J Clin Nurs. 2021;00:1–27. wileyonlinelibrary.com/journal/jocn | 1 DOI: 10.1111/jocn.15832
R E V I E W
Models of support to family members during the trajectory of
cancer: A scoping review
Maria Samuelsson RN, RSCN, Doctoral Student
1,2
| Anne Wennick RN, RSCN, PhD, Senior
Lecturer
1
| Jenny Jakobsson RN, PhD, Associate Lecturer
1
| Mariette Bengtsson RN, PhD,
Associated Professor
1
This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
© 2021 The Authors. Journal of Clinical Nursing published by John Wiley & Sons Ltd.
1Faculty of Health and Society,
Department of Care Science, Malmö University, Malmö, Sweden
2Department of Pediatrics, Skåne
University Hospital, Malmö, Sweden Correspondence
Maria Samuelsson, Jan Waldenströms gata 25, 205 06 Malmö, Sweden.
Email: maria.samuelsson@mau.se Funding information
This research received no specific grant from any funding agency in the public, commercial or not- for- profit sectors.
Abstract
Aims and objectives: To map the existing literature on support models provided to
family members during the cancer trajectory.
Background: Cancer diagnosis, treatment and survivorship have a profound influence
on the surrounding family members. This scoping review is part of the development
of a support model for family members of persons diagnosed with colorectal cancer.
Design: The method was guided by the Arksey and O’Malley framework, described in
the Joanna Briggs Institute guidelines, and the reporting is compliant with PRISMA-
ScR Checklist. Searches were conducted in PubMed, CINAHL and PsycINFO from
November 2019– February 2020 with no limitation in publication year or study design.
Complementing searches were conducted in reference lists and for grey literature,
followed by an additional search in September 2020. Inclusion criteria were primary
research about support provided by health care, to family members, during cancer, of
an adult person, in Swedish or English, of moderate or high methodological quality.
Quality was assessed using the Joanna Briggs Institute critical appraisal tools. Data
were extracted using a charting form.
Result: A total of 32 studies were included in the review describing 39 support models.
Conclusion: The mapping of the existing literature resulted in the identification of
three themes of support models: psychoeducation, caregiver training and
psycho-logical support. In addition, that future research should target a specific diagnosis
and trajectory phase as well as include family members and intervention providers in
model development.
Relevance for clinical practice: Knowledge from the literature on both the needs of
the family members and existing support models should be incorporated with the
prerequisites of clinical practice. Clinical practice should also be complemented with
structured assessments of family members’ needs conducted regularly.
K E Y W O R D S
cancer, cancer trajectory, family, family caregivers, implementation, intervention, nurse,
psychosocial support, support model, supportive care
1 | INTRODUCTION
Cancer diagnosis, treatment and survivorship, described as the
can-cer trajectory, have a profound influence on the surrounding family
members. The impact of the diagnosis leads family members not only
to needing support of their own (Lambert et al., 2012; Lavallée et al.,
2019; Sklenarova et al., 2015) but also to having needs that shift
throughout the cancer trajectory (Given et al., 2012). Consequently,
numerous interventions combining information with emotional
sup-port have been designed to supsup-port family members (Treanor et al.,
2019). However, their effect on the family members’ quality of life
(QoL) is small and short lived. This, along with persistent reports
of unmet needs for emotional, informational and relational
sup-port (Lambert et al., 2012; Lavallée et al., 2019; Mollica et al., 2020;
Sklenarova et al., 2015), calls for increased focus on how to provide
adequate support. Consequently, this scoping review was designed as
an initial step in the development of a support model for family
mem-bers of persons diagnosed with colorectal cancer in Sweden. Before
designing a new intervention, examining the existing support models
appears beneficial. Thus, this scoping review was conducted to map
and review existing support models for family members of a person
diagnosed with cancer. To examine factors affecting the likelihood of
meeting the needs of family members, this study contrasts the
exist-ing support models against unmet needs described by Lambert et al.
(2012) and cancer trajectory phases described by Given et al. (2012),
since these are widely cited and clinically applicable.
In this scoping review, ‘family member’ is used when referring to
a person connected to the person stricken by cancer and to Wright
(2013) definition: ‘the family is who they say they are’. Thus, family
members also include, for example, next of kin and friends.
In addition, it encompasses ‘family caregiver’ and ‘informal
care-giver’. The rational to also including these roles are that the definition
of family caregiving by Weitzner et al. (2000) describes not only the
management of disease symptoms and treatment of side effects,
co-ordinating or administering treatments in the home, but also the
pro-viding of emotional support and assisting the person with activities
of daily living. This implies that the role of a family member and/or a
family caregiver appears to be close connected, or even intertwined,
and assumingly not static, meaning needs might change over time
re-lated to their level of engagement. Thus, as a result of this position, this
scoping review does not distinguish between being a family member
and a family caregiver when searching for models of support.
A cancer diagnosis not only affects the family members
them-selves but also challenges the relationships within the family,
es-tablished communication patterns, and roles and responsibilities
(Northouse et al., 2005). In addition, the role of the family members
during the cancer trajectory is multifaceted— comprising practical,
psychological and empathetic aspects (Blindheim et al., 2013). They
experience a physical, mental and emotional struggle. A cancer
di-agnosis even has a negative effect on the family members’ health;
for instance, they have higher rates of depression and weakened
im-mune response (Aizer et al., 2013), as well as increased risk of
isch-aemic heart disease (Mollerberg et al., 2016) and of coronary heart
disease and stroke (Ji et al., 2012). These risks persist over time.
Moreover, self- reported poorer QoL also persists through years
of survivorship, especially if the family members’ needs for
sup-port are not met during the cancer trajectory (Kim & Carver, 2019).
Consequently, researchers have emphasised the necessity of
focus-ing on family members as well as on the person diagnosed (Ji et al.,
2012; Kim et al., 2019; Norlyk & Martinsen, 2013). Lambert et al.
(2012) have categorised family members’ need for support in six
do-mains of unmet needs:
• Comprehensive cancer care, for example, being told about the help
healthcare professionals can offer, having possibilities to
partici-pate or help in the person's care and receiving appropriate
infor-mation from healthcare professionals.
• Emotional and psychological, for example, receiving help in dealing
with own emotional distress and getting emotional support for
self/having someone to talk to.
• Partner or caregiver impact and daily activities, for example,
receiv-ing financial support, help dealreceiv-ing with impact on work and help
looking after own health.
• Relationship, for example, receiving help communicating with the
person about illness and concerns and communicating with
oth-ers, such as family and friends.
• Information, for example, knowing what to expect from the illness,
treatment and prognosis.
• Spirituality, for example, feeling there is hope for the future and
receiving spiritual support.
The categories of unmet needs echo the patterns generally
re-ported in the cancer family caregiver literature (Chen et al., 2016; Girgis
et al., 2011; Osse et al., 2006); therefore, it is used in this scoping
re-view to contrast the existing models of support. In addition,
research-ers have proposed that the cancer trajectory significantly influences
what the family members need and when they need it (Given et al.,
2012; Northouse, 1984). Thus, meeting the needs of family members
requires recognising phase- specific problems and needs. The cancer
trajectory follows two winding paths that sometimes overlap, for
What does this paper contribute to the wider
global community?
