium and fine metal blades (TP Orthodontics, La Porte, Indiana, USA) or by the EVA Ortho-Strips System (GAC International, New York, USA). In order to avoid trauma to the interdental papilla, the appropriate method of stripping was selected according to tooth form, non-triangular or triangular respectively. There is a greater risk of papillary damage if the EVA system is used on the non-triangular form; in these cases manual use of single-sided blades was the preferred option. The
to debonding, or at debonding. The aim was to achieve small but distinct enamel flattening of the contact surfaces. The reduction of any contact point between two teeth was approximately the thickness of the coarse blade of either system, i.e. 0.22 mm for hand stripping or 0.34 mm for EVA-stripping. The preformed positioner (Ortho-Tain Positioner, Ortho-(Ortho-Tain Inc., Toa Alta, Puerto Rico) comprised a soft plastic appliance, covering all erupted teeth.
Figure 2. Maxillary vacuum-formed retainer (VFR) and bonded mandibular canine-to-canine retainer (Group V-CTC), maxillary VFR and mandibular interproximal enamel reduction (S) of anterior teeth (Group V-S), and prefabricated positioner (Group P).
A
B
All retention appliances were distributed within one hour after debonding. The subjects in groups V-CTC and V-S were instructed to wear the vacuum-formed retainer 22-24 hours per day for two days and nights and then at night for 12 months. In group P the positioner was to be worn for 30 minutes during the day and at night for 12 months. During daytime wear the subjects were instructed to chew actively on their positioners. During the second year of retention the retainers were worn every other night.
Data collection
Nine separate appointments were scheduled for each subject, for impressions for dental casts and photographs: before start of treatment (T0), at the end of active treatment and start of retention (T1), after one year of retention, at the end of two-years’ retention (T2), and post-retention after one, two, three, four and five years (T3). Measurements were taken on the dental casts on the above nine occasions. Paper I presents the measurements at T0, T1 and after one year of retention, Paper II the measurements at T0, T1 and T2 and, finally, Paper IV presents the measurements at T0, T1, T2 and T3.
One examiner (GET) took the following linear measurements on dental casts using an electronic digital caliper (Mauser Digital 6, Winterthur, Switzerland) to a precision of 0.01 mm:
• Little´s irregularity index (LII) for the maxilla and the
mandible - the summed displacement of the anatomic contact points of the upper and lower incisors and canines (19) • Maxillary and mandibiular intercanine widths: the distance
between the canine cusp tips
• Maxillary and mandibiular intermolar widths: the distance between the mesiobuccal cusp tips of the first molars • Maxillary and mandibiular arch lengths: the perpendicular
distance from the midpoint of the incisal edges of the central incisors to a line joining the mesial anatomic contact points of the first molars
• Overbite - the overlap of upper to lower central incisors • Overjet - the distance parallel to the occlusal plane from
the incisal edge of the most labial maxillary incisor to the opposing mandibular central incisor
Data on patient ages and treatment times were retrieved from the treatment records.
Data analysis: Per protocol (PP)
The PP-strategy was selected as the chosen strategy for analyzing measurements.
Paper III
The outcome to be assessed was the costs of two years of retention treatment, including both scheduled and unscheduled appointments. Papers I and II confirmed that in compliant patients the three retention methods were equally effective in retaining the results of the orthodontic treatment (37, 38). Thus cost minimization analysis (CMA) could be applied. Five appointments were scheduled for each subject during the two-year retention treatment period. As the trial was randomized, a similar number of broken appointments and cancellations could be expected in the three groups.
Data analysis: Intention-to-treat (ITT)
The CMA was based on the Intention-To-Treat principle (ITT), i.e. the analysis included all data on 75 patients. If subjects presented for their appointments, there were direct and indirect costs. If subjects failed to present there were still direct costs but the indirect costs were nil.
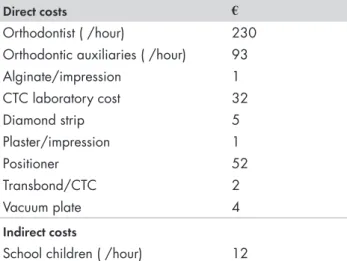
Direct costs
Direct costs comprised material costs and treatment time costs. Material costs, i.e. impression material, orthodontic bonding material, laboratory material and fees, consumables, etc., were compiled and calculated according to average commercial prices (Table 1).
Treatment time costs included the costs of premises, dental equipment, maintenance and cleaning and were calculated according to average commercial prices in Sweden. Staff salaries, including
payroll tax, were calculated for dental auxiliaries (€93/hour) and
the orthodontist (€230/hour) (Table 1). The treatment costs were
calculated and estimated in Euros (€). Treatment times in minutes for
measured with a stop-watch for each patient, on the assumption that the randomization process produced equal groups. The estimation of treatment time was based on the booked chairside time.
Indirect costs
Indirect costs were defined as loss of time from school and in travelling
to and from the orthodontic clinic, i.e. €12/hour for school children
(Table 1). As most of the subjects were adolescents and attended their retention control appointments on their own, i.e. unaccompanied by a parent, parental time was not included. The clinic was close to the school: travelling time to the clinic was estimated at 15 minutes. All
costs were based on 2013 prices and were expressed in Euros (€),
SEK 100= €11.63 on 25 April 2013 (www.xe.com).
