Experiences of Patients with
HIV/AIDS in Meeting with
Healthcare Professionals
på en eller
flera rader
HUVUDOMRÅDE: Nursing
FÖRFATTARE: Amina Aden, Fartum Farah, Katty Wiklund HANDLEDARE: Anna-Karin johansson, Julia Lindblom
JÖNKÖPING 2021 Jan
Summary
Background: Human immunodeficiency virus (HIV) is a global
epidemic. Lack of knowledge about the disease has increased the spread of the virus. There is a stigma around the disease, and patients with HIV/AIDS experience discrimination. The relationship between healthcare professionals, especially between nurses and their patients, should be based on HIV/AIDS knowledge and experiences. Aim: The aim of this study was to describe the experiences of patients living with HIV/AIDS in meeting with healthcare professionals. Method: A literature study was conducted based on 13 qualitative scientific articles. These articles were analysed and compiled based on Friberg's five-step model.
Results: The result was based on 13 qualitative scientific articles.
These results are presented in two main themes: patients experiencing positive encounters; and patients experiencing negative encounters with healthcare professionals. Experiencing positive encounters created two sub-themes: the value of knowledge and experience among healthcare professionals; and the importance of a respectful relationship. Negative encounters were divided into three sub-themes: patient experience of stigma and discrimination; inadequate and denied care; and breach of confidentiality by healthcare professionals. Conclusion: Patients living with HIV/AIDS describe both positive and negative experiences in meeting with healthcare professionals. Knowledge, experience, understanding, and empathy are required from nurses and other healthcare professionals in order to prevent stigma, discrimination, and negative attitudes.
Keywords: HIV / AIDS; patient perspective; person-centred
Patienter med HIV/AIDS och deras upplevelser av
mötet med vårdpersonal
En litteraturöversikt
Sammanfattning
Bakgrund: Humant immunbristvirus (HIV) anses vara en
epidemisk sjukdom som spridits över världen. Bristande kunskap om sjukdomen bidrar till ökad spridning av infektionen, diskriminering och stigma. Det är viktigt att vårdpersonalen ger patienter med HIV/AIDS förutsättningar för god och säker vård. Relationen mellan vårdpersonal och patienten måste därför kännetecknas av gott bemötande baserat på kunskap om och erfarenheter av sjukdomen. Syftet: Syftet med denna studie var att beskriva hur patienters med HIV/AIDS upplever möten med vårdpersonal. Metod: En litteraturöversikt genomfördes med hjälp av 13 kvalitativa vetenskapliga artiklar. Artiklarna analyserades utifrån Fribergs fem-stegs modell. Resultat: Resultatet baserades på 13 kvalitativa vetenskapliga artiklar. Resultatet presenteras i två huvudteman: patientens upplevelser av positiva och negativa bemötande från vårdpersonalen. Att uppleva positiva bemötande skapade två underteman; värdet av kunskap och erfarenhet bland vårdpersonal; och vikten av en respektfull relation. Negativa bemötande delades in i tre underteman: upplevelsen av stigmatisering och diskriminering; otillräcklig och förnekande av vård; och upplevelsen av sekretessbrott från vårdpersonalen. Slutsats: Patienter med HIV/AIDS beskrev både positiva och negativa upplevelser av möten med vårdpersonal. Kunskap, erfarenhet, förståelse och empati krävs av sjuksköterskor och annan vårdpersonal för att förebygga stigmatisering, diskriminering, och negativa attityder.
Nyckelord: HIV/AIDS, patientperspektiv, personcentrerad
Table of Contents
Introduction ... 1
Background ... 1
HIV/AIDS ... 1
Treatment for HIV/AIDS ... 2
Living With HIV/AIDS ... 3
The nurse's role in the Care of patients with HIV/AIDS ... 3
Person-Centred Care ... 4
Aim ... 5
Material and Method ... 5
Design ... 5
Selection and Data Collection ... 5
Data Analysis ... 7
Ethical Considerations ... 7
Results ... 8
Experiencing positive encounters ... 9
The value of knowledge and experience among healthcare professionals ... 9
The importance of a respectful relationship ... 10
Experiencing negative encounters ... 11
Stigma and discrimination ... 11
Inadequate Care and denied Care ... 12
Breach of confidentiality... 13
Discussion ... 14
Method Discussion ... 14 Results Discussion ... 16Conclusion ... 20
Clinical Implication ... 21
References ... 23
Appendix I: Search matrix ... 37
Appendix II: Article matrix ... 38
1
Introduction
Human Immunodeficiency Virus (HIV) is a global epidemic. Without treatment, HIV can develop into the most advanced stage of HIV infection: Acquired Immunodeficiency Syndrome (AIDS) (Tiraboschi, 2019). There are approximately 37.9 million people worldwide living with HIV/AIDS, of which 36.2 million are adults and 1.7 million are children under the age of 15 (WHO, 2018). According to the Swedish health and medical services act, the main goal in the healthcare system is to provide healthcare according to needs, on equal terms for the entire population (SFS: 2017:30). Life can be socially and mentally challenging for patients with HIV/AIDS due to experienced marginalisation and stigma in their society (Da Cruz et al., 2017). Stigma involves discrimination and negative attitudes based on specific characteristics or illness, such as HIV/AIDS. When facing a certain stigma, a person feels disgraced and disapproved as an individual (Emmanuel et al., 2009). HIV-related stigma can be experienced in healthcare settings, which can affect the patient's tendency to seek care and adherence to medication in order to manage the disease in long-term (Kalichman et al., 2011). Improved continuity of care, trust between patients and nurses, and continuous education and training are described as being essential parts of care for patients living with HIV/AIDS (Watson 2008). The emotional state and empathy of nurses play a key role in providing quality care and promotes communication to increase acceptance and understanding about HIV/AIDS (Downes & Foote, 2019).
Background
HIV/AIDSHuman immunodeficiency virus (HIV) infection is caused by the retrovirus. This virus is contagious except during the first few weeks of being infected or under antiretroviral medication (Bradbury & Samaras, 2008). HIV can spread through unprotected vaginal or anal sex; it is rarely infectious through oral sex. Other ways of transmission include sharing needles, contaminated blood transfusions, usage of contaminated surgical or sharp equipment. An infected woman can infect her child during pregnancy, through delivery, and the breastfeeding period (Tiraboschi, 2019).
2
HIV primarily lives and replicates in the human cell and, consequently, destroys the shape of the genetic mass (DNA) of the host cells. HIV infection is irreversible, has no cure, and is categorised as a chronic illness (Tiraboschi, 2019). HIV causes several immunological and physical changes in the person since the virus attaches to white blood cells. Physiological changes, such as osteoporosis, atherosclerosis, and neurocognitive decline occur due to the weakening of the immune system (Desai 2010).
According to Iweala (2004), there are different ways to test if a person is infected with HIV. Test from blood or a swab from mucous membranes identifies antibodies of the virus. Many international studies have reported frequent symptoms such as nausea, coughing, pain, anxiety, vomiting, diarrhoea, lack of appetite, fatigue, and anorexia in patients with HIV (Tsai et al., 2002; Peltzer & Phaswana-Mafuya, 2008). Fever, fatigue, and swollen glands are early signs of the HIV infection in both men and women (Peltzer & Phaswana-Mafuya, 2008).