• In general, the reviewed support models consider
nei-ther the impact of the specific diagnosis nor the cancer
trajectory, which may negatively affect the likelihood to
meet the family members’ needs.
• A majority of the support models reviewed contains
multiple components, and as a result, may be difficult to
apply in clinical practice.
• Future research needs to include the prerequisite of
clinical practice when designing support models, to
en-able for the support to be implemented and thus reach
the targeted family members
instance, in case of recurrence (Fletcher et al., 2012). One path leads
to palliative care and the end of life, and the other to rehabilitation and
survivorship. This scoping review focuses on the latter. Consequently,
to elucidate the support models’ recognition of the trajectory, we have
sorted all the reviewed models into a phase of relevance as described
by Given et al. (2012)— namely, diagnosis, treatment and survivorship.
Many interventions have been developed over the past
de-cades to support family members of persons with cancer. For
instance, systematic reviews have described interventions
aim-ing to support family caregivers in pain management (Chi et al.,
2020) and interventions aiming to improve cancer caregivers’ QoL
(Waldron et al., 2013). In addition, they have reported on
inter-ventions supporting family caregivers who care for persons with
advanced cancer at home (Ahn et al., 2020) and on interventions
aiming to improve the care for persons diagnosed with lung cancer
(Kedia et al., 2020). The effectiveness of cancer helplines has also
been systematically reviewed (Heckel et al., 2019). Fu et al. (2017),
Ferrell and Wittenberg (2017), and Applebaum and Breitbart
(2013) all reviewed randomised control trials of psychosocial
in-terventions. Further, Treanor et al. (2019) have discussed quasi-
experimental trials. To the best of our knowledge, no review has
been conducted aiming to include support models regardless of
study design. By doing so, this scoping review seeks to broaden
the picture of existing models and examine them in relation to
family members’ unmet needs— thereby elucidating the relevant
factors for designing support models for family members of
per-sons with cancer. In preparation for this scoping review, we made
searches to locate comparable, published or ongoing, scoping
re-views in PubMed, Cumulative Index to Nursing and Allied Health
Literature (CIHNAL), Cochrane Library and Joanna Briggs Institute
Systematic Review Register. However, none were identified.
2 | AIM
This scoping review aimed to map the existing literature on support
models provided to family members during the cancer trajectory.
Therefore, we asked the following research questions:
(i) What are the characteristics of the models described?
(ii) During which phase of the cancer trajectory is the described
support provided?
(iii) What are the aims of the support?
(iv) To whom is the support directed?
3 | METHOD
3.1 | Design
The study was designed as a scoping review. According to Arksey
and O'Malley (2005), this design allows for further exploration
by including unlimited study designs, settings and outcomes.
Furthermore, the design allows for additional questions to be
asked on the research topic of interest. The design and
implemen-tation were guided by a methodological framework developed
by Arksey and O'Malley (2005), refined by Levac et al. (2010)
and Colquhoun et al. (2014), and described by the Joanna Briggs
Institute (2015). Prior to the review, a protocol was constructed to
describe the planned methodology and search strategy (https://
bmjop en.bmj.com/conte nt/10/9/e0376 33.info). To achieve rigour,
the reporting was compliant with the Preferred Reporting Items
for Systematic reviews and Meta- Analyses extension for Scoping
Reviews Checklist (File S1). To enable replication and enhance
reli-ability, we documented the search and selection process using a
PRISMA flow chart (Figure 1).
3.2 | Data collection
3.2.1 | Search strategy
The Population Concept and Context (PCC) mnemonic
recom-mended for scoping reviews was used to establish effective search
criteria (Table 1).
The search strategy was developed in collaboration with a
re-search librarian well versed in using rere-search databases. An initial
broad search (e.g. next of kin, support and cancer) was conducted
in PubMed to inform the subsequent searches. In accordance with
recommendations from the research librarian, systematic searches
were conducted in PubMed, Cumulative Index of Nursing and
Allied Health and PsycINFO between November 2019– February
2020 (File S2), with no limitation in publication year or study
de-sign. An additional search was conducted in September 2020.
Search tools such as Medical Subject Headings, Headings,
Thesaurus and Boolean operators (AND/OR) were used to expand
and narrow the search. Keywords (e.g. ‘support’ and ‘neoplasm’)
and synonyms (e.g. ‘family’, ‘next of kin’ and ‘partner’) were
ap-plied to the different databases.
Grey literature identified in the databases was scoped to
iden-tify unpublished studies and ensure that no relevant reference
was missed. For the same reason, additional searches for grey
literature were conducted in Google Scholar and SwePub. Grey
literature identified included books, conference abstracts and
re-search posters.
3.2.2 | Inclusion criteria
The following inclusion criteria were applied: a primary research
in Swedish or English about support provided by healthcare
pro-fessionals to family members during the cancer trajectory of an
adult person. The reason for the limitation in language was that the
available resources of the research team were not enough to hire a
professional translator. In addition, the following exclusion criteria
were applied: first, to exclude studies describing support targeting
specific illness- related issues as they are not applicable to other
di-agnoses. Second, to exclude studies focusing on the
terminal/pal-liative phase and support postmortem as this study focuses on the
trajectory towards survivorship. Third and last, to exclude studies
focusing on children (< 18 years old) due to their specific needs of
support related to maturity.
A quality cut- off was set at studies not presenting one of the
following: aim, criteria for inclusion and exclusion, sample, data
collection, the process of analysis (all study designs), and a
descrip-tion and analysis of dropouts (quantitative studies). The radescrip-tionale
behind this decision was that their presentation of the support
models provided to family members would be incomplete without
this information. Consequently, these studies were categorised as
having ‘low quality’ and excluded (n=5; Table 2) whereas the
re-maining studies containing the required methodological
informa-tion were included. Assessment was conducted by two reviewers
independently and, if any disagreements, discussed in the research
team. To enable systematic exclusion of studies with incomplete
methodological description, the Joanna Briggs Institution Critical
Appraisal tools (Tufanaru et al., 2017)— ‘Checklist for Qualitative
Research’, ‘Checklist for Quasi- Experimental Studies’ and ‘Checklist
for Randomised Controlled Trials’, were used.
3.2.3 | Study selection
The study selection process is presented in a flow diagram (Figure 1).
First, all titles (6,140) were screened for relevance by the first
au-thor (MS) in collaboration with the librarian, consulting the research
team at any hesitation. Searches in grey literature and reference lists
identified another 33 studies. All relevant titles were imported into
a reference programme, Endnote X9, and checked for duplicates.