Direct costs €
Orthodontist ( /hour) 230 Orthodontic auxiliaries ( /hour) 93
Alginate/impression 1 CTC laboratory cost 32 Diamond strip 5 Plaster/impression 1 Positioner 52 Transbond/CTC 2 Vacuum plate 4 Indirect costs
School children ( /hour) 12
Table 1. Direct and indirect costs in Euros ( ). CTC, mandibular canine-to-canine retainer.
Societal costs
Societal costs were defined as the sum of direct and indirect costs. Cost-minimization analysis
As all three treatment outcomes were equal, a cost-minimization analysis (CMA) was undertaken. Higher values (i.e. higher costs) indicate relatively less cost-minimization than lower values (i.e. lower
CMA = Societal costs Number of subjects
This calculation divides the societal costs by the total number of subjects after two years of retention. A second cost-minimization analysis was made on the group of subjects who presented for unscheduled appointments.
Statistical analysis
Sample size calculationIn Papers I, II and IV the calculated sample size for each group was based on a significance level of 0.05 and 80 per cent power to detect a clinically meaningful difference of 2.0 mm (SD = 2.0 mm) of the LII. Power analysis showed that at least 16 subjects would be required in each group. To compensate for attrition in the follow-up study, 25 subjects were enrolled in each group.
Descriptive statistics
In Papers I, II and IV arithmetic means and standard deviations (SD) were calculated at group level for each variable, at times corresponding to pretreatment (T0), the end of active treatment and start of retention (T1), after two years of retention treatment (T2), and after five years or more out of retention (T3).
Differences between and within groups
Significant differences in means between groups were assessed by one-way analysis of variance (ANOVA) and within groups, by t-test to the previous time point, using the Statistical Package for Social Sciences (version 22.0.0.0, IBM SPSS Inc., Chicago, Illinois, USA). P-values less than 5 per cent (P<0.05) were considered statistically significant.
Error of method
Twenty randomly selected dental casts were measured by the same examiner (GET) on two separate occasions at an interval of four weeks. The error of the method did not exceed 0.45 mm for any of the 10 measurements (39). A paired t-test disclosed no significant mean differences between the two series of records.
RESULTS
Paper I – one year of retention
The mean age at the start of retention (T1) was 14.1 years (SD 1.3) in group V-CTC (18 girls, 7 boys), 14.7 years (SD 1.8) in group V-S (14 girls, 11 boys) and 14.3 years (SD 1.5) in group P (13 girls, 12 boys) (Figure 1). The mean active orthodontic treatment period was 1.6 years (SD 0.3) in the V-CTC group, 1.8 years (SD 0.5) in the V-S group and 1.6 years (SD 0.3) in the P group. There were no significant intergroup differences with respect to age or duration of active treatment. Moreover, there were no significant differences among any of the three retention strategies with respect to linear measurements on the study casts before and after active treatment. Maxilla
Small, insignificant intergroup differences were found among the maxillary retention methods. During the retention period the mean LII increased between 0.5 and 0.8 mm. In all three groups, the mean intercanine widths decreased: the change was more pronounced for
the positioner (1.6 mm) than for the vacuum-formed retainer
(0.6-0.7 mm). The mean intermolar width decreased between 0.8 and 1.0 mm. All three groups exhibited a minimal increase in mean arch length (0.1-0.3 mm) (Paper I, Table 1).
Mandible
In the mandible, small, insignificant intergroup differences were observed in mean LII: the mean increase in LII was greatest in the P group (1.1 mm) followed by the V-S and V-CTC groups (0.8 and 0.6
There was a significant difference in mean intercanine width between groups V-CTC and V-S (P <.001): it was unchanged in the V-CTC group, whereas group V-S exhibited a mean reduction of -1.0 mm. In group P the mean reduction was -0.7 mm (Paper I, Table 1).
Insignificant intergroup differences in mean intermolar width were also observed: in group V-CTC it was unchanged but decreased in the V-S and P groups by 0.6 and 0.8 mm respectively (Paper I, Table 1).
There was a significant difference in mean arch length between the V-CTC and V-S groups (P <0.05): it remained unchanged in the V-S group, but increased in the V-CTC group to 0.7 mm. In the P group the mean change was 0.5 mm (Paper I, Table 1).
Overbite and overjet
There was a small but significant change in overbite between groups V-CTC and V-S: -0.4 and +0.2 mm respectively (P <0.05). In group P the mean change was -0.2 mm. The mean overjet was stable in all three groups with a range of 0.0 to 0.3 mm (Paper I, Table 1).
Paper II – two years of retention
After 2 years of retention (T2), 69 of the original 75 subjects remained in the trial: 24 (17 girls and 7 boys) in group V-CTC, 23 (14 girls and 9 boys) in group V-S and 22 (13 girls and 9 boys) in group P (Figure 1). There were no significant intergroup differences with respect to age at start of treatment, active treatment time, body height at retention start, or gender.
Maxilla
The only significant intergroup difference was in the mean change in maxillary intercanine width: P (-1.8 mm) vs. V-CTC (-1 mm) and V-S (-0.9 mm) (p < 0.01) (Table 1). Most of this difference occurred during the first year, although at that stage the differences were not significant (Paper II, Table 1).
