MALMÖ UNIVERSIT Y HEAL TH AND SOCIET Y DOCT OR AL DISSERT A TION 20 1 1:5 MA GD ALEN A ANNERS TEN GERSHA TER MALMÖ UNIVERSIT MALMÖ UNIVERSITY
MAGDALENA
ANNERSTEN GERSHATER
PREVENTION OF FOOT
ULCERS IN PATIENTS wITH
DIABETES MELLITUS
Nursing in outpatient settings
isbn/issn 978-91-7104-412-9 / 1653-5383 PREVENTION OF FOO T UL CERS IN P A TIENT S w ITH DIABETES MELLITUS
P R E V E N T I O N O F F O O T U L C E R S I N P A T I E N T S W I T H D I A B E T E S M E L L I T U S
Malmö University
Health and Society Doctoral Dissertation 2011: 5
© Copyright Magdalena Annersten Gershater 2011 Cover: Heidi Grill Magnusson
Pictures 1-8 and 10-11 by courtesy of Jan Apelqvist Picture 9: Magdalena Annersten Gershater ISBN 978-91-7104-412-9
ISSN 1653-5383 Holmbergs, Malmö 2011
MAGDALENA
ANNERSTEN GERSHATER
PREVENTION OF FOOT ULCERS
IN PATIENTS WITH DIABETES
MELLITUS
Malmö University, 2011
Faculty of Health and Society
Nursing in outpatient settings
CONTENTS
ABSTRACT ... 11
ORIGINAL PAPERS I-Iv ... 13
DEFINITIONS ... 14
Healed ulcer ... 14
Multiple ulcers ... 14
Health care assistant ... 15
Home nursing ... 15
Participant driven education ... 15
INTRODUCTION ... 20
BACKGROUND ... 21
Diabetes Mellitus ... 21
Micro vascular complications ... 21
Macro vascular complications ... 22
Treatment ... 22
Foot ulcers in patients with diabetes ... 22
Neuropathy... 23
Peripheral arterial disease... 24
Treatment of foot ulcers ... 25
Health care organization ... 26
Hospitals ... 26
Primary health care centers ... 26
Home nursing organization ... 27
Registered nurses’ formal competence ... 28
Leadership ... 29
Nursing practice ... 29
Research and Development ... 32
Diabetes nursing ... 32
Prevention ... 33
Prevention of foot ulcers ... 34
PREvIOUS STUDIES ... 37
Factors related to ulceration and outcome ... 37
Nursing in home nursing setting ... 45
Prevention ... 45 Patient education ... 46 RATIONALE ... 48 AIM ... 49 Specific aims ... 49 METHODS ... 51 Study I ... 51 Design ... 51 Primary Outcome ... 51 Setting ... 51 Study population ... 51 Inclusion criteria ... 51 Procedure ... 52
Data management and analysis ... 52
Study II ... 54
Design ... 54
Setting ... 54
Inclusion criteria ... 54
Procedure ... 54
Data management and analysis ... 54
Study III ... 56 Design ... 56 Setting ... 56 Study population ... 56 Inclusion criteria ... 56 Procedure ... 56
Study Iv ... 57 Design ... 57 Setting ... 58 Study population ... 58 Inclusion criteria ... 58 Exclusion Criteria ... 58 Procedure ... 58
Data management and analysis ... 59
ETHICAL CONSIDERATIONS ... 61 RESULT ... 63 Study I ... 63 Demographic characteristics ... 63 Study II ... 69 Study III ... 70 Performing leadership ... 70 Performing education ... 71
Performing the nursing process ... 72
The registered nurses’ competence and professional development ... 74
Study Iv ... 74
Baseline ... 74
Follow up at six months ... 75
Intervention ... 75
METHODOLOGICAL CONSIDERATIONS ... 78
Identification of the research problem ... 78
Study design and procedure ... 79
Recruitment ... 79
Reliability ... 82
validity ... 83
Educational intervention ... 84
RESULT DISCUSSION ... 86
The fragile patient ... 86
The coordinating nurse ... 89
Organization and prevention ... 92
FURTHER RESEARCH ... 96 CONCLUSION ... 97 ACKNOwLEDGEMENTS ... 98 SAMMANFATTNING PÅ SvENSKA ... 101 REFERENCES ... 104 PAPERS 1 – 4 ... 123
ABSTRACT