F I G U R E 1 PRISMA Flow diagram
Records iden fied through databasesearching in PubMed, Cinahl, PsychINFO
n= 6002
Addi onal search September n=138
Addi onal records iden fied through other sources, SwePub, Google scholar and reference lists
n= 33
Studies included in review n = 32
Full-text ar cles excluded due to methodology
quality n = 5 Full-text studies included in the cri cal
appraisal n = 37
Full-text ar cles assessed for eligibility n = 75
Full-text ar cles excluded, with reasons n = 38 Advanced cancer/Pallia on n = 8 Not able to separate from pa ent
outcome n = 11 Not primary research n = 12 Not provided by health care n = 2
No fulltext n= 3 Illess specific focus=2 Records excluded
n= 356 Records screened by abstract
n = 431
Records excluded n= 83 Records a er duplicates removed and
screened by tle n = 514
de
dul
cnI
ytil
ibi
gil
E
gni
ne
erc
S
oit
aci
fit
ne
dI
n
TA B L E 1
The PCC mnemonic as recommended by the Joanna
Briggs Institute
Participants Family members of a person diagnosed with cancer
Concept Support model
Context The cancer trajectory, both in a hospital and home setting
After removal of duplicates and screening of titles, 83 studies were
excluded due to being reviews, studies about instrumental
develop-ment or studies describing family caregiver needs. Second, 431
ab-stracts were screened and assessed with the inclusion criteria using
the Rayyan system for systematic reviews by Ouzzani et al. (2016).
The rational for using Rayyan is that its system enables a systematic
collaboration and sorting. To enhance the cohesion during the study
selection process, all abstracts were reviewed independently by two
reviewers. Eligible studies (75) were retrieved and read in full text
by the research team members, as described above regarding the
abstracts. Studies were assessed with the inclusion and exclusion
criteria using a charting form, and 38 studies were consequently
excluded.
3.2.4 | Data extraction
To maintain consistency across the different qualitative and
quan-titative approaches, the research team designed a data extraction
form when writing the protocol based on the research questions and
the recommendation by the Joanna Briggs Institute (2015). To
vali-date the extraction form for utility and completeness, three
mem-bers of the research team independently piloted the form on a study
of each study design included. This validation was conducted at the
beginning of the inclusion process and resulted in no corrections
needed. Apart from study characteristics, the following
informa-tion was extracted: support model (type of support, delivery mode
and intervention provider), phase of the trajectory (e.g. at
diagno-sis or during treatment), aim of the support and participating family
member.
3.3 | Analysis
In this scoping review, a semantic deductive thematic analysis
was conducted. This approach was chosen as it allows a
descrip-tive analysis, during which data were sorted using four research
questions as well as the six domains of unmet needs described
by Lambert et al. (2012) and mentioned in the introduction. Thus,
the deductive approach described by Braun and Clarke (2006), in
which the coding and theme development are directed by
exist-ing concepts or ideas, seemed most appropriate to answer the
re-search questions, resulting in the study protocol (which previously
stated that the analysis would follow an inductive approach) had
to be modified. Consequently, the analysis was directed by the
following:
(i) What are the characteristics of the models described?
(ii) During which phase of the cancer trajectory is the described
support provided?
(iii) What are the aims of the support?
(iv) To whom is the support directed?
First, the extracted data were read through and the parts
of text answering the research questions were highlighted and
sorted into new Microsoft Word documents named ‘model’,
‘tra-jectory’, ‘aim’ and ‘participating family member’. Data in the
docu-ment ‘trajectory’ were sorted into the trajectory phases described
by Given et al. (2012). Data in the document ‘models’ were further
divided into ‘description of the intervention’, ‘sessions’, ‘mode’
and ‘by whom’. Lastly, based on the description of the support,
the models grouped were divided into three themes. The models
identified were then compared with the unmet needs described by
Lambert et al. (2012).
3.4 | Consultation
In line with Arksey and O'Malley (2005) purpose of consulting with
stakeholders, contact nurses were approached with the preliminary
results and asked to offer additional information, perspective,
mean-ing and thoughts on applicability. A contact nurse is a registered
nurse with specialist knowledge in oncological and psychosocial care
who is assigned to support both the person diagnosed and their
fam-ily members throughout the cancer trajectory. A total of five contact
nurses were asked to take part in this process and reflect over the
schematic results’ relevance and applicability to clinical practice. The
contact nurses were from two regions in Sweden and cared for
per-sons with gastrointestinal, urological and breast cancer. A telephone
or digital meeting was arranged with each nurse individually at their
convenience. The contact nurses recognised the content in the
support models as part of the support they provided and
acknowl-edged its importance. However, they did not provide such support
in a structured manner. Instead, they offered support when a need
was identified, for example, if a family member contacted them and
expressed a wish for information. Furthermore, they found the
sup-port models difficult to apply, due to both lack of time and lack of
knowledge.
Author, year, country
No data collection No aim No inclusion/ exclusion criteria No analyse of dropouts
Barg et al. (1998), USA x x x
Saita et al. (2014), Italy x x x
Toseland et al. (1995), USA x
Walsh et al. (2004), USA x
Walsh- Burke et al. (1992), USA x
TA B L E 2
Studies excluded due to
TA B L E 3
Included studies
Author, year, country Aim Design Participants Diagnosis
1. Arnaert et al. (2010), Canada To explore the experiences of cancer patients’ relatives attending a non- residential, 2.5- day retreat
Qualitative, semi- structured interviews Eight relatives (seven women, one man) Not Stated 2. Badger et al. (2013), USA To test the effectiveness of two psychosocial interventions for improving QoL in recently
diagnosed breast cancer survivors and their partners, and to test the efficacy of two delivery methods (telephone and videophone)
Quasi- experimental 49 partners Breast
3. Badger et al. (2011), USA To test the effectiveness of two telephone- delivered psychosocial interventions for maintaining and improving QoL
Quasi- experimental 71 patients and 70 social network members Prostate 4. Badger et al. (2020), USA To compare the effectiveness of two 8- week telephone- delivered interventions designed
for Latina breast cancer survivors in treatment and their informal caregivers who participated in the study with the survivors
Quasi- experimental 241 patients and 230 caregivers Breast
5. Badr et al. (2016), USA To develop and evaluate a dyadic web- based intervention Qualitative, semi- structured interviews 16 patients and 12 caregivers Oral cancer
6. Bahrami and Farzi (2014), Iran To define the effect of a supportive educational programme based on the COPE model on the promotion of quality life and reduction of family caregivers’ burden of caring for women with breast cancer
Quasi- experimental 64 caregivers Breast
7. Belgacem et al. (2013), France To assess the efficacy of the programme by monitoring the evolution of the QoL of patients and caregivers alike and the physical, psychological, and social burden experienced by caregivers; to investigate the effects of the programme on the relationship between patients and healthcare providers by measuring patient satisfaction
Multicentre RCT 33 patients and 34 caregivers Multiple (haematological and oncological)
8. Birnie et al. (2010), Canada To explore MBSR participation for couples affected by cancer. In particular, it examines the programme's impact on symptoms of stress, mood disturbance, and mindfulness for both cancer patients and their partners; it also begins to explore relationships between couples’ outcomes.