Mandible
There was a significant difference in mean mandibular LII change between V-CTC (0.6 mm) and P (1.6 mm) (p < 0.01). The change was greatest, but not significant, during the first year of retention but persisted in the P group (Paper II, Table 2).
There were significant intergroup differences in mean intercanine width: an increase of 0.2 mm in V-CTC, and decreases in V-S (-1.0 mm) and P (-1.1 mm) (p < 0.001). The difference between V-CTC and V-S had already been observed during the first year (p < 0.001).
During the second year, significant intergroup differences emerged in mean intercanine widths between P (-0.4 mm) and V-CTC (0.1 mm) and V-S (0.0 mm) (p < 0.01). After two years, the mean intercanine width differed significantly between V-CTC (27.6 mm) and V-S (26.4 mm) (p < 0.05) (Paper II, Table 2).
Intermolar width and arch length did not differ significantly at the end of the 2 year follow-up period (Paper II, Table 2).
Overbite and overjet
The mean overbite decreased, albeit not significantly, in V-CTC (-0.4 mm) and increased in V-S (0.4 mm) and P (0.2 mm). Nevertheless, during the first year there was a significant difference in mean change in overbite between V-CTC (-0.4 mm) and V-S (0.2 mm) (p < 0.05) (Paper II, Table 3).
There was a significant difference in mean overjet between V-CTC (2.8 mm) and V-S (3.6 mm) (p < 0.05), due to a reduction in V-CTC (-0.3 mm) and an increase in V-S (0.5 mm) (p < 0.05) (Paper II, Table 3).
Retention capacity and compliance
Of the 69 subjects who completed the trial, compliance was assessed as excellent in 38 and good in 31 (Paper II, Fig. 3). This figure shows that in the group with excellent compliance, there was a negative correlation between change in mandibular LII and growth, but a positive correlation in the group with good compliance. Thus when patient compliance was excellent, LII did not change, even though the subjects were growing. The t-test for independent samples disclosed a significant difference in mean change of mandibular LII, with 0.7 mm in the group with excellent compliance and 1.3 mm in the good compliance group (p < 0.05). There was no significant difference in compliance between boys and girls.
During the two years of retention, five subjects mislaid their vacuum-formed retainers and had to have replacements made. No patients lost a positioner. Of 24 subjects, 17 kept their CTC in situ.
Three subjects had their CTC rebonded once, three twice and one subject four times. These complications did not have any significant influence on the outcome of retention.
Retention capacity and body height growth
Height was measured at the start of retention and after two years of retention. However, for 13 subjects, the measurements were incomplete, leaving 56 subjects for whom both measurements were available (Paper II, Fig. 4). In group V-CTC (14 girls and 5 boys), the mean body height increase was 1.4 cm (SD 1.8), in V-S (9 girls and 7 boys) 2.4 cm (SD 3.1) and in P (13 girls and 8 boys) 1.4 cm (SD 2.5). There were no significant intergroup differences during the two years. The boys grew significantly more than the girls: mean 3.3 cm (SD 3.2) for boys and 0.8 cm (SD 1.2) for girls. None of the other measurements differed significantly between boys and girls. During the two years of retention, 29 subjects (14 girls and 15 boys) grew more than 1 cm and 4 of these (1 girl and 3 boys) had an increase of mandibular LII greater than 3.5 mm, with a maximum of 4.9 mm. No correlation was found between mean change of LII and growth in body height (Paper II, Figure 4).
Retention capacity and initial crowding
After two years of retention, there was no significant difference in mandibular LII between the group of 18 subjects with initial mild crowding (LII < 3.5 mm) and the group of 28 subjects with severe crowding (LII > 6.5 mm) (Paper II, Table 4).
Retention capacity and gender
After two years, 44 girls and 25 boys remained in the study. There was no significant difference between boys and girls with respect to any of the measurements.
2
Paper III – Cost-minimization analysis
The outcome to be assessed was the cost of two years of retention treatment for a group of 75 patients, including both scheduled and unscheduled appointments. Papers I and II showed that the three retention methods were equally effective in retaining the result of the orthodontic treatment in compliant patients. Thus, CMA could
be applied. During the two-year retention treatment period, five appointments were scheduled for each subject. Direct and indirect costs were estimated (Table 1). As the trial was randomized, broken appointments and cancellations could be expected to be similar in all three groups.
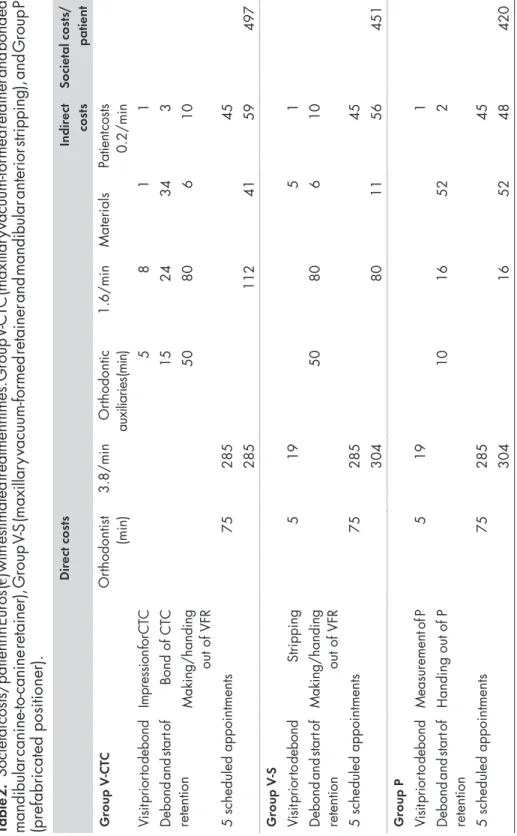
Societal costs for scheduled appointments
The societal costs/patient for two years of retention treatment were €497 in group V-CTC, €451 in group V-S and €420 in group P
(Table 2). The total costs per group for the 25 patients were €12425
for group V-CTC, €11275 for group V-S and €10500 for group P.