Currently, 770 000 people die of HIV/AIDS -related illnesses every year with an estimation of 470 000 people dying annually from the disease in Africa (UNAIDS, 2019). The region being hit hardest by the global HIV epidemic is Sub-Saharan Africa, where socio-economic problems contribute to the increase and spread of HIV infection. The lack of access to healthcare, education, and other social services makes HIV prevention challenging (Kharsany & Karim, 2016). Unlike many developing countries, European nations have national guidelines and testing policies to provide the possibility of early diagnosis and access to antiretroviral treatment for HIV infections (Vermund et al., 2012). In Sweden, between 400- 500 cases of HIV are reported each year; however, more than half of these cases are from non-Swedes. Today, 8,000 people with HIV live in Sweden (Folkhälsomyndigheten, 2019).
Treatment for HIV/AIDS
Treatment begins with a combination of two to three different groups of antiretroviral medicine. Immediate treatment gives the best effect and improves long-term health, quality of life, and increases life expectancy (Kalichman et al., 2011). According to Chemtob et al. (2018), choosing suitable Anti-Retroviral Therapy (ART) is important in preventing illness and mortality. In high-income countries, the mortality of people infected with HIV has
3
decreased because of Highly Active Antiretroviral Therapy (HAART) (Chemtob et al., 2018).
Patients with HIV/AIDS can suffer from depression and anxiety disorders as they adjust to the diagnosis of a lifetime chronic disease. Therefore, it is important to assist a patient with counselling, such as behavioral activation for effective psychotherapy among patients with HIV/AIDS and their families in order to cope with the illness and discrimination (Moitra 2020).
Nurses are required to promote self-care, provide information to increase patient's HIV knowledge to manage the illness, and the prevention and treatment of mild and serious mental health problems (Lin et al., 2012).
Living With HIV/AIDS
Watson (2018) describes four categories of HIV/AIDS complexities: socio-economic, medical complexity, physiological, and other factors such as culture, faith, beliefs, and communication. Socio-economic complexity consists of isolation, poverty, and family issues that people with HIV/AIDS might face in society. Medical complexities include complications of medication, chronic pain, and cardiovascular disease. Sexually Transmitted Infections (STI) are common in people with HIV/AIDS, and this combination makes them (even more) contagious, and increases the risk to spreading STI to their partners (Kalichman et al., 2011). Psychological complexities such as stigma, anxiety, depression, and embarrassment negatively impact a patient’s well-being. A high level of stress and depression can contribute to a poor quality of life and health status (Effendy et al., 2019; Kolodziej., 2016).
The nurse's role in the Care of patients with HIV/AIDS
Many nurses may experience stress when caring for patients with HIV/AIDS. The stress is based on the risk of becoming infected and seeing patients suffer from their disease, which may hinder them to provide quality care (Seron et al., 2018). Nurses are required to be knowledgeable and confident in their role, and to build good relationships with their patients to enhance their trust for nurses (Relf et al., 2011). The International Council of Nurses' (2012) code of ethics defines the four fundamental responsibilities for nurses: to promote health, prevent illness, restore health, and alleviate suffering. The ethical codes for nurses demonstrate the professional's values, such as respect for the human rights. This
4
means giving equal care to all patients despite the background or beliefs, such as ethnic background, sexual orientation, social status, and political views.
Nurses are required to identify HIV-related complexities when assessing patients with HIV/AIDS to achieve holistic care (Watson, 2018). A holistic perspective means addressing the whole person, observing, and considering the patient's biological, social, psychological, and spiritual aspects in order to get a broader understanding of a patient's health situation (Mccance, 2003). Ross et al. (2015) describes nurses as understanding and providing safe care through compassion, courage, and commitment for patients with HIV/ AIDS. Depression, lack of social support, high levels of pain, stigma, stress, and physical inactivity for patients with HIV/AIDS can affect Health-Related Quality of Life (HRQol) (Chapman et al., 2019). Therefore, it is important for nurses to provide emotional support to the patients and their families (Lin et al., 2012).
Person-Centred Care
Person-centred care (PCC) plays an important role in improving healthcare and achieving general well-being: mental, physical, socio-cultural, and spiritual health (Mccance, 2003). Person-centred care means that care is given with dignity and respect for the patient in accordance with their needs and wishes. Person-centred care supports patients to exercise individual choice and autonomy in their healthcare decisions (Brummel-Smith et al., 2016). Every patient should be considered as a capable individual with the ability to make decisions regarding their health situation (Ekman, 2014).
Person-centred care focuses on the patient's need of care. Nurses should collaborate with different professional groups, such as medical doctors and therapists so the patient can achieve a high-quality care that respects and meets the individual's needs. Such nursing interventions have shown to improve patient experience, quality of care, and health outcomes (Ross et al. 2015). Patients provided with information about how to manage their disease, symptoms to look out for, and the risk and benefits of treatment are empowered to make their own decisions, while increasing confidence and self-determination in controlling their health situation (Náfrádi 2018).
5
Person-centred care provides opportunity for the patient to participate in decision making related to treatments and allows them to interact with health professionals through conversations and dialog (Abboah-Offei et al., 2019). The nurse’s ability to give support and quality care for patients with HIV/AIDS is based on the knowledge of how their patients interact with nurses and other healthcare professionals during their hospital visits. According to Relf et al. (2011), nurses must have the knowledge and professional skills to meet the demand of their expanding roles in healthcare.
Aim
The aim of this study was to describe the experiences of meetings with healthcare professionals for patients with HIV/AIDS.
Material and Method
DesignA literature review was conducted using an inductive approach based on qualitative scientific articles. The literature review aimed to collect existing research in order to get a clear picture of what was to be studied (Friberg, 2017a). According to Segesten (2017), it is appropriate to use a qualitative design when people's experiences or perceptions are examined. In the literature review, the aim was to describe the experiences of patients living with HIV and AIDS; therefore, a qualitative design was relevant for our study.
Selection and Data Collection
Database searches were done on two occasions: the first search was made with a helicopter perspective to verify the aim and that the requested material was available (Friberg, 2017a). A search was done for qualitative scientific articles in CINAHL, PubMed, MEDLINE and PsycINFO databases. The databases were chosen based on appropriateness and relativeness to the aim of the review (Karlsson, 2017). CINAHL contains material on nursing (Östlundh, 2017). PubMed and Medline are based on a nursing, medicine, and dentistry context from different journals (Karlsson, 2017). PsycINFO contains references of articles or books covering mainly psychology and medicine and psychiatry (Forsberg & Wengström, 2016). Before the database search, inclusion and exclusion criteria were established (Östlundh, 2017). Delimitation was made in the
6
databases to sort out irrelevant material for the study's aim (Friberg, 2017a). The delimitation made were peer-reviewed, written in English, and published during 2010-2020. Inclusion criteria was articles studying patients with HIV/AIDS experiences of meeting with healthcare professionals. Articles without abstracts and literature reviews were excluded.
Search terms used to find scientific articles were "HIV" and "AIDS", OR "human immunodeficiency virus", "People living with HIV and AIDS", OR "Patients with HIV/AIDS" OR "HIV-positive" AND "patients experiences" OR "patient's perspective" AND "nurses OR health care attitude", "Stigma", AND "qualitative study". Search terms varied depending on the databased used (Appendix I). Booleans search operators were applied to combine the selected terms in the search. The Boolean search operators were AND, OR. Truncation search method in which an asterisk (*) symbol was placed on the root of the term was used to help broaden the search (Östlundh, 2017).