Quasi- experimental 21 couples Multiple (most common are prostate,
breast, and colon)
9. Budin et al. (2008), USA To conduct a randomised controlled clinical trial of phase- specific evidence- based psychoeducation and TC interventions to enhance emotional, physical, and social adjustments in patients with breast cancer and their partners
RCT 249 patient- partner dyads Breast
10. Carlson et al. (2017), Canada To report the results of a negative randomised controlled trial that piloted brief supportive- expressive therapy (SET) for partners of men with prostate cancer and to discuss lessons learned for future clinical trials
RCT 77 partners Prostate
11. Carlsson and Strang (1998), Sweden To evaluate whether educational groups have an effect on the perceived level of knowledge and whether this has a positive effect on mood
Quasi- Experimental 32 patients and 8 next of kin; 25 patients in control group
Gynaecological 12. Chambers et al. (2014), Australia To compare the effectiveness of two low- intensity approaches for distressed patients with
cancer and caregivers who had called cancer helplines seeking support RCT 354 patients and 336 caregivers Not Stated
13. Chien et al. (2020), Taiwan To understand the effectiveness of a couple- based psychosocial information package (PIP) and multimedia psychosocial intervention (MPI) on patients with prostate cancer and their partners
Quasi- Experimental 103 patients and 103 partners Prostate
14. Chiquelho et al. (2011), Portugal To describe proFamilies: a psychoeducational multi- family discussion group intervention for cancer patients and their families
Quasi- Experimental; qualitative focus group interviews
22 family members Not Stated
15. Gabriel et al. (2019), South Africa To implement and evaluate the effectiveness of a psychosocial intervention programme on the QoL and caregiver burden of the primary caregivers of women with breast cancer
Quasi- Experimental 108 caregivers Breast
16. Gjerset et al. (2019), Norway To investigate differences between female and male caregivers regarding (a) health status at the start of the 1- week educational programme and at 3 months after termination, (b) self- reported needs for support at the start of the programme, and (c) changes in health status from the start to 3 months after termination of the programme
Quasi- Experimental 115 partners Not Stated
17. Heckel et al. (2019), Australia To evaluate the utility of a telephone outcall programme for cancer caregivers and to examine longitudinal changes in their distress levels and supportive care needs
RCT 108 caregivers Not Stated
18. Heinrichs et al. (2012), Germany To investigate the short- and long- term efficacy of a couple- based psychosocial
intervention for couples faced with female breast- or gynaecological cancer RCT 72 couples Multiple (breast or gynaecological)
19. Hendrix et al. (2013), USA To investigate the effects of an individualised caregiver training intervention on caregiver's self- efficacy in home care and symptom management; to investigate whether the caregiver training intervention has an effect on caregivers’ psychological well- being (i.e. depression, anxiety and quality of life)
RCT 120 patient– caregiver dyads Haematological
20. Köhle et al. (2017), Netherlands To examine user- experiences with a web- based self- help intervention based on ACT and self- compassion among partners of cancer patients
Qualitative, individual semi- structured interviews 20 partners Multiple (colon, Kahler's, lung, prostate, leukaemia, bladder, lymph node, pancreas, head and neck, and breast)
TA B L E 3
Included studies
Author, year, country Aim Design Participants Diagnosis
1. Arnaert et al. (2010), Canada To explore the experiences of cancer patients’ relatives attending a non- residential, 2.5- day retreat
Qualitative, semi- structured interviews Eight relatives (seven women, one man) Not Stated 2. Badger et al. (2013), USA To test the effectiveness of two psychosocial interventions for improving QoL in recently
diagnosed breast cancer survivors and their partners, and to test the efficacy of two delivery methods (telephone and videophone)
Quasi- experimental 49 partners Breast
3. Badger et al. (2011), USA To test the effectiveness of two telephone- delivered psychosocial interventions for maintaining and improving QoL
Quasi- experimental 71 patients and 70 social network members Prostate 4. Badger et al. (2020), USA To compare the effectiveness of two 8- week telephone- delivered interventions designed
for Latina breast cancer survivors in treatment and their informal caregivers who participated in the study with the survivors
Quasi- experimental 241 patients and 230 caregivers Breast
5. Badr et al. (2016), USA To develop and evaluate a dyadic web- based intervention Qualitative, semi- structured interviews 16 patients and 12 caregivers Oral cancer
6. Bahrami and Farzi (2014), Iran To define the effect of a supportive educational programme based on the COPE model on the promotion of quality life and reduction of family caregivers’ burden of caring for women with breast cancer
Quasi- experimental 64 caregivers Breast
7. Belgacem et al. (2013), France To assess the efficacy of the programme by monitoring the evolution of the QoL of patients and caregivers alike and the physical, psychological, and social burden experienced by caregivers; to investigate the effects of the programme on the relationship between patients and healthcare providers by measuring patient satisfaction
Multicentre RCT 33 patients and 34 caregivers Multiple (haematological and oncological)
8. Birnie et al. (2010), Canada To explore MBSR participation for couples affected by cancer. In particular, it examines the programme's impact on symptoms of stress, mood disturbance, and mindfulness for both cancer patients and their partners; it also begins to explore relationships between couples’ outcomes.
Quasi- experimental 21 couples Multiple (most common are prostate,
breast, and colon)
9. Budin et al. (2008), USA To conduct a randomised controlled clinical trial of phase- specific evidence- based psychoeducation and TC interventions to enhance emotional, physical, and social adjustments in patients with breast cancer and their partners
RCT 249 patient- partner dyads Breast
10. Carlson et al. (2017), Canada To report the results of a negative randomised controlled trial that piloted brief supportive- expressive therapy (SET) for partners of men with prostate cancer and to discuss lessons learned for future clinical trials
RCT 77 partners Prostate
11. Carlsson and Strang (1998), Sweden To evaluate whether educational groups have an effect on the perceived level of knowledge and whether this has a positive effect on mood
Quasi- Experimental 32 patients and 8 next of kin; 25 patients in control group
Gynaecological 12. Chambers et al. (2014), Australia To compare the effectiveness of two low- intensity approaches for distressed patients with
cancer and caregivers who had called cancer helplines seeking support RCT 354 patients and 336 caregivers Not Stated
13. Chien et al. (2020), Taiwan To understand the effectiveness of a couple- based psychosocial information package (PIP) and multimedia psychosocial intervention (MPI) on patients with prostate cancer and their partners
Quasi- Experimental 103 patients and 103 partners Prostate