In Group V-CTC the direct costs comprised €438 and the indirect
costs €59.
In Group V-S the direct costs were €395 and the indirect costs €56.
Finally, in Group P the direct costs were €372 and the indirect
costs €48.
Societal costs for unscheduled appointments
Societal costs for a bonded/rebonded CTC were €35, a new CTC
€75, a new vacuum-formed retainer €101 and a new positioner €67 (Paper III, Table 4).
In Group V-CTC, 13 subjects had their CTC bonded/rebonded, two subjects needed replacement CTC’s and two needed new vacuum-formed retainers. The total cost for unscheduled appointments in this
group was €807 or €32 per patient.
In Group V-S, three subjects had their vacuum-formed retainers replaced. The total cost for unscheduled appointments in this group
was €303 or €12 per patient.
Finally, in Group P no unscheduled appointments occurred.
Paper IV – Long-term effects and stability
Of the 75 subjects originally enrolled, 26 failed to complete the trial: three declined to participate and 23 left the district or were unable to be contacted. Consequently, 49 subjects (33 girls, 16 boys) attended their final appointment after five years or more out of retention (T3) (Figure 1; Table 3). As there were no significant differences between boys and girls in any of the study variables, the data for the sexes were pooled for analysis.
Table
2.
Societal costs/patient in Euros (
€) with estimated treatment times. Group V
-CTC (maxillar
y vacuum-for
med retainer and bonded
mandibular canine-to-canine retainer), Group V
-S (maxillar
y vacuum-for
med retainer and mandibular anterior stripping), and Group P
(prefabricated positioner). Dir ect cos ts Indir ect cos ts Societal cos ts/ patient Gr oup V -CT C Or thodontist (min) 3.8/min Or thodontic au xi liar ie s (m in ) 1.6/min Materials Patient costs 0.2/min
Visit prior to debond
Impression for CTC
5
8
1
1
Debond and star
t of retention Bond of CTC 15 24 34 3 Making/handing out of VFR 50 80 6 10 5 scheduled appointments 75 285 45 285 112 41 59 497 Gr oup V -S
Visit prior to debond
Stripping
5
19
5
1
Debond and star
t of retention Making/handing out of VFR 50 80 6 10 5 scheduled appointments 75 285 45 304 80 11 56 451 Gr oup P
Visit prior to debond
Measurement of P
5
19
1
Debond and star
t of retention Handing out of P 10 16 52 2 5 scheduled appointments 75 285 45 304 16 52 48 420
Table 3. Post-retention, showing how many years the 49 patients had been out of retention at T3: minimum of five years.
5 years 6 years 7 years 8 years 9 years
V-CTC 13 1 1 1
V-S 12 4 1
P 15 1
Totals 40 6 1 1 1
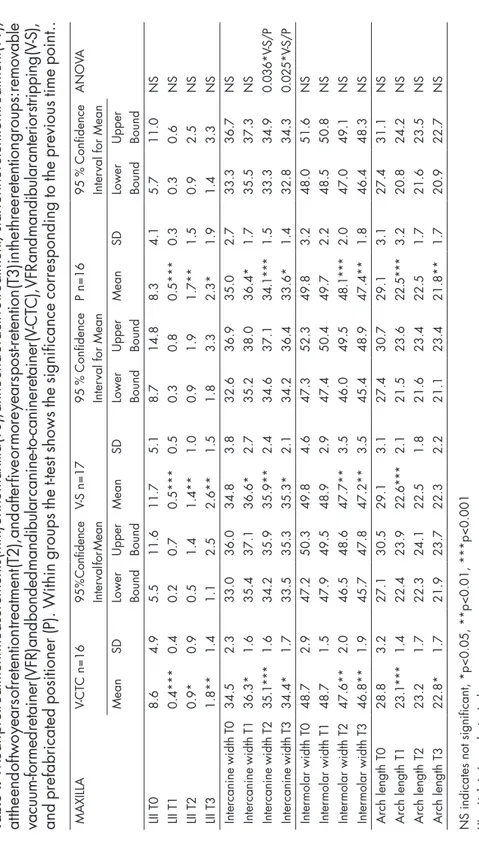
Maxilla T0-T3 (Table 4)
At the start of treatment (T0), the mean LII was 8.6 mm in the V-CTC group, 11.7 mm in the V-S group and 8.3 mm in the P group. There were no significant intergroup differences. After treatment (T1), the mean LII was less than 0.5 mm in all three groups, with no significant intergroup differences. Small changes in LII occurred during the retention period (T1-T2).