During the searches, all titles/headlines were read and the articles relevant to the study's aim were selected for the result (Friberg, 2017a). The abstract of the selected articles was read to get an overview of the content, and articles that did not fit the study's aim were excluded. Searches in CINAHL resulted in 1052 articles, limited by headings, abstract availability, and with inclusion and exclusion criteria (Henricson 2017; Östlundh, 2017). The CINAHL database has functions to limit the search range; such functions are MeSH (Medical subject heading) and MH (major heading). Finally, twelve articles were selected for quality review, and then three articles were selected for the result, which wholly answered the study's aim. Same search procedure was used in PUBMED, and the search yielded 245 articles, of which nine articles were selected for quality review. These articles were read in their entirety to determine if the articles were consistent with the study's aim.
Three articles were relevant for the aim of the study (Appendix I). A further search was done in PsycINFO and Medline, and both searches were presented (Appendix I). A manual search was performed through the references from located articles. The manual search generated two relevant articles for the aim of the study, which was quality reviewed. One of the articles presented is a mix-method study design; however, the qualitative part included the patients' healthcare experience. A total of thirteen articles with 12 points in each article were selected after the quality review based on a protocol from School of Health and Welfare at Jönköping University (Appendix II). All articles with a score lower than 12 were excluded. Forty-seven out of sixty articles were excluded during the
7
quality-review (Appendix III). Four of the thirteen articles included were carried out in Canada, two in China, and one in Sweden, USA, Holland, South Africa, Ghana, and Ethiopia (Appendix II).
Data Analysis
Following the quality review, the 13 articles were analysed using the Friberg analysis model, which includes various steps to facilitate the analysis process (Friberg, 2017b). In the first step, the results of the articles were read with openness on several occasions with the attempt to understand the result. The articles were first read individually by the authors; then they were discussed in the group in order to understand the material. In the second step, the articles' results were read once more, and the text that corresponded to the aim of this study was highlighted. In the third step, the highlighted text was transferred to a separate document and compiled into similar units in order to obtain a clear overview of the articles' main findings. In the fourth step, the main findings were divided into themes and subthemes, which were later separated by identifying the similarities and differences in the articles. The text was objectively created in the fifth step, which generated a more in-depth and meaningful understanding of the themes and subthemes. Lastly, the result was presented based on the themes and subthemes that emerged throughout the text analysis. The study's result was formed as a new part of the analysis (Friberg, 2017b).
Ethical Considerations
Prior to the study, a level of pre-understanding was discussed among all three students; what emerged was a preconception, based on our university education and our work life experience. The results in the study may be influenced by the preconceived choice and interpretation of the analysis. To get an objective and consistent view, a discussion led to increased awareness and reflection of such risks throughout the work process (Priebe & Landström, 2017).
The articles included in our study were ethically reviewed according to the review protocol. According to Kjellström (2017), there must be an ethical consideration throughout the project. For literature reviews, no ethical approval is required; however, there should be an ethical stance regarding the articles used in the study's results. Ethical principles are established through the respect for human rights, fundamental freedoms, health, safety, and personal integrity. A participant's consent is essential. The researcher must
8
inform a participant of the aim of the research, protect privacy and confidential material, and respect a participants' right to consent. Moreover, the participants' information should only be used for purpose of study (Vetenskaprådet, 1990). Medical research must promote the participants' health and well-being, minimise risks, and protect their human rights (World Medical Association [WMA] declaration of Helsinki, 2013).
According to Kjellstöm (2017), the comparison between the benefit of the study and risks must be weighed; the respect for the participant's integrity is required to avoid any injury. Another risk is associated with the language; the articles selected for the study were in English, which could lead to misinterpreting of the results for a non-English speaking person. To reduce these risks, all three students read the articles, led discussions about individual interpretation, and translated all medical terms from English to Swedish or vice-versa with the help of Swedish MeSH.
Results
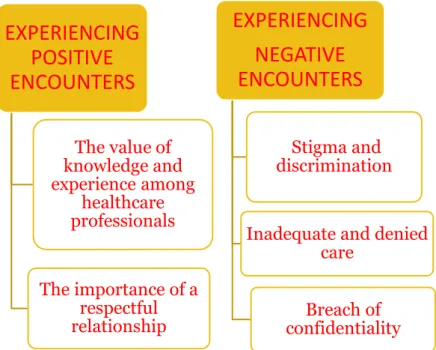
The result was based on data from 13 qualitative scientific articles. Features of the meeting with healthcare professionals (HCP) resulted in two main themes: experiencing positive encounters and experiencing negative encounters. Under “Experiencing positive encounters” two subthemes were found: the value of knowledge and experience among healthcare professionals and the importance of a respectful relationship. In comparison, the theme negative encounters resulted in three subthemes; experiencing stigmatization and discrimination; experiencing inadequate and denied care; and experiencing a breach of confidentiality from the healthcare professionals. The figure below presents the two main themes and the five sub-themes that corresponded to the results of the articles' main findings (figure.1).
9
Figure 1. Description of the two main themes and the five sub-themes
Experiencing positive encounters
Despite stigma and prejudice, we found that patients living with HIV/AIDS also experienced positive encounters in relation to healthcare professionals. Healthcare professionals used their knowledge during their hospital visits by showing respect and providing information and emotional support. As a result, patients felt valued and cared for, which enhanced their quality of life and trust for healthcare professionals: especially from nurses with whom they had the most interaction during their hospital appointments (Chen et al., 2010; Gagnon, 2015; Stuterheim et al., 2014); Donnelly et al., 2016).
The value of knowledge and experience among healthcare professionals
Patients with HIV/AIDS described their overall experiences as being positive in their meetings with healthcare professionals (HCP). They argued that treatment and nursing measures had improved compared to the early days regarding how patients were treated when the disease was viewed as deadly (Chen et al., 2010; Gagnon, 2015; Donnelly et al., 2016; Herder & Agardh, 2019). The patients described that HCP level of knowledge determined how patients were treated and whether their relationship could develop: either positively or negatively. For patients with HIV/AIDS, healthcare professionals with knowledge and experience on HIV/AIDS care have provided positive responses and better treatment. For instance, the patients received better treatment and easily accessed care from clinics within the HIV network compared to clinics outside the network. Clinics within the HIV network were
EXPERIENCING
POSITIVE
ENCOUNTERS
The value of knowledge and experience among healthcare professionals The importance of a respectful relationshipEXPERIENCING
NEGATIVE
ENCOUNTERS
Stigma and discriminationInadequate and denied care
Breach of confidentiality
10
able to create an atmosphere where patients felt welcomed and were seen as human beings and were treated with dignity by the nurses and other HCP (Wagner et al., 2016: Dako-Gyeke et al., 2015; Wodajo et al., 2017).
A study from Ghana emphasized how patients with HIV/AIDS travelled long distances to search for clinics within the HIV network (Dako-Gyeke et al., 2015). Patients saw HCP working at such clinics as being competent since they were specially trained in handling such healthcare settings. Patient experience was much more positive at these specialised clinics where nurses were able to see the patient from a holistic view and identified their patients´ real issues (Dako-Gyeke et al., 2015; Donnelly et al., 2016; Gagnon, 2015; Wagner et al., 2016).