14. Chiquelho et al. (2011), Portugal To describe proFamilies: a psychoeducational multi- family discussion group intervention for cancer patients and their families
Quasi- Experimental; qualitative focus group interviews
22 family members Not Stated
15. Gabriel et al. (2019), South Africa To implement and evaluate the effectiveness of a psychosocial intervention programme on the QoL and caregiver burden of the primary caregivers of women with breast cancer
Quasi- Experimental 108 caregivers Breast
16. Gjerset et al. (2019), Norway To investigate differences between female and male caregivers regarding (a) health status at the start of the 1- week educational programme and at 3 months after termination, (b) self- reported needs for support at the start of the programme, and (c) changes in health status from the start to 3 months after termination of the programme
Quasi- Experimental 115 partners Not Stated
17. Heckel et al. (2019), Australia To evaluate the utility of a telephone outcall programme for cancer caregivers and to examine longitudinal changes in their distress levels and supportive care needs
RCT 108 caregivers Not Stated
18. Heinrichs et al. (2012), Germany To investigate the short- and long- term efficacy of a couple- based psychosocial
intervention for couples faced with female breast- or gynaecological cancer RCT 72 couples Multiple (breast or gynaecological)
19. Hendrix et al. (2013), USA To investigate the effects of an individualised caregiver training intervention on caregiver's self- efficacy in home care and symptom management; to investigate whether the caregiver training intervention has an effect on caregivers’ psychological well- being (i.e. depression, anxiety and quality of life)
RCT 120 patient– caregiver dyads Haematological
20. Köhle et al. (2017), Netherlands To examine user- experiences with a web- based self- help intervention based on ACT and self- compassion among partners of cancer patients
Qualitative, individual semi- structured interviews 20 partners Multiple (colon, Kahler's, lung, prostate, leukaemia, bladder, lymph node, pancreas, head and neck, and breast)
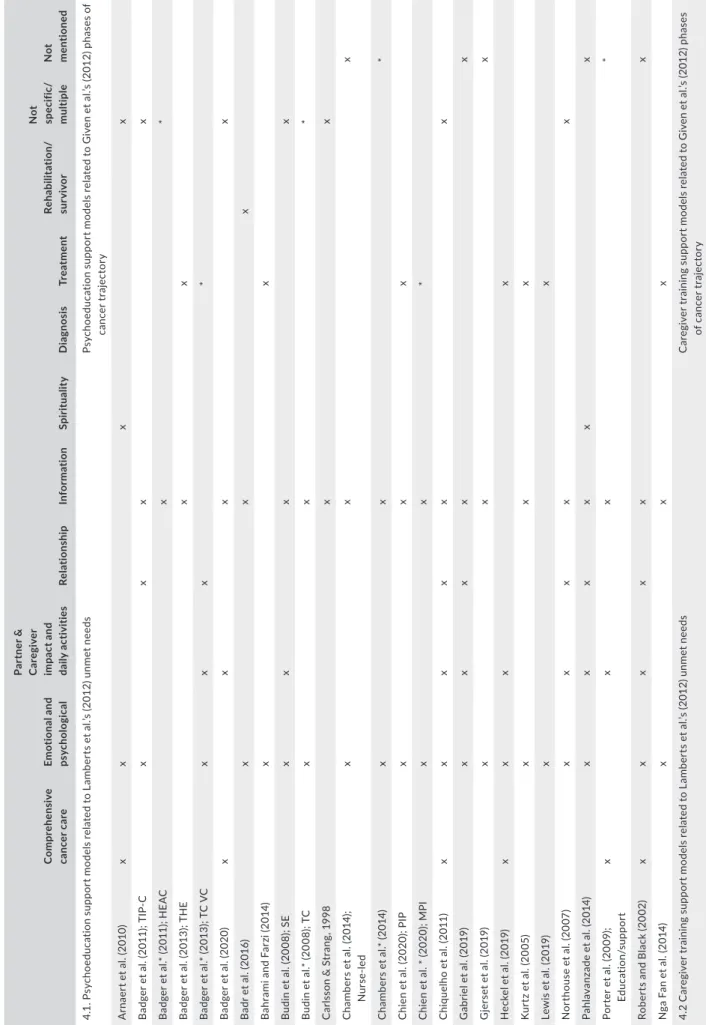
4 | RESULTS
This scoping review includes 32 studies published between 1998–
2020. The included studies contain the designs of randomised
con-trolled trials (n = 17), quasi- experimental trials (n = 11), a combination
of quasi- experimental and qualitative focus group interviews (n = 1)
and qualitative studies (n = 3). The cancers in focus are breast (n =
6), prostate (n = 4), lung (n = 2), haematological (n = 1), colorectal (n
= 1), oral (n = 1), leukaemia (n = 1) or multiple/not mentioned (n =
16). Characteristics of the included studies are presented in Table 3.
The included studies describe 39 support models provided to family
members during the cancer trajectory, presented in three themes:
psychoeducation (n = 26), caregiving training (n = 6) and
psycho-logical support (n = 7). Each theme describes how, by whom and to
whom the support is provided. Table 4 offers detailed information
on the aim and design of the support models. Table 5 relates the
support models to the six domains of unmet needs described by
Lambert et al. (2012) and shows during which trajectory phase the
support was provided as described by Given et al. (2012).
4.1 | Psychoeducation
Out of the 32 studies reviewed, 19 described 26 different
psychoe-ducational support models provided to family members during the
cancer trajectory. The models predominately addressed the
treat-ment phase of the cancer trajectory and were focused on addressing
emotional and psychological unmet needs, unmet needs related to
the partner or caregiver impact and daily activities, and relational
and informational unmet needs.
Author, year, country Aim Design Participants Diagnosis
21. Kozachik et al. (2001), USA To determine the impact of a 16- week supportive nursing intervention on caregivers of patients with newly diagnosed cancer
RCT 125 dyads Multiple (breast, colon, lung, non-
Hodgkin's lymphoma, and pancreas) 22. Kuijer et al. (2004), NZ Explored to what extent a decrease in perceived equity after the intervention could
predict relationship quality and psychological distress directly after the intervention and 3 months later To explore to what extent a decrease in perceived equity after the intervention could predict relationship quality and psychological distress directly after the intervention and 3 months later
RCT 59 dyads Not Stated
23. Kurtz et al. (2005), USA To determine whether a clinical nursing intervention focusing on teaching caregivers and their cancer patients’ skills to better manage the symptoms would reduce caregiver depressive symptomatology
RCT 237 dyads Not Stated
24. Lewis et al. (2019), USA To test the short- term efficacy of a brief, fully manualised marital communication and interpersonal support intervention for couples facing recently diagnosed breast cancer
RCT 322 pairs Breast
25. Northouse et al. (2007), USA To determine whether a family- based intervention could improve appraisal variables (appraisal of illness or caregiving, uncertainty, hopelessness), coping resources (coping strategies, self- efficacy, communication), symptom distress, and quality of life in men with prostate cancer and their spouses
RCT 235 couples Prostate
26. Porter et al. (2009), USA To determine the efficacy of a novel partner- assisted emotional disclosure intervention in a sample of patients with gastrointestinal (GI) cancer
Quasi- experimental 130 couples Multiple (GI- cancers)
27. Porter et al. (2011), USA To determine the efficacy of a caregiver- assisted CST protocol in a sample of patients with
lung cancer RCT 233 dyads Lung
28. Roberts and Black (2002), Australia To report the results of an evaluation of an Australian education and support programme for individuals with cancer and their family and friends— the Living with Cancer Education Programme (LWCEP)
Quasi- experimental 576 family members and friends Not Stated
29. Schellekens et al. (2017), Netherlands he aim of this study was to examine the effectiveness of MBSR added to CAU compared to CAU alone to reduce psychological distress in patients with lung cancer and/or their partners he aim of this study was to examine the effectiveness of MBSR added to CAU compared to CAU alone to reduce psychological distress in patients with lung cancer and/or their partners
To examine the effectiveness of MBSR added to CAU compared to CAU alone in reducing psychological distress in patients with lung cancer and/or their partners
RCT 63 patients and 44 partners Lung
30. Sherwood et al. (2012), USA To determine, in patients with solid tumours, whether a nurse- delivered symptom management intervention was more effective than a coach- led intervention in increasing caregiver involvement in symptom management and improving caregivers’ emotional health
RCT 225 family caregivers Not Stated
31. Nga Fan et al. (2014), Hong Kong To evaluate the efficacy of the programme in reducing depression, anxiety, stress, and burden of care among carers of patients with colorectal cancer
RCT 140 carers Colorectal
32. Pahlavanzade et al. (2014), Iran To determine the effect of a family need- based programme on the burden of care in caregivers of leukaemia patients
RCT 70 caregivers Leukaemia
In the reviewed studies, psychoeducation contained both
self- therapeutic and diagnosis- related education. This support
model combined various educational approaches, and apart from