After five years or more out of retention (T3), the mean LII ranged from 1.8 to 2.6 mm. There were no significant intergroup differences.
In all three groups, there was an average increase in intercanine width of 1-2 mm during treatment (T0-T1), with a return to pretreatment levels in all groups at T3. Small, albeit significant intergroup differences were found between the V-S and P groups after two years of retention (T2) and this difference remained at T3.
The intermolar width and arch length decreased during treatment (T0-T1) in all groups because of extraction of premolars, but then remained fairly stable during the retention period as well as during the five-year postretention period. No significant intergroup differences were found.
MAXILLA V-CTC n=16 95 % C on fid en ce Inter
val for Mean
V-S n=17
95
%
Confidence
Inter
val for Mean
P n=16
95
%
Confidence
Inter
val for Mean
ANOV A Mean SD Lower Bound Upper Bound Mean SD Lower Bound Upper Bound Mean SD Lower Bound Upper Bound LII T0 8.6 4.9 5.5 11.6 11.7 5.1 8.7 14.8 8.3 4.1 5.7 11.0 NS LII T1 0.4*** 0.4 0.2 0.7 0.5*** 0.5 0.3 0.8 0.5*** 0.3 0.3 0.6 NS LII T2 0.9* 0.9 0.5 1.4 1.4** 1.0 0.9 1.9 1.7** 1.5 0.9 2.5 NS LII T3 1.8** 1.4 1.1 2.5 2.6** 1.5 1.8 3.3 2.3* 1.9 1.4 3.3 NS Intercanine width T0 34.5 2.3 33.0 36.0 34.8 3.8 32.6 36.9 35.0 2.7 33.3 36.7 NS Intercanine width T1 36.3* 1.6 35.4 37.1 36.6* 2.7 35.2 38.0 36.4* 1.7 35.5 37.3 NS Intercanine width T2 35.1*** 1.6 34.2 35.9 35.9** 2.4 34.6 37.1 34.1*** 1.5 33.3 34.9 0.036* V -S/P Intercanine width T3 34.4* 1.7 33.5 35.3 35.3* 2.1 34.2 36.4 33.6* 1.4 32.8 34.3 0.025* V -S/P Inter molar width T0 48.7 2.9 47.2 50.3 49.8 4.6 47.3 52.3 49.8 3.2 48.0 51.6 NS Inter molar width T1 48.7 1.5 47.9 49.5 48.9 2.9 47.4 50.4 49.7 2.2 48.5 50.8 NS Inter molar width T2 47.6** 2.0 46.5 48.6 47.7** 3.5 46.0 49.5 48.1*** 2.0 47.0 49.1 NS Inter molar width T3 46.8** 1.9 45.7 47.8 47.2** 3.5 45.4 48.9 47.4** 1.8 46.4 48.3 NS Arch length T0 28.8 3.2 27.1 30.5 29.1 3.1 27.4 30.7 29.1 3.1 27.4 31.1 NS Arch length T1 23.1*** 1.4 22.4 23.9 22.6*** 2.1 21.5 23.6 22.5*** 3.2 20.8 24.2 NS Arch length T2 23.2 1.7 22.3 24.1 22.5 1.8 21.6 23.4 22.5 1.7 21.6 23.5 NS Arch length T3 22.8* 1.7 21.9 23.7 22.3 2.2 21.1 23.4 21.8** 1.7 20.9 22.7 NS
NS indicates not significant, *p<0.05, **p<0.01, ***p<0.001 LII = Little´s Irregularity Index
Table
4.
Mean pretreatment measurements (mm) of the maxilla (T0), at the end of active treatment/star
t of the retention treatment (T1),
at the end of two years of retention treatment (T2), and after five or more years post-retention (T3) in the three retention groups: removable vacuum-for
med retainer (VFR) and bonded mandibular canine-to-canine retainer (V
-CTC), VFR and mandibular anterior stripping (V
-S),
and prefabricated positioner (P). W
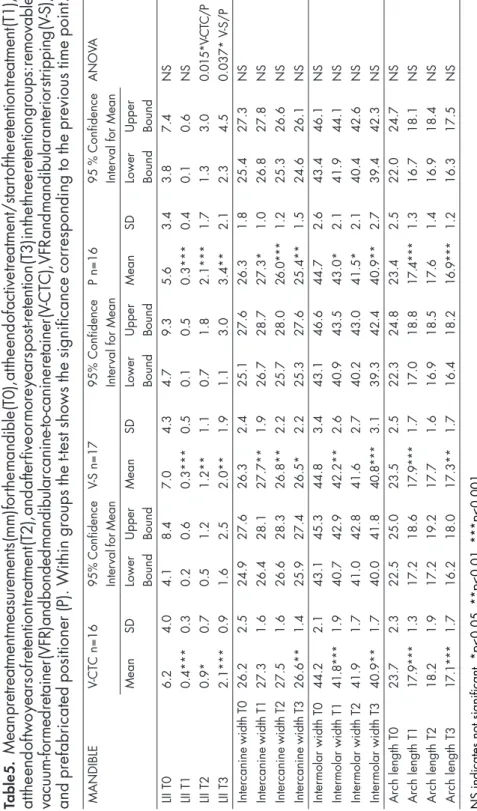
Mandible T0-T3 (Table 5)
At the start of orthodontic treatment (T0), the mean LII was 6.2 mm in the V-CTC group, 7.0 mm in the V-S group and 5.6 mm in the P group, with no significant intergroup differences. After treatment (T1), the mean LII was less than 0.4 mm in all three groups, with no significant intergroup differences.