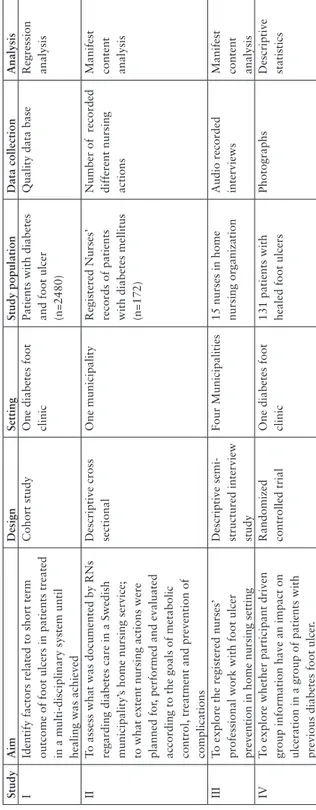
Amputation in patients with diabetes mellitus preceded by a foot ulcer is a serious complication. Patients with the highest risk of developing a foot ulcer are often found in home nursing settings. The overall aim was to focus on how registered nurses are working with prevention of foot ulcers in patients with diabetes mellitus in outpatient settings: - to identify factors related to short term outcome of foot ulcers in patients treated in a multi-disciplinary system until healing was achieved. - to assess what was documented by registered nurses regarding diabetes care in a Swedish municipality’s home nursing service; to what extent nursing actions were planned for, performed and evaluated according to the goals of metabolic control, treatment and prevention of complications.- to explore registered nurses’ professional work with foot ulcer prevention in home nursing settings. - to explore whether participant driven group information has an impact on ulceration in a patient group with previous diabetes foot ulcer. Study I used logistic regression analysis to identify factors related to outcome in a cohort of 2480 consecutive patients with diabetic foot ulcer at a multidisciplinary foot clinic. Results: Healed primarily: 65% (n=1617), 9% (n=250) after minor amputation, 8% (n=193) after major amputation and 17% (n=420) died unhealed. Primary healing was related to co- morbidity, duration of diabetes, extent of peripheral vascular disease and type of ulcer. In neuropathic ulcers, deep foot infection, site of ulcer and co-morbidity was related to amputation. In neuro-ischemic/ischemic ulcers amputation was related to co morbidity, peripheral arterial disease and type of ulcer.
Study II was a cross sectional assessment of all nursing records of patients with diabetes (n=172) in a municipality’s home nursing setting and analyzed with manifest content analysis. Results: The overall standard of nursing records was
insufficient. Evaluation of blood glucose was documented in 61% (n=105) of the records, weight was documented in 6% (n=10), blood pressure in 10% (n=17) and ongoing foot ulcers were documented in 21% (n=36).
Study III was a qualitative interview study of 15 registered nurses from four municipalities, analyzed with manifest content analysis. Results: Registered nurses in home nursing settings worked mainly through health care assistants. The nurses used leadership and education as the main tools to enable the nursing process. They mainly relied on experience based competence.
Study IV was a randomized controlled trial comparing participant driven education in group with standard information, in patients with diabetes and previous foot ulcers. An interim analysis was made 6 months after intervention of 131 included patients. Results: After 6 months follow up, 58% (n=57) of the 98 evaluated patients had not developed a new foot ulcer. There was no statistical difference between the two interventions. The most common reasons for ulceration were plantar stress ulcer and minor external trauma. Five patients had deceased and 13 had withdrawn consent to participate.
Conclusion: Patients with diabetes and high risk of developing foot ulcer constitute a fragile group that needs special foot protective attention. This requires a well educated staff in the home nursing organization and well