The importance of a respectful relationship
Patients that considered having a respectful relationship with their healthcare professionals, especially nurses, related it to close contact and interaction with their nurse (Herder & Agardh, 2019; Dako-Gyeke et al., 2015: Gagnon, 2015; Donnelly et al., 2016). Patients felt that their relationship with nurses was integral for their well-being and quality of life. Trust was the key feature in the relationship; the patient tended to be open and genuine about the anamnesis. As a result, patients' well-being and care satisfaction improved (Herder & Agardh, 2019). Reaching the patient and creating trust through a respectful relationship was important in that the nurse listened to the patient’s problems (Dako-Gyeke et al., 2015: Donnelly et al., 2016). Patients described the nurses as having an approach that promoted a good relationship. They showed concern, spoke kindly, made eye contact, and smiled to patients during hospital appointments. Patients with HIV/AIDS felt valued and heard, which enhanced their confidence in nurses. Patients also preferred continuity: i.e., seeing the same nurse in order to avoid repeating their story to a new nurse who did not understand their situation (Okoro et al., 2014; Dako-Gyeke et al., 2015: Stuterheim et al., 2014); Donnelly et al., 2016).
A study from Sweden, focusing on homosexual men had generally conveyed positive encounters with the nurses through communication and building respectful relationships (Herder & Agardh, 2019). Also, clinics within HIV networks were perceived as creating a good atmosphere for patients with HIV/aids (Gagnon, 2015). One patient stated that nurses at the hospital where she was admitted were both supportive and helpful. Another patient said his HIV nurse was supportive of him and of his family and friends (Stutterheim et al., 2014).
11
Experiencing negative encounters
Several studies described how patients with HIV/AIDS experienced negative encounters with healthcare professionals (HCP), which created insecurities and fear. Such experiences were stigma, discrimination, and refusal, which led to constant fear of being denied care and distrust with nurses and other healthcare professionals (HCP). Stigma, breach of confidentially, and discriminatory attitudes from nurses and HCP mostly affected patient trust in healthcare plans and medication adherence. Therefore, the global health goal to reduce HIV infection and facilitate access to quality healthcare services for patients with HIV/AIDS could significantly be undermined by such treatment from the nurse (Wagner et al., 2016; Stutterheim et al., 2014; Okoror et al., 2014; Wodajo et al., 2017).
Stigma and discrimination
Several studies showed that healthcare professionals treated patients with HIV/AIDS poorly due to the stigma surrounding their HIV status (Stutterheim et al., 2014: Gagnon, 2015; Wagner et al., 2016. The nurses could ask irrelevant questions to the patients: such as how and when they got the HIV diagnosis (Stutterheim et al., 2014; Okoror et al., 2014; Ion & Elston, 2015). Patients also reported discriminatory behaviours from nurses: such as gossiping, using unnecessary precautions, an excessive curiosity regarding a patient’s HIV status, and showing discomfort when giving care (Gagnon, 2015; Wagner et al., 2016; Wodajo et al., 2017). Pregnant women living with HIV/AIDS experienced discrimination as they were tested for HIV without their knowledge or consent. These women also mentioned not receiving appropriate pre-or post-HIV test counselling. The nurses already assumed to know how these pregnant women contracted HIV and could be inappropriately labelled as having multiple partners or being a sex worker. Some were even told they did not deserve to give birth (Ion & Elston, 2015; Donnelly et al., 2016).
Homosexual patients with HIV/AIDS experienced prejudices, homophobic comments, and judgmental looks regarding their sexual orientation, thus, negatively influencing their interaction with nurses. Their previous experience with nurses led them to reluctantly disclosing their sexual orientation, fearing
12
discrimination, stigma, shame, and despair (Wagner et al., 2016; Ion & Elston, 2015). These patients also experienced receiving counselling on HIV transmission due to their sexual orientation instead of counselling regarding their sexual practices (Wagner et al., 2016). Groups such as gay men, homeless people, drug users, and sex workers experienced being intensely stereotyped, scrutinized, and categorized by HCP as being dangerous, infectious, careless, and dishonest. The patients were also labelled as faking their visit to the hospital in order to seek drugs. These stereotypes affected their perception of seeking and adhering to treatments (Ion & Elston, 2015; Wagner et al., 2016).
Marginalized groups in Canada - such as aboriginals, African, Latino and Asian patients living with HIV/AIDS stated they experienced stigma or feared being stigmatized concerning their meeting with healthcare professionals, which hindered them from accessing care (Donnelly et al., 2016). Nurses and HCP assumed that this patient group had contracted the disease through risky behaviours to which the patients exposed to themselves (Donnelly et al., 2016).
Inadequate Care and denied Care
Patients with HIV/AIDS described not been provided with adequate care, as the nurses and other healthcare professionals (HCP) lacked knowledge in HIV care, thus resulting in negative experiences (Dako-Gyeke et al., 2015). It was more frequent for patients to receive unfair treatment from HCP Clinics outside the HIV network. Nurses and other HCP at clinics outside the HIV network were perceived as being afraid of contracting HIV - even from patients with suppressed virology (Ion & Elston, 2015; Gagnon, 2015; Wagner et al., 2016; Dako-Gyeke et al., 2015). Patient experience in the different studies indicated that HCP, prior to specialising in HIV care, were perceived as being unprofessional and ignoring patients. This made the patients worry about what could go wrong and felt dependent on the nurse performing their work correctly (Wodajo et al., 2017; Gagnon, 2015; Dako-Gyeke et al., 2015; Donnelly et al., 2016; Chen et al., 2010).
Nurses’ lack of knowledge was observed, inadequate treatment and denied care for patients with HIV/AIDS was described (Wadojo, 2017; Abedinia et al., 2019). When patients sometimes visited hospitals for other health problems, their HIV diagnosis overshadowed their current health status, thus, resulting in frustration for the patient and delay of care. Patients with HIV/AIDS experienced being discharged whilst still in need of treatment without their knowledge (Abedinia et al., 2019). Wodajo
13
et al. (2017) mentioned that patients experienced delayed treatments after admission. Most hospitals in low and middle-income countries had no daily care plan for patients with HIV/AIDS (Wodajo et al., 2017; Abedinia et al., 2019; Okoror et al., 2014; Dako-Gyeke et al., 2015).
In the study from Sweden on homosexual men with HIV/AIDS, shortage or conflicting information from nurses regarding HIV infectiousness was expressed. They experienced that nurses were not transparent with their answers when patients asked if medication minimized HIV infectiousness and potential transmission to their partners. These patients instead sought information from public health, academic literature or HIV organizations. The patients’ lack support and counselling, made them worry about their long-term health and their way of living with the diagnosis (Herder & Agardh, 2019). These men wanted easily accessible information from the nurses and exact answers on their HIV infectiousness in order to calm their fears about infecting others (Herder & Agardh, 2019).
Abedinia et al. (2019) suggested that patients with HIV/AIDS in need of surgery or examination were refused treatment by HCP. One patient, admitted for acute abdominal pain, mentioned being denied endoscopy examination. Nurses and other HCP argued that the examination materials would be contaminated if they were used on patients who were HIV positive. Pregnant women with HIV/AIDS experienced being denied examination and being forced to fill in forms during their maternity visits regarding agreeing to abort their baby because of their HIV status (Abedinia et al., 2019; Wadajo et al., 2017; Chen et al., 2010).