Small changes in LII occurred during the retention period (T1-T2). In the P-group a small but significantly higher LII was apparent compared to the V-CTC, mean 2.1 versus 0.9 mm. After five years or more out of retention (T3), the mean LII ranged from 2.0 to 3.4 mm. The average value was significantly higher in the P group than in the V-S group.
In all three groups, intercanine width increased on average 1 mm during treatment (T0-T1) and had returned to pretreatment levels at T3. No significant intergroup differences were found.
As in the maxilla, mandibular intermolar width and arch length decreased during treatment (T0-T1) in all groups because of extraction of premolars. Both measurements remained fairly stable during the retention period as well as during the five-year postretention period. No significant intergroup differences were found.
MANDIBLE V-CTC n=16 95% C onfidence In te rv al fo r M ea n V-S n=17 95% Confidence Inter
val for Mean
P n=16
95
%
Confidence
Inter
val for Mean
ANOV A Mean SD Lower Bound Upper Bound Mean SD Lower Bound Upper Bound Mean SD Lower Bound Upper Bound LII T0 6.2 4.0 4.1 8.4 7.0 4.3 4.7 9.3 5.6 3.4 3.8 7.4 NS LII T1 0.4*** 0.3 0.2 0.6 0.3*** 0.5 0.1 0.5 0.3*** 0.4 0.1 0.6 NS LII T2 0.9* 0.7 0.5 1.2 1.2** 1.1 0.7 1.8 2.1*** 1.7 1.3 3.0 0.015* V -CTC/P LII T3 2.1*** 0.9 1.6 2.5 2.0** 1.9 1.1 3.0 3.4** 2.1 2.3 4.5 0.037* V -S/P Intercanine width T0 26.2 2.5 24.9 27.6 26.3 2.4 25.1 27.6 26.3 1.8 25.4 27.3 NS Intercanine width T1 27.3 1.6 26.4 28.1 27.7** 1.9 26.7 28.7 27.3* 1.0 26.8 27.8 NS Intercanine width T2 27.5 1.6 26.6 28.3 26.8** 2.2 25.7 28.0 26.0*** 1.2 25.3 26.6 NS Intercanine width T3 26.6** 1.4 25.9 27.4 26.5* 2.2 25.3 27.6 25.4** 1.5 24.6 26.1 NS Inter molar width T0 44.2 2.1 43.1 45.3 44.8 3.4 43.1 46.6 44.7 2.6 43.4 46.1 NS Inter molar width T1 41.8*** 1.9 40.7 42.9 42.2** 2.6 40.9 43.5 43.0* 2.1 41.9 44.1 NS Inter molar width T2 41.9 1.7 41.0 42.8 41.6 2.7 40.2 43.0 41.5* 2.1 40.4 42.6 NS Inter molar width T3 40.9** 1.7 40.0 41.8 40.8*** 3.1 39.3 42.4 40.9** 2.7 39.4 42.3 NS Arch length T0 23.7 2.3 22.5 25.0 23.5 2.5 22.3 24.8 23.4 2.5 22.0 24.7 NS Arch length T1 17.9*** 1.3 17.2 18.6 17.9*** 1.7 17.0 18.8 17.4*** 1.3 16.7 18.1 NS Arch length T2 18.2 1.9 17.2 19.2 17.7 1.6 16.9 18.5 17.6 1.4 16.9 18.4 NS Arch length T3 17.1*** 1.7 16.2 18.0 17.3** 1.7 16.4 18.2 16.9*** 1.2 16.3 17.5 NS
NS indicates not significant, *p<0.05, **p<0.01, ***p<0.001 LII = Little´s Irregularity Index.
Table
5.
Mean pretreatment measurements (mm) for the mandible (T0), at the end of active treatment/star
t of the retention treatment (T1),
at the en d of two year s of retent ion treatme nt (T2), and a fter five or m ore years post-rete ntion (T3) i
n the three ret
ention group
s: removable
vacuum-for
med retainer (VFR) and bonded mandibular canine-to-canine retainer (V
-CTC), VFR and mandibular anterior stripping (V
-S),
and prefabricated positioner (P). W
Overbite and overjet T0-T3 (Table 6)
During the observation period, the overbite remained fairly stable and no intergroup differences were found.
During treatment (T0-T1), the overjet decreased significantly in all three groups, without any intergroup differences. At the end of the retention period (T2), the mean overjet was significantly higher in the V-S than in the V-CTC group, 3.8 versus 2.9 mm. After five years or more post-retention (T3), there were no significant intergroup differences in mean overjet.