one single- session nurse intervention (Chambers et al., 2014), it
was provided in a series of sessions. The support was provided
using telephone (Badger et al., 2013; Badger et al., 2011; Badger
et al., 2020; Budin et al., 2008; Chambers et al., 2014; Heckel
et al., 2019; Nga Fan et al., 2014), a combination of in person and
telephone (Bahrami & Farzi, 2014; Kurtz et al., 2005; Northouse
et al., 2007), video (Badger et al., 2013; Budin et al., 2008), a
webpage (Badr et al., 2016) or a retreat weekend (Arnaert et al.,
2010). In four studies, the support was provided as group sessions
(Carlsson & Strang, 1998; Chiquelho et al., 2011; Gjerset et al.,
2019; Pahlavanzade et al., 2014), and the remaining provided it
as one- to- one. The number of sessions ranged from 1– 10, and
the sessions lasted for 24– 120 min (the median was 45 min). The
interventions were conducted by nurses, trained intervention
providers or multidisciplinary teams. In two studies, the
inter-vention provider was not reported (Badr et al., 2016; Bahrami
and Farzi, 2014). The family member invited to participate was
identified by the person diagnosed with cancer. The inclusion
essentially involved persons providing significant support to the
person, so there was a variation in terminology: ‘partners’ (Budin
et al., 2008; Gjerset et al., 2019), ‘caregivers’ (Chambers et al.,
2014), ‘family caregiver’ (Bahrami & Farzi, 2014; Pahlavanzade
et al., 2014), ‘carers’ (Nga Fan et al., 2014) and ‘families and
friends’ (Carlsson & Strang, 1998; Chiquelho et al., 2011; Roberts
& Black, 2002).
Author, year, country Aim Design Participants Diagnosis
21. Kozachik et al. (2001), USA To determine the impact of a 16- week supportive nursing intervention on caregivers of patients with newly diagnosed cancer
RCT 125 dyads Multiple (breast, colon, lung, non-
Hodgkin's lymphoma, and pancreas) 22. Kuijer et al. (2004), NZ Explored to what extent a decrease in perceived equity after the intervention could
predict relationship quality and psychological distress directly after the intervention and 3 months later To explore to what extent a decrease in perceived equity after the intervention could predict relationship quality and psychological distress directly after the intervention and 3 months later
RCT 59 dyads Not Stated
23. Kurtz et al. (2005), USA To determine whether a clinical nursing intervention focusing on teaching caregivers and their cancer patients’ skills to better manage the symptoms would reduce caregiver depressive symptomatology
RCT 237 dyads Not Stated
24. Lewis et al. (2019), USA To test the short- term efficacy of a brief, fully manualised marital communication and interpersonal support intervention for couples facing recently diagnosed breast cancer
RCT 322 pairs Breast
25. Northouse et al. (2007), USA To determine whether a family- based intervention could improve appraisal variables (appraisal of illness or caregiving, uncertainty, hopelessness), coping resources (coping strategies, self- efficacy, communication), symptom distress, and quality of life in men with prostate cancer and their spouses
RCT 235 couples Prostate
26. Porter et al. (2009), USA To determine the efficacy of a novel partner- assisted emotional disclosure intervention in a sample of patients with gastrointestinal (GI) cancer
Quasi- experimental 130 couples Multiple (GI- cancers)
27. Porter et al. (2011), USA To determine the efficacy of a caregiver- assisted CST protocol in a sample of patients with
lung cancer RCT 233 dyads Lung
28. Roberts and Black (2002), Australia To report the results of an evaluation of an Australian education and support programme for individuals with cancer and their family and friends— the Living with Cancer Education Programme (LWCEP)
Quasi- experimental 576 family members and friends Not Stated
29. Schellekens et al. (2017), Netherlands he aim of this study was to examine the effectiveness of MBSR added to CAU compared to CAU alone to reduce psychological distress in patients with lung cancer and/or their partners he aim of this study was to examine the effectiveness of MBSR added to CAU compared to CAU alone to reduce psychological distress in patients with lung cancer and/or their partners
To examine the effectiveness of MBSR added to CAU compared to CAU alone in reducing psychological distress in patients with lung cancer and/or their partners
RCT 63 patients and 44 partners Lung
30. Sherwood et al. (2012), USA To determine, in patients with solid tumours, whether a nurse- delivered symptom management intervention was more effective than a coach- led intervention in increasing caregiver involvement in symptom management and improving caregivers’ emotional health
RCT 225 family caregivers Not Stated
31. Nga Fan et al. (2014), Hong Kong To evaluate the efficacy of the programme in reducing depression, anxiety, stress, and burden of care among carers of patients with colorectal cancer
RCT 140 carers Colorectal
32. Pahlavanzade et al. (2014), Iran To determine the effect of a family need- based programme on the burden of care in caregivers of leukaemia patients
RCT 70 caregivers Leukaemia
TA B L E 4
Support models
Author Intervention Sessions Mode By who/To whom Aim Conclusion
Psycoeducation Arnaert et al.
(2010)
The Skills for Healing Weekend Retreat included a package of interventions: (1) didactic sessions on how to negotiate the medical system, on the role of nutrition and complementary therapy, on stress and the relaxation response, and on spirituality in cancer care; (2) coping skills such as relaxation and yoga from the mindfulness- based stress reduction paradigm; and (3) supportive- expressive support group therapy, a series of lectures on healing and coping modalities, and frequent opportunities for participants to share their stories with others
Weekend Retreat An interdisciplinary approach,
including an oncologist, a specialist in mind– body medicine, a nurse, a social worker, and a spiritual care provider
Informal caregiver
Providing respite from the strains of caring for an individual, as well as skills to aid them in coping
The findings indicate that the retreat, in bringing people together to partake in discussions and activities, fostered a sense of community among the participants. The retreat also had enduring effects, contributing to relatives’ ongoing processes of healing as well as providing them with strategies for coping in their roles as caregivers
Badger et al. (2011) Interpersonal counselling intervention (TIP- C): a standard interpersonal psychotherapy combined with cancer education, targeting the social support behaviours of both cancer survivors and their partners. The intervention addressed (1) mood and affect management, (2) emotional expression, (3) interpersonal communication and relationships, (4) social support, and (5) cancer information.
An 8- week health education attention condition (HEAC). It included written material about cancer diagnosis and treatments and health- related topics such as nutrition during cancer, exercise to decrease fatigue, resources for cancer survivors, and resources for quitting smoking
TIP- C: An 8- week intervention for both patient and partner. During this same period, the partners received a session every other week (four sessions) to discuss the partner's own physical and emotional well- being. The average session length was 30 min each.