Many studies suggest that patients with HIV/AIDS experienced a lack of collaboration among healthcare institutions (Abedinia et al., 2019; Wodajo et al., 2017; Chen et al. 2010). The patients also described being denied hospital sheets and bedding and being isolated from other patients. If bedding was not available, the patients were told to go to another hospital that could provide them with bedding or isolation rooms (Okoror et al., 2014; 2017; Chen et al., 2010: Abedinia et al., 2019; Wodajo et al., 2017).
Breach of confidentiality
It was common for patients with HIV/AIDS to experience breaches of confidentiality, as healthcare professionals revealed their HIV status without their consent (Okoror et al.,2014; Stutterheim et al.,
14
2014; Ion & Elston, 2015). Many patients often experienced negative and unfair treatment. These patients started having difficulty accessing health
care services in healthcare settings since their previous experience with healthcare professionals made them lose hope. This made the patients uncomfortable and worried of their status being openly disclosed since many of the patients were not open with their HIV diagnosis and had only shared it with their loved ones (Dako-Gyeke et al., 2015; Okoror et al., 2014). Several patients also felt that their integrity was ignored when accessing healthcare services. The patients described being in constant fear of their HIV status being openly disclosed at clinics; they felt ashamed to return to the hospital (Donnelly et al., 2016; Dako-Gyeke et al., 2015; Okoror et al., 2014).
It was common for healthcare professionals to disclose patient HIV status to other healthcare professionals or patients without patient consent. This was a violation of patient confidentiality while healthcare explained the action as safeguarding themselves (Gagnon, 2015; Okoror et al.,2014; Stutterheim et al., 2014; Ion & Elston, 2015). Patients with HIV/AIDS described a structural way of healthcare professionals revealing their HIV status; they had specific-colored medical journals assigned to HIV patients. These patients were scheduled specific days for clinic reception, and drapes separated them during examinations resulting in personal information being leaked to others (Dako-Gyeke et al., 2015; Okoror et al., 2014)
Discussion
Method Discussion
The following four concepts are important in providing the study's research quality: credibility, dependability, transferability, and reproducibility (Mårtensson & Fridlund, 2017b). According to Mårtensson and Fridlund (2017a), an inductive approach is relevant when searching a phenomenon objectively, and all material about the phenomenon is of interest.
The credibility of the literature review could be clarified if the study’s result is valid and the knowledge crated is reasonable. One way to demonstrate the credibility of the study is with help from fellow students and the supervisor, critical examine and helped revise and reform the literature review throughout the writing
15
process (Mårtensson &Fridlund, 2017b). The chosen method was required to answer the study's aim and achieve credibility (Mårtensson & Fridlund, 2017b). In addition, the selection of articles influenced the credibility of the literature review. Selected articles were taken from reliable databases: such as Cinahl, Pubmed, Medline, and PsychInfo and they contain journals about medicine and nursing (Karlsson, 2017). The reason for choosing several databases was to increase the search content and the credibility of the literature review (Henricson, 2017). Only peer-reviewed articles were included, which strengthened the credibility of the review (Henricson, 2017). Articles were quality reviewed with the help of School of Health and Welfare review protocol from the Department of Nursing at Jonkoping University (Appendix III). Only quality-reviewed articles were used in the literature review to strengthen its credibility.
Search terms used were determined to be relevant for the aim of the study, and the search was specified with the help of inclusion criteria. Forsberg and Wengström (2016) describe the importance of choosing a specific research area, limiting searches, and highlighting the importance of a critical approach during the reading and writing of the data selection and analysis of the result. If database search did not generate sufficient material, then manual searches were performed through the reference list. Two of the results articles were from year 2007 and 2001. These articles were seen to provide in-depth information about patients´ experience. Comparisons were drawn between these two articles and the remaining articles, which are presented in the results’ discussion section (Henricson, 2017). We chose healthcare professionals (HCP) because most of the scientific articles we read describe the nurse's area of responsibility and other professions that are part of the care chain where the nurses were included. We focused on bringing science-based knowledge to our studies of the nurse's role and responsibilities. Dependability is based on the awareness of preconceptions and its influence on the study. According to Mårtensson and Fridlund (2017b), perception and interpretation of information may depend on students' knowledge, language, and experience, which may influence the results' interpretations.
Transferability is about how the study results could be used in another context, groups, and situations (Mårtensson & Fridlund, 2017b). The articles used come from a variety of different countries, which can depend on culture, healthcare system, education, and economics. Nine of the 13 articles came from high-income countries; the remaining four were from low-income countries. One advantage of having articles from different countries or even continents is to obtain a more comprehensive picture of the phenomenon. A risk of having articles from various countries is
16
differences of point of views in the healthcare system, cultural, economic, and educational. As Sweden is becoming more multi-cultural, these results can be relevant in healthcare appointments with patients with HIV/AIDS coming from different backgrounds. It is noteworthy that most of the articles came from high-income countries, which still reported HIV-related stigma within healthcare settings.
In order to increase the study's reproducibility, a literature review should have a detailed description of the method through the transparent processing of data selection, collection, and data analysis. The study's reproducibility can be further strengthened if primary reference sources from scientific databases are used (Forsberg & Wengström, 2016), which is one of the study criteria. All articles were individually read during data analysis, discussed together, and data was objectively processed (Forsberg & Wengström, 2016; Henricson, 2017). Incomplete articles without an abstract were excluded. One disadvantage with this exclusion is that some articles may contain valuable information on the topic. To increase the review's reproducibility, all three students read the articles several times and highlighted key findings (Friberg, 2017a; Forsberg & Wengström, 2016; Henricson, 2017). The articles' main findings were discussed as much as possible to avoid individual influence (Mårtensson & Fridlund, 2017b).
Results Discussion
The analysis resulted in two themes and five subthemes considered to reflect the experiences of patients living with HIV/AIDS in their meetings with healthcare professionals. The two main themes were: experiencing positive encounters and negative encounters in healthcare settings. The results are discussed based on person-centred care, which is the theoretical framework of the literature review.
The study results indicated a strong need for knowledge and experiences in HIV and AIDS care among professionals (HCP) in healthcare settings. Patients described their encounters with healthcare professionals as both positive and negative. The patients associated positive encounters with being accepted, respected, and valued. Clinics within HIV networks were chosen over other clinics due to their effective care for patients with HIV/AIDS (Dako-Gyeke et al.,2015; Donnelly et al., 2016; Gagnon, 2015). Negative
17
encounters were associated with a lack of knowledge, which prompted stigma, discrimination, and healthcare refusal by healthcare professionals. Negative approaches toward patients with HIV/AIDS were common and expected of nurses and HCP in clinics outside HIV networks (Stutterheim et al., 2014; Okoror et al., 2014; Watson, 2018; Gagnon, 2015). The negative encounters were considered to be central to the main discussion since patients with HIV/AIDS belong to a vulnerable group of patients. The study indicated patients often experienced stigma and discrimination despite also experiencing positive encounters (Gagnon, 2015).