OVERBITE V-CTC n=16 95 % Confidence Inter
val for Mean
V-S n=17
95
%
Confidence
Inter
val for Mean
P n=16
95
%
Confidence
Inter
val for Mean
ANOV A Mean SD Lower Bound Upper Bound Mean SD Lower Bound Upper Bound Mean SD Lower Bound Upper Bound T0 2.0 1.6 1.2 2.9 2.6 2.0 1.6 3.7 3.3 1.7 2.4 4.2 NS T1 2.1 0.9 1.6 2.6 1.8 0.7 1.5 2.2 2.3* 0.8 1.9 2.8 NS T2 1.6 1.1 1.0 2.2 2.5** 1.0 1.9 3.0 2.4 1.2 1.8 3.0 NS T3 1.8 1.6 1.0 2.7 2.6 1.3 1.9 3.3 2.7 0.9 2.3 3.1 NS OVERJET T0 4.5 2.0 3.4 5.6 5.6 2.6 4.3 6.9 5.7 2.6 4.4 7.0 NS T1 2.9* 0.6 2.6 3.2 3.2** 1.1 2.6 3.8 2.9*** 0.7 2.6 3.3 NS T2 2.9 1.1 2.3 3.4 3.8* 1.1 3.3 4.4 3.5* 1.0 3.0 4.1 0.040* V -CTC/V -S T3 3.7** 1.3 3.0 4.4 4.1 1.2 3.5 4.7 3.7 1.2 3.1 4.3 NS
NS indicates not significant, *p<0.05,**p<0.01, ***p<0.001.
Table
6.
Mean overbite and overjet (mm) pretreatment (T0), at the end of active treatment/star
t of the retention period (T1), at the end
of
the
two year retention
period (T2), and five or more years post-retention (T3) in the three
retention groups: removable
vacuum-for
med
retainer (VFR) and bonded mandibular canine-to-canine retainer (V
-CTC), VFR and mandibular anterior stripping (V
-S) and prefabricated
positioner (P). W
DISCUSSION
All three retention methods provided good long-term clinical stability after five years or more post-retention. Thus, in patients meeting the inclusion criteria, any of the three retention methods can be recommended.
Although there are a number of studies evaluating stability after orthodontic treatment (5, 7, 8, 15, 40), few are based on RCT (11-14, 28). These RCT studies analyse stability and relapse, but only in the short-term perspective. To our knowledge, this is the first RCT specifically designed to evaluate and compare three different retention strategies for retaining stability at least five years out of retention. Thus, no comparison of long-term stability can be made with previous studies; future studies are required to confirm our results.
Relapse
The results showed that most of the relapse occurred during the first year of retention, with only small changes during the second year, implying that the first year of retention is the most important in retaining the treatment result (Paper II, Table 2). These findings are consistent with those of Kuijpers-Jagtman (41), that 50 % of relapse occurred within the first two years of retention.
In the maxilla, small, but significant differences in tooth positions were noted after five years or more out of retention (T3) with differences in mean intercanine widths between groups V-S and P (Table 4). This might be attributable to the effect of the mandibular stripping in constructing a strong vault, thereby providing better
the mandible there was a significant difference in mean LII between groups V-S and P at T3 (Table 5).
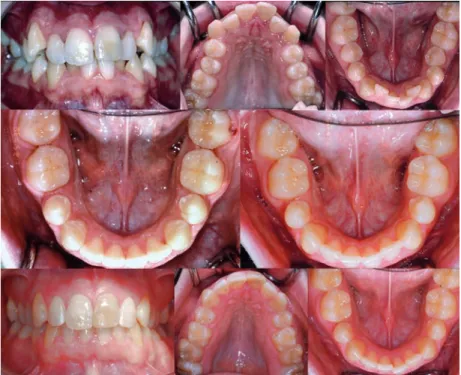
Figures 3, 4 and 5 show one case of severe mandibular LII from each retention treatment group at T0 and then the treatment results at T1, T2 and T3.
Figure 3. Group V-CTC. Five years post-retention.
Upper row: Anterior teeth, upper and lower arches before active treatment (T0), with a mandibular LII of 12.7 mm.
Middle row: Lower arch after active treatment and at the start of retention (T1) and at the end of two years of retention (T2).
Lower row: Anterior teeth, upper and lower arches at five years post-retention (T3), with a mandibular LII of 2.6 mm.
Figure 4. Group V-S. Nine years post-retention.
Upper row: Anterior teeth, upper and lower arches before active treatment (T0), with a mandibular LII of 15.8 mm.
Middle row: Lower arch after active treatment and at the start of retention (T1) and at the end of two years of retention (T2).
Lower row: Anterior teeth, upper and lower arches at nine years post-retention (T3), with a mandibular LII of 2.6 mm.
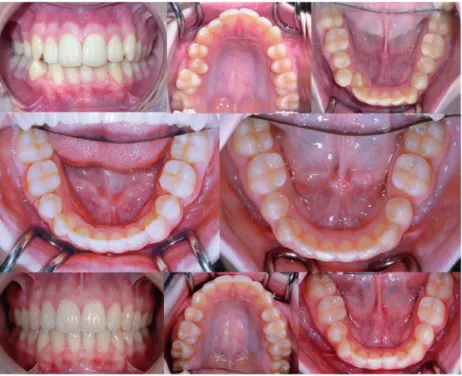
Figure 5. Group P. Five years post-retention.
Upper row: Anterior teeth, upper and lower arches before active treatment (T0), with a mandibular LII of 7.7 mm.
Middle row: Lower arch after active treatment and at the start of retention (T1) and at the end of two years of retention (T2).