HEAC: Survivors received weekly telephone calls to review these materials. No counselling was offered. During this same period, the partners received telephone calls every other week for a total of four sessions. The average session was 30 min each
Telephone TIP- C: Trained interventionists (A master's- prepared nurse or social
worker
with psychiatric and oncology expertise)
HAEC: Research assistant Supportive intimate or family
partner
Maintaining and improving QoL (psychological, physical, social, and spiritual well- being)
The psychosocial interventions in this study were effective in maintaining or improving the QoL for prostate cancer survivors and their partners. Both the survivor and their intimate partner or family member benefitted from the interventions. Future research is needed to determine the optimal timing and client characteristics for each interventio
Badger et al. (2013)
The interventions were telephone health education (THE) and telephone or videophone interpersonal counselling (TC or VC). Participants received pamphlets about (1) breast cancer terminology, (2) treatments, (3) side effect management, (4) nutrition, (5) physical activity, and (6) resources. The TC and VC addressed (1) mood and affect management, (2) emotional
expression, (3) interpersonal communication and relationships with family and providers, (4) social support, and (5) follow- up, resources and referral to any support services that might be required (e.g. insurance and financial)
Participants received eight weekly sessions of health education, and their partners received four sessions every other week
Telephone Videophone
Trained interventionists Supportive partner
Improve QoL, social and spiritual well- being and reduce distression and depression
Survivors’ and partners’ social well- being improved in the TC and VC treatment groups, but not in the THE group. Telephone- delivered psychosocial interventions can be effective for managing QoL in breast cancer survivors and their supportive partners. There was no evidence of superior outcomes associated with using videophones over the conventional telephone
Badger et al. (2020)
Supportive health education (SHE) and TIP- C.
SHE: Standardised educational materials were sent to the participants prior to the initial session. SHE focused on (1) normal breast health and breast cancer, (2) routine tests and associated terminology, (3) treatment, side effects and strategies to combat side effects, (4) lifestyle interventions such as nutrition and physical activity, and (5) resources and referrals. TIP- C: see Badger et al. (2011, 2013)
TIP- C: One session a week for 8 weeks. The average session was 29 min.
SHE: One session a week for 8 weeks. Average time was 24 min/intervention
Telephone Trained interventionists Informal caregivers
Decrease symptoms of distress and social isolation. Increase symptom management, and social support.
The interventions improved different outcomes. TIP- C demonstrated superior benefits for depression management, and SHE was more successful in anxiety and cancer- related symptom management
Badr et al. (2016) CARES (Computer- Assisted oral cancer Rehabilitation and Support programme), grounded in Self- Determination Theory, which emphasises fulfilment of the fundamental psychological needs for competence, autonomy, and relatedness). CARES offered practical cancer- specific information and national healthy lifestyle guidelines/recommendations for cancer survivors. It also provided an opportunity to solicit and offer support to peers and each other through limited access, facilitated bulletin boards, and survivor– caregiver sharing function
Not applicable Web- based Not applicable
Primary caregiver
Enhancing autonomy, competence, and relatedness as well as improving QoL
This study demonstrates that OC survivors and caregivers are interested in using an online programme to improve QoL and that providing tailored website content and features based on the person's role as survivor or caregiver is important in this population
Bahrami and Farzi (2014)
Supportive educational programme, based on COPE model, which focuses on creativity, optimism, planning, and expert information on individuals
Two hospital visits (first visit 60 min, the following 30 min)
Two telephone sessions for 9 days
In person and telephone
–
Family caregiver
Improving QoL (cancer patients’ caregivers’ QoL and WHO QoL) and reducing family caregivers’ caring burden
It can be concluded that provision of support and education for family caregivers of women with breast cancer can reduce their caring burden and improve their quality of life
TA B L E 4
Support models
Author Intervention Sessions Mode By who/To whom Aim Conclusion
Psycoeducation Arnaert et al.
(2010)
The Skills for Healing Weekend Retreat included a package of interventions: (1) didactic sessions on how to negotiate the medical system, on the role of nutrition and complementary therapy, on stress and the relaxation response, and on spirituality in cancer care; (2) coping skills such as relaxation and yoga from the mindfulness- based stress reduction paradigm; and (3) supportive- expressive support group therapy, a series of lectures on healing and coping modalities, and frequent opportunities for participants to share their stories with others
Weekend Retreat An interdisciplinary approach,
including an oncologist, a specialist in mind– body medicine, a nurse, a social worker, and a spiritual care provider
Informal caregiver
Providing respite from the strains of caring for an individual, as well as skills to aid them in coping
The findings indicate that the retreat, in bringing people together to partake in discussions and activities, fostered a sense of community among the participants. The retreat also had enduring effects, contributing to relatives’ ongoing processes of healing as well as providing them with strategies for coping in their roles as caregivers
Badger et al. (2011) Interpersonal counselling intervention (TIP- C): a standard interpersonal psychotherapy combined with cancer education, targeting the social support behaviours of both cancer survivors and their partners. The intervention addressed (1) mood and affect management, (2) emotional expression, (3) interpersonal communication and relationships, (4) social support, and (5) cancer information.
An 8- week health education attention condition (HEAC). It included written material about cancer diagnosis and treatments and health- related topics such as nutrition during cancer, exercise to decrease fatigue, resources for cancer survivors, and resources for quitting smoking
TIP- C: An 8- week intervention for both patient and partner. During this same period, the partners received a session every other week (four sessions) to discuss the partner's own physical and emotional well- being. The average session length was 30 min each.
HEAC: Survivors received weekly telephone calls to review these materials. No counselling was offered. During this same period, the partners received telephone calls every other week for a total of four sessions. The average session was 30 min each
Telephone TIP- C: Trained interventionists (A master's- prepared nurse or social
worker
with psychiatric and oncology expertise)
HAEC: Research assistant Supportive intimate or family
partner
Maintaining and improving QoL (psychological, physical, social, and spiritual well- being)
The psychosocial interventions in this study were effective in maintaining or improving the QoL for prostate cancer survivors and their partners. Both the survivor and their intimate partner or family member benefitted from the interventions. Future research is needed to determine the optimal timing and client characteristics for each interventio
Badger et al. (2013)
The interventions were telephone health education (THE) and telephone or videophone interpersonal counselling (TC or VC). Participants received pamphlets about (1) breast cancer terminology, (2) treatments, (3) side effect management, (4) nutrition, (5) physical activity, and (6) resources. The TC and VC addressed (1) mood and affect management, (2) emotional
expression, (3) interpersonal communication and relationships with family and providers, (4) social support, and (5) follow- up, resources and referral to any support services that might be required (e.g. insurance and financial)
Participants received eight weekly sessions of health education, and their partners received four sessions every other week
Telephone Videophone
Trained interventionists Supportive partner
Improve QoL, social and spiritual well- being and reduce distression and depression
Survivors’ and partners’ social well- being improved in the TC and VC treatment groups, but not in the THE group. Telephone- delivered psychosocial interventions can be effective for managing QoL in breast cancer survivors and their supportive partners. There was no evidence of superior outcomes associated with using videophones over the conventional telephone
Badger et al. (2020)
Supportive health education (SHE) and TIP- C.