Experiences of Positive Encounters in Healthcare
The literature review revealed that patients with HIV/AIDS experienced positive encounters with healthcare professionals, especially with nurses, who possessed higher knowledge about HIV/AIDS. The patients described being secure, accepted, and understood by these nurses. Patients could be open about their issues and receive individual care. Nurses provided easy access to healthcare services with reliable and transparent competence and experience in HIV/AIDS care. Manganye et al. (2013) and Shahar et al. (2020) highlighted that nurses and HCP who have knowledge and experiences can communicate and interact better with the patients during their meetings. Educating and informing patients about their HIV, training on how to live with the disease, and giving advice on sexual health have shown to be the required measures in improving health-related quality of life for these patients (Brinsdon et al., 2017). The person-centred care concept implemented in healthcare settings in high-income countries focuses on patients as individuals with a disease. Still, implementation of patient-centred care for patients with HIV and AIDS seems to have its weaknesses (Morgan & Yoder, 2012). In low-income countries, the concept is relatively new in urban areas and was not recognized in rural areas (Abboah-Offei et al., 2019). According to Abboah-Offei et al. (2019) person-centred care supports nurse-patient relationships and promotes early detection and prevention of risk factors and comorbid illness; it also increases patient adherence to medication, which is vital in improving outcomes and evidence-based care. Person-centred care practices promote shared decision-making in healthcare settings and could reduce vulnerability. In addition, it promotes patients' knowledge and trust for HCP to facilitate their determination to engage in their treatment and long-term health.
Experiences of negative encounters in healthcare
Shahar et al. (2020) reported that healthcare professionals acknowledge the existence of HIV-related stigma and
18
discrimination, resulting in negative experiences and improper care for patients with HIV/AIDS in healthcare settings both in high and low-income countries. Gagnon (2015) reports stigma and discrimination in Canada's healthcare settings. According to Manganye el et. (2013), destructive or discriminatory behaviours negatively affect quality of care. Patients with HIV/AIDS experienced that healthcare professionals were reluctant to provide care in both income and low-income countries (Okoror et al., 2017). This undermines one of the global sustainable development goals of ensuring healthy lives and promoting well-being to all ages and reducing the HIV epidemic (UNAID, 2017). Previous healthcare experience affects patient's subsequent action, despite having skills and symptoms of illness (Okoro et al 2017).
The ICN code (2012) urge nurses to be familiar with the ethical, moral, and professional responsibility to give proper and quality care without discrimination, stigma, and prejudice. This code addresses all nurses and could be introduced in nursing programmes worldwide (ICN, 2012).
During the early years, when HIV/AIDS was a new phenomenon, and even more stigmatized, nurses and HCP often feared contamination (Webb et al., 2001; Chen et al., 2007). As of today, fear of HIV/AIDS still exists in both high and low-income countries. Different individual reactions or coping mechanisms can occur in healthcare (Gari et al., 2013). In high-income countries, HIV is treated with highly effective anti-retroviral therapy and patient's empowerment through education to help them take control of their situation (Shahar et al., 2020). While in low-income countries, nurses and other healthcare professionals have difficulty in reaching these patients to provide care, as well as educating patient with HIV/AIDS and their family members (Gari et al., 2013).
Seron et al. (2018) explains two strategies that could reduce stigma in caring for patients with HIV/AIDS: one is the nurse acknowledging his or her fears, concerns, and accepting the responsibility of providing optimal care for patients with HIV/AIDS. Another approach is improving communications between healthcare professionals and patients to reduce stigma and promote person-centred care practices. The trust between the patient and HCP is built on a long-term relationship, discussing each partner’s role, expectations upon appointments, and encouragement: such as showing respect in patient preferences and enhancing the patients’ willingness to engage in healthcare. This can apply to nurses in high and low-income countries in order for them to be able to build a respectful relationship with their patients with HIV/AIDS (Gari et al., 2013).
19
Our study results indicate other factors that intensify stigma and discrimination: such as ethnicity, gender, sexual orientation, and socio-economic status. Nurses in both high income and low-income countries have prejudice about who could contract HIV (Gari et al., 2013). According to Abboah-Offei et al. (2019), person-centred care is an important starting point for adequate care, communication, and clinical guidance. Nurses need to provide opportunities for patients to influence their care plan, given the chance of recovery and individual adaptation of care (Van Dongen et al., 2016). However, opportunities for patients can be different within high and low-income countries. Patients with HIV/AIDS in low-income countries mostly experience financial issues and the problem of availability of ARTs to access treatments. High-income countries can have different healthcare systems, leading to other and better conditions for these patients (Gari et al., 2013).
Another primary source of discrimination reported in high and low-income countries is the breach of confidentiality by healthcare professionals (HCP) when openly discussing the patients´ HIV status in the ward (Gari et al., 2013). This act is unacceptable and against the goal of equal rights and care in healthcare settings (SFS: 2017:30). According to the discrimination law (SFS: 2008: 567), nurses should provide equal care without discrimination and promote easy, accessible care. Brinsdon et al. (2017) propose that education not only negatively impacts behaviour; it changes attitudes towards patients with HIV/AIDS. Changes are required on a structural level to implement the behavioural change that hinders adequate care in high and low-income countries. For low-income countries, better financial support from the government level is needed, as well as better education and more awareness within societies (Gari et al., 2013).
Our study showed that the HCP did not provide adequate care and even refused to give care to patients with HIV/AIDS, which could affect the patients' trust that determined patients' willingness to seek or participate in their care. Fuller et al. (2017) suggest that HCP should inform and listen to patients' experiences and increase patient autonomous engagement and motivation in living with HIV and Aids. Since HIV is a long-term illness, the nurses and HCP in general, are required to monitor and support patients with HIV/AIDS by recording and reporting any improvements of the patients´ health status (Watson, 2018). Gari et al. (2013) confirm a lack of knowledge regarding treating patients with HIV/AIDS critical issues, especially infection pathways and treatment effectiveness. This could be the basis for developing a stigmatized view that is negative to the quality-of-care patients received. This
20
can be a problem within HCP in different healthcare sectors in high and low-income countries. Watson (2018) suggests that a person-centred care (PCC) approach can help nurses and all HCP identify and holistically assess these complexities in order to prevent poor quality care. An annual review and support of lifestyle change can help avoid health complexity and increase life expectancy and quality of life for these patients globally (Watson 2008; 2018).
Healthcare professionals in low and middle-income countries appear to be lacking core competencies in providing HIV and AIDS care. This could be noticeable as patients with HIV/AIDS generally experience negative encounters during their meetings with HCP, especially in HIV non-specific clinics (Relf et al., 2011). In high-income countries, the perception of HIV has drastically changed from a deadly to a manageable chronic illness due to suitable, improved, and accessible antiretroviral therapy (ART) (Shahar et al., 2020, Gari et al., 2013). In low and middle-income countries, patients with HIV/AIDS still experience stigma and discrimination in healthcare settings, which hinders patients from utilising healthcare services (Manganye el et. 2013). Patients with HIV/AIDS mentioned that low quality of healthcare contributed to impaired psychological health, resulting in high mortality of the disease in early age (Manganye el et. 2013).