Lower row: Anterior teeth, upper and lower arches at five years post-retention (T3), with a mandibular LII of 2.1 mm.
Methodological aspects
Papers I, II and IV
An RCT was selected in order to reduce the risk of error from such factors as selection bias, the clinician´s preferred treatment method and to ensure that patient compliance was equally distributed between groups. Furthermore, strict inclusion criteria and random allocation of subjects reduced bias and confounding variables by ensuring that both known and unknown determinants of outcome were evenly distributed among the subjects. The prospective design also ensured that the baseline characteristics, treatment progression, and side effects were strictly controlled and accurately observed.
The terms ”randomized controlled trial” and ”randomized clinical trial” are often regarded as synonymous. The ”C” in RCT stands for ”controlled”, signifying that the trial includes a ”control group” of untreated subjects. In the present studies, a group receiving no retention treatment would be irrelevant: the aim was to compare the outcomes of three different retention methods, not what would happen if subjects were left untreated. An alternative to non-treatment might be a previous treatment which had been tested for long-term stability. However, no such data were available.
The standardized treatment of all patients by the same orthodontic team made a valid comparison of the retention treatment methods. On the other hand, there is a potential drawback: the same possible errors may have been made on all patients.
In a long-term study, the effect of attrition on outcomes must be considered; some attrition is inevitable. Subjects will move out of the catchment area, increasing attrition and detracting from the evidential quality. In the present study the attrition rate was acceptable: according to the sample size calculation, the number of subjects remaining in each group was adequate to ensure that the outcomes were not biased by loss of data.
The ITT principle provides a high standard of analysis, as all patients are included in the results. In the present study, however, the PP-strategy was preferred, as it was difficult to account for missing measurements. At the final appointment of the trial, five years or more post-retention (Paper IV), 26 patients were unaccounted for, or could not be contacted. How should the missing patients be assessed, as failures or successes? It is probably incorrect to assume that all patients who failed to keep their appointments were failures. The subjects most likely to keep their appointments are presumably the dissatisfied ones. At T0, T1, T2 and T3, ten measurements of different characteristics were taken on every patient. What measurements should be allocated to the missing patients? To falsify figures or estimate measurements for patients failing to attend appointments is unlikely to have corrected the results, hence the PP-strategy was chosen for Papers I, II and IV.
VFR’s and positioners were worn part-time. This regimen was based on research showing equal stability of treatment results following full- or part-time wear of Essix retainers (11-14, 28).
The use of LII for measuring relapse of tooth positions may have some limitations: it tends to exaggerate cases with considerable irregularity but little length shortage, i.e. a rotated tooth without crowding (19). Another drawback is that it does not include the distal contact point of the canine. Thus canines may be in a very crowded position, but this may not be disclosed by the index (Figure 6).
Figure 6. Group V-S. Six years post-retention.
Upper row: Anterior teeth, upper and lower arches before active treatment (T0), with a mandibular LII of 8.0 mm.
Middle row: Lower arch after active treatment and at the start of retention (T1) and at the end of two years of retention (T2).
Lower row: Anterior teeth, upper and lower arches at six years post-retention (T3), with a mandibular LII of 1.8 mm.
Most patients had substantial pretreatment crowding (T0). In all groups, the mean LII after treatment (T1) was below or equal to 0.5 mm in both jaws, indicating successfully treated cases (Tables 4 and 5). However, the mean intercanine width in both jaws was generally somewhat expanded after treatment and relapse could be expected:
thus at the end of the observation period the intercanine widths had returned to pretreatment values in all groups. The mean changes of mandibular intercuspid distance and LII at T2 were similar to those confirmed by Renkema et al. (42), i.e. between 1.0 and 1.8 mm.
A crucial question in retention treatment planning is how long the patients should wear their retainers. In this study it was decided to discontinue all retention appliances after two years, as this was the customary period used by many Swedish orthodontists.
Paper III
After two years of retention treatment, the three retention methods were shown to be equally effective in retaining the treatment result and thus a cost-minimization analysis was carried out. The evaluation of treatment costs was based on the ITT approach, meaning that all cases, successful or not, were included in the analysis. The mean treatment times for taking impressions, bonding of CTC’s, stripping, and making and inserting VFR’s were estimated, on the basis of booked chairside time (Table 2). As treatment times were estimated and expected to be the same for each patient there was no statistical material to process. An alternative approach to timing would have been to use a stopwatch for every appointment included in the study, but this was impractical. The study subjects were treated in the same way as the other orthodontic patients. No retreatments were necessary during the retention period.
As the P-group required less chairside time, the societal costs were lower than in the V-CTC or V-S groups. Overall, indirect costs were fairly low as most of the patients were adolescents attending a high school located in the same small city as the orthodontic clinic. Indirect costs would be higher in larger cities with longer distances between schools and clinics. The catchment area for the patients represented a good average of Swedish socioeconomic status.
Costs are dependent on local factors such as staff, technicians and urban versus rural areas. Our orthodontic auxiliaries did the technical work for retention appliances and this reduced laboratory costs. If a local technician had made the VFR’s the societal cost would have been higher, not only because of the technician’s fee but also because the patient would have had to come back the next day, i.e. both direct and indirect costs would have been higher. The results