SHE: Standardised educational materials were sent to the participants prior to the initial session. SHE focused on (1) normal breast health and breast cancer, (2) routine tests and associated terminology, (3) treatment, side effects and strategies to combat side effects, (4) lifestyle interventions such as nutrition and physical activity, and (5) resources and referrals. TIP- C: see Badger et al. (2011, 2013)
TIP- C: One session a week for 8 weeks. The average session was 29 min.
SHE: One session a week for 8 weeks. Average time was 24 min/intervention
Telephone Trained interventionists Informal caregivers
Decrease symptoms of distress and social isolation. Increase symptom management, and social support.
The interventions improved different outcomes. TIP- C demonstrated superior benefits for depression management, and SHE was more successful in anxiety and cancer- related symptom management
Badr et al. (2016) CARES (Computer- Assisted oral cancer Rehabilitation and Support programme), grounded in Self- Determination Theory, which emphasises fulfilment of the fundamental psychological needs for competence, autonomy, and relatedness). CARES offered practical cancer- specific information and national healthy lifestyle guidelines/recommendations for cancer survivors. It also provided an opportunity to solicit and offer support to peers and each other through limited access, facilitated bulletin boards, and survivor– caregiver sharing function
Not applicable Web- based Not applicable
Primary caregiver
Enhancing autonomy, competence, and relatedness as well as improving QoL
This study demonstrates that OC survivors and caregivers are interested in using an online programme to improve QoL and that providing tailored website content and features based on the person's role as survivor or caregiver is important in this population
Bahrami and Farzi (2014)
Supportive educational programme, based on COPE model, which focuses on creativity, optimism, planning, and expert information on individuals
Two hospital visits (first visit 60 min, the following 30 min)
Two telephone sessions for 9 days
In person and telephone
–
Family caregiver
Improving QoL (cancer patients’ caregivers’ QoL and WHO QoL) and reducing family caregivers’ caring burden
It can be concluded that provision of support and education for family caregivers of women with breast cancer can reduce their caring burden and improve their quality of life
Author Intervention Sessions Mode By who/To whom Aim Conclusion Budin et al. (2008) Standardised psychoeducation (SE) or telephone counselling (TC) or both (SE
+TC)
Both SE and TC interventions were based on a theoretical framework. The content was organised under three broad topics: (1) health- relevant information, (2) information on skill development to facilitate effectiveness of coping, and (3) psychosocial support.
SE by video consisted of four phases: coping with your diagnosis, recovering from surgery, understanding adjuvant therapy, and your ongoing recovery.
TC: Separate scripts were tailor- made for patients and partners to address the unique phase- specific individual needs of patients and partners
Interventions at the following phases of the cancer treatment recovery trajectory: (1) baseline or upon entry into the study; (2) diagnostic phase, when the diagnosis of breast cancer was determined; (3) postsurgical phase, 2 days after surgery; (4) adjuvant therapy phase, when making decisions about adjuvant therapy after discussion with an oncologist; and (5) ongoing recovery phase, 2 weeks after completion of chemotherapy or radiation or 6 months after surgery if no adjuvant therapy was received. SE: Four phase- specific psychoeducation videos. TC: Four standardised phase- specific sessions for
each patient and partner
SE: Video TC: Telephone
Nurse Partner
TC objectives: to reduce anxiety, shape reality- based appraisals, facilitate coping and attainment of support, process
information, encourage adaptive behavioural change, promote functional communication, and promote reintegration of a holistic concept of self
TC group had poorer scores on physical symptoms
compared with the SE +TC group and poorer vocational scores compared with standard care
Carlsson and Strang (1998)
Educational and supportive group programme Seven sessions (1.5– 2 h) at different stages of disease Mixed supportive groups
– Next of kin Families
Improving mood No significant change
Chambers et al. (2014)
A nurse- led self- management intervention with feedback about patients’ levels of distress and stress reduction instructions. The session focused on eliciting concerns, ensuring access to relevant cancer information, offering brief psychoeducation, orienting participants to the psychological self- management strategies provided in the accompanying resource kit, and, where relevant, discussing specific strategies matched to participant need.
Psychoeducation about the psychological impact of cancer, coping and stress management skills, problem solving, cognitive therapy, and enhancing support networks. Participants were given assigned behavioural homework for each core component. Additional components for specific treatment effects were included where relevant (e.g. pain, sleep disturbance, fatigue)
First intervention: one Session Second intervention: five sessions
Both interventions: Telephone, resource kit with written information, and an audio instructional CD about relaxation exercises
First intervention: Nurse Second intervention: Psychologist Caregivers
Improvements in psychological health, including reduced psychological distress (anxiety and depression) and increased positive adjustment and coping skills
Many distressed patients with cancer and their caregivers may benefit significantly from a single session of a nurse psychoeducation intervention that can be delivered remotely by telephone and supported by self- management materials. Survivors and caregivers with low education and low literacy may require more in- depth and targeted support
Chien et al. (2020) Psychosocial information package (PIP) included a psychosocial information manual and telephone support for 6 weeks. Six- session psychosocial information manuals were provided. The manuals were mailed to the participants weekly. The receipt of the information was confirmed by telephone, and appointments were set for the telephone support period. The multimedia psychosocial intervention (MPI) included a weekly
psychosocial information film via the mobile messaging application, a psychosocial information manual, and professional support for 6 weeks
PIP: Six sessions for 6 weeks MPI: Six sessions 6 weeks
PIP: Manual and telephone information and
support MPI: Information
film via mobile plus support
Nurse Partners
Improving emotion status, relationship satisfaction, health- related quality of life (HRQOL)
Partners of patients in a PIP group reported significant improvement in positive and negative affect and mental HRQOL. Partners in the MPI group also reported significant improvement in the negative affect
Chiquelho et al. (2011)
proFamilies: a psychoeducational intervention for cancer patients and their families. Educational components: information on cancer and treatment, community resources, technical terms, and home precautions. Support components: normalising experience of cancer, improving emotion- management strategies, encouraging communication, developing stress management strategies, cognitive relaxation training, dealing with anxieties and fears, and recognising the importance of social support networks. Group members were encouraged to contact another group member or a friend during the week as a way of activating their social networks.
Six sessions, once a week for 6 weeks Multi- family
discussion group
Multidisciplinary Families
Creating cohesion and diminishing perceived stress
The programme responds to the patients’ and their families’ needs, and participation promotes an adequate level of family cohesion and diminishes the perceived stress
Gabriel et al. (2019)
Information about cancer and practical care, information relating to the management of common symptoms and dealing with the patient's emotions, adjustment to the role of caregiver, communication, dealing with the emotional aspect of caring, self- care
Six sessions, once a week for 6 weeks. Each session was 90 min in length
Face- to- face sessions
Nurse
Primary caregivers
Reducing caregiving burden and improving self- reported QOL
The psychosocial intervention programme had a positive effect on caregiver burden and QOL. Issues such as sustainability of such programmes and advocacy relating to caregiver burden need further research