Nurses are responsible for providing nursing care specific to the needs of the patient with HIV/AIDS. Therefore, it is crucial to create a framework from national governments, health ministries, educators, and external funders to ensure that healthcare professionals have the knowledge and skills required (Manganye el et., 2013, Shahar et al., 2020). However, low-income countries have a long way to go before reaching the same capacities in healthcare settings (Manganye el et., 2013; Gari et al., 2013). The same recommendations may also be needed in healthcare settings in high-income countries. Due to the low prevalence of patients with HIV/AIDS, a specific HIV/AIDS care based on the patient’s needs could therefore be inadequate (Gari et al., 2013; Shahar et al., 2020). Peltzer and Phaswana-Mafuya (2008) suggest that an improvement in healthcare on the hospital and community levels that values patients and family education and promotes empowerment and self-care for patients will help them in managing and control their long-term health.
21
The literature review describes patients with HIV/AIDS as experiencing positive and negative encounters in meetings with their healthcare professionals'. Adverse experiences were associated with a lack of knowledge and experiences within HCP. Lack of knowledge leads to discrimination and fear of contracting HIV, which results in stigma and care denial. The study shows that healthcare professionals, especially nurses, showed negative attitudes towards patients with HIV/AIDS. Therefore, there is a strong need for knowledge and understanding among nurses and other HCP about HIV/AIDS in how to care for all patients on equal terms. Person-centred care is one aspect that needs to be implemented in healthcare settings for patients with HIV/AIDS. By establishing mutual respect, information, access to care, and creating a partnership to help shared decision-making, person-centred care can be implemented. Patients express the desire for nurses to be knowledgeable about HIV/AIDS-related subjects in order to prevent stereotypical discriminatory approaches. The goal for all nurses is to strive for better healthcare on the individual, societal, and global levels. Our study indicates one area that needs to be further explored which includes the factors that can hinder the implementation of person-centred care as a framework for nurses in the global healthcare system.
Clinical Implication
The results of this study could help nurses to reflect on the change of individual and workplace perspectives to provide optimal care for patients living with HIV/AIDS. The study can provide insight into patient experience from care provided in these healthcare settings. Nurses can provide optimal care for patients with HIV/AIDS care by seeking knowledge and reflecting on their attitudes in meeting this group. Person-centred care is a nursing model that can help promote optimal treatment and care; it is considerate of and responds to the preferences, needs, and values of the individual patient with HIV/AIDS. There is good evidence that person-centred care approaches can improve safety, quality, patient satisfaction, and healthcare professional satisfaction. Recent research has shown that person-centred care practice has improved trust between nurses and their patients. More research is needed to describe nurses' attitudes towards patients living with HIV/AIDS from the patient's perspective.
23
References
*Results articles
Abboah-Offei, M., Bristowe, K., Koffman, J., Vanderpuye-Donton, N. A., Ansa, G., Abas, M., & Harding, R. (2019). How can we achieve person-centred care for people living with HIV/AIDS? A qualitative interview study with healthcare professionals and patients in Ghana. AIDS Care, 32(12), 1–10.
https://doi.org/10.1080/09540121.2019.1698708
* Abedinia, N., Rasoolinajad, M., Noorbala, A., & Badie, B. M.
(2019). I am HIV-positive, but I am a human being: qualitative study on experiences of stigma in health care centres in the Islamic Republic of Iran. Eastern Mediterranean Health Journal, 25(10), 669–676. https://doi.org/10.26719/emhj.19.012
Billhult, A., & Henricson, M. (2017). Kvalitativ metod. I M, Henricson (Red.) Vetenskaplig teori och metod: från idé till
examination inom omvårdnad (2:1 uppl.) (s.111–117).
Studentlitteratur AB
Bradbury, R. A., & Samaras, K. (2008). Antiretroviral therapy and the human immunodeficiency virus–improved survival but at what cost? Diabetes, Obesity and Metabolism, 10(6), 441–450
Brinsdon, A., Abel, G., & Desrosiers, J. (2017). "I'm taking control": how people living with HIV/AIDS manage stigma in health interactions. AIDS Care, 29(2), 185–188.
https://doi.org/10.1080/09540121.2016.1204420
Brummel‐Smith, K., Butler, D., Frieder, M., Gibbs, N., Henry, M., Koons, E., Loggers, E., Porock, D., Reuben, D., Saliba, D., Scanlon, W., Tabbush, V., Tinetti, M., Tumlinson, A., & Vladeck, B. (2016). Person‐Centered Care: A Definition and Essential Elements.
Journal of the American Geriatrics Society (JAGS), 64(1), 15–18.
https://doi.org/10.1111/jgs.13866
24
Chapman Lambert, C., Westfall, A., Modi, R., Amico, R., Golin, C., Keruly, J., (2019). HIV-related stigma, depression, and social support are associated with health-related quality of life among patients newly entering HIV care. AIDS
Care, ahead-of-print(ahead-of-print),1–8.
https://doi.org/10.1080/09540121.2019.1622635
Chemtob, D., Mor, Z., & Sheffer, R. (2018). Causes of death and mortality trends of all individuals reported with HIV/AIDS in Israel, 1985–2010. Journal of Public Health, 40(1), 56–64. https://doi.org/10.1093/pubmed/fdx039
* Chen W, Starks H, Shiu C, Fredriksen-Goldsen K, Simoni J,
Zhang F, Pearson C, & Zhao H. (2007). Chinese HIV-positive patients and their healthcare providers: contrasting Confucian versus Western notions of secrecy and support. Advances in
Nursing Science, 30(4), 329–342.
https://doi-org/10.1097/01.ans.0000300182.48854.65
* Chen, W.-T., Shiu, C.-S., Simoni, J., Fredriksen-Goldsen, K.,
Zhang, F., & Zhao, H. (2010). Optimizing HIV care by expanding the nursing role: patient and provider perspectives. Journal of
Advanced Nursing (John Wiley & Sons, Inc.), 66(2), 260–268.
https://doi-org/10.1111/j.1365-2648.2009.05165.
Da Cruz, D. S. M., dos Santos Cordeiro, R., Marques, D. K. A., & Silva, P. E. (2017). Experience of Patients with Hiv/Aids and the Influence of Religiousity/Spirituality When Coping the Disease.
Journal of Nursing UFPE / Revista de Enfermagem UFPE, 11(10),
4089–4095. https://doi.org/10.5205/reuol.10712-95194-3-SM.1110sup201711
* Dako-Gyeke, M., Dako-Gyeke, P., & Asampong, E. (2015).
Experiences of Stigmatization and Discrimination in Accessing Health Services: Voices of Persons Living With HIV in Ghana.
Social Work in Health Care, 54(3), 269–285.
https://doi-org/10.1080/00981389.2015.1005268
Desai, L. (2010). Early Immune Senescence in HIV Disease. Current HIV/AIDS Reports, 7(1), 4–10.
https://doi.org/10.1007/s11904-009-0038-4
25
SFS(2008:567).Discrimineringslagen
https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/diskrimineringslag-2008567_sfs-2008-567
* Donnelly, L. R., Bailey, L., Jessani, A., Postnikoff, J., Kerston, P.,
& Brondani, M. (2016). Stigma Experiences in Marginalized People Living With HIV Seeking Health Services and Resources in Canada. The Journal of the Association of Nurses in AIDS Care : JANAC, 27(6), 768–783.
https://doi-org/10.1016/j.jana.2016.07.003
Downes, R., & Foote, E. (2019). HIV and communication skills for practice. HIV Nursing, 19(4), 86–94.
Downes, R., & Foote, E. (2019). HIV and communication skills for practice. HIV Nursing, 19(4), 86–94.
Effendy, E., Amin, M., de Vega, L., & Utami, N. (2019). The
Association between CD-4 Level, Stress and Depression Symptoms among People Living with HIV/AIDS. Open Access Macedonian
Journal of Medical Sciences, 7(20), 3459–3463.
https://doi.org/10.3889/oamjms.2019.446
Ekman, I. (2014). Personcentrering inom hälso- och sjukvård:
från filosofi till praktik (1. uppl.) (21–36). Liber
Emmanuel Monjok, Andrea Smesny, & E. James Essien. (2009). HIV/AIDS - Related Stigma and Discrimination in Nigeria: Review of Research Studies and future directions for Prevention
Strategies. African Journal of Reproductive Health, 13(3), 21–36.
Friberg, F. (2017a). Att göra en litteraturöversikt. I F. Friberg (Red.), Dags för uppsats - vägledning för litteraturbaserade
examensarbeten (3 uppl.) (s. 141–152). Studentlitteratur AB.
Friberg, F. (2017b). Att bidra till evidensbaserad omvårdnad med grund i analys av kvalitativ forskning. I F. Friberg (Red.), Dags för
uppsats - vägledning för litteraturbaserade examensarbete (3
uppl.) (p. 129–139). Studentlitteratur AB.
26
Folkhälsomyndigheten (2019). Kunskap for hiv för hälso -och sjukvården. Retrieved 2020-02-27
from https://www.folkhalsomyndigheten.se/hividag/behandling
Forsberg, C., & Wengström, Y. (2016). Att göra systematiska
litteraturstudier: värdering, analys och presentation av omvårdnadsforskning (4 uppl.). Natur & Kultur
Fuller, S. M., Koester, K. A., Guinness, R. R., & Steward, W. T. (2017). Patients' perceptions and experiences of shared decision-making in primary HIV care clinics. Journal of the Association of
Nurses in AIDS Care, 28(1), 75–84.
* Gagnon, M. (2015). Re-thinking HIV-Related Stigma in Health
Care Settings: A Qualitative Study. The Journal of the Association
of Nurses in AIDS Care, 26(6), 703–719.
https://doi.org/10.1016/j.jana.2015.07.005
Gari, S., Doig-Acuña, C., Smail, T., Malungo, J. R., Martin-Hilber, A., & Merten, S. (2013). Access to HIV/AIDS care: a systematic review of socio-cultural determinants in low- and high-income countries. BMC Health Services Research, 13(1), 198.
Henricson, M. (2017). Diskussion. I M. Henricson (Red.),
Vetenskaplig teori och metod: från idé till examination inom omvårdnad (2:1 uppl.) (p. 411–420). Studentlitteratur AB
* Herder, T., & Agardh, A. (2019). Navigating between rules and
reality: a qualitative study of HIV positive MSM's experiences of communication at HIV clinics in Sweden about the rules of conduct and infectiousness. AIDS Care, 31(10), 1304–1310. https://doi-/10.1080/09540121.2019.1566590
International council of nurses ICN (2012). The ICN of ethics
for nurses. Hämtad
från https://www.icn.ch/sites/default/files/inline-files/2012_ICN_Codeofethicsfornurses_%20eng.pdf
27
* Ion, A., & Elston, D. (2015). Examining the Health Care Experiences of Women Living with Human Immunodeficiency Virus (HIV) and Perceived HIV-Related Stigma. Women's health
issues: Official Publication of the Jacobs Institute of Women's Health, 25(4), 410–419.
https://doi-org/10.1016/j.whi.2015.03.012
Iweala, O. I. (2004). HIV diagnostic tests: an overview.
Contraception, 70(2), 141-147. DOI:
https://doi.org/10.1016/j.contraception.2004.03.012
Kalichman, S. C., Cherry, C., Kalichman, M. O., Amaral, C. M., White, D., Pope, H., ... & Cain, D. (2011).
Integrated behavioral intervention to improve HIV/AIDS treatment adherence and reduce HIV transmission. American
Journal of Public
Health, 101(3),531538.https://ajph.aphapublications.org/doi/full/
10.2105/AJPH.2010.197608
Karlsson, E. (2017) Informationssökning. I M, Henricson (Red.)
Vetenskaplig teori och metod: från idé till examination inom omvårdnad (2:1 uppl.) (p. 81–93) Studentlitteratur AB
Kharsany, A. B., & Karim, Q. A. (2016). HIV Infection and AIDS in Sub-Saharan Africa:Current Status, Challenges and
Opportunities. The Open AIDS Journal, 10(1), 34–48. https://doi.org/10.2174/1874613601610010034
Kjellström, S. (2017). Forskningsetik. i M. H. (Red.), Vetenskaplig
teori och metod- från idé till examination inom omvårdnad (2:1
uppl.) (p. 57–77). Studentlitteratur.
Kołodziej, J. (2016). Effects of stress on HIV infection progression.
HIV & AIDS Review, 15(1), 13-16. https://doi.org/10.1016/j.hivar
Lin, C., Li, L., Wan, D., Wu, Z., & Yan, Z. (2012). Empathy and avoidance in treating patients living with HIV/AIDS (PLWHA) among service providers in China. AIDS Care, 24(11), 1341– 1348. https://doi.org/10.1080/09540121.2011.648602
28
Manganye, B. S., Maluleke, T. X., & Lebese, R. T. (2013).
Professional nurses' views regarding stigma and discrimination in the care of HIV and AIDS patients in rural hospitals of the
Limpopo province, South Africa. African Journal of AIDS
Research
(AJAR), 12(1),33-40. https://doi.org.proxy.library.ju.se/10.2989/16085906.2013.81 5411
Mccance, T. (2003). Caring in Nursing Practice: The Development of a Conceptual Framework. Research and Theory for Nursing
Practice, 17(2), 101–
116. https://doi.org/10.1891/rtnp.17.2.101.5317
Morgan, S., & Yoder, L. (2012). A Concept Analysis of Person-Centered Care. Journal of Holistic Nursing, 30(1), 6–15. https://doi.org/10.1177/0898010111412189
Moitra, T. (2020). Using Behavioral Psychotherapy Techniques to Address HIV Patients' Pain, Depression, and Well-Being.
Psychotherapy (Chicago, Ill.), 57(1), 83–89.
https://doi.org/10.1037/pst0000258
Mårtensson, J., & Fridlund, B. (2017a). Kritisk incidentteknik. I M, Henricson (Red.) Vetenskaplig teori och metod: från idé till
examination inom omvårdnad (2:1 uppl.) (P.155–167)
Studentlitteratur AB
Mårtensson, J., & Fridlund, B. (2017b). Vetenskaplig kvalitet i examensarbete. I M, Henricson (Red.) Vetenskaplig teori och
metod: från idé till examination inom omvårdnad (2:1 uppl.) (P.
421–436) Studentlitteratur AB
Náfrádi, N. (2018). An empirical test of the Health Empowerment Model: Does patient empowerment moderate the effect of health literacy on health status? Patient Education and Counseling, 101(3), 511–517. https://doi.org/10.1016/j.pec.2017.09.004
* Okoror, T. A., BeLue, R., Zungu, N., Adam, A. M., &
Airhihenbuwa, C. O. (2014). HIV Positive Women's Perceptions of Stigma in Health Care Settings in Western Cape, South Africa.
Health Care for Women International, 35(1), 27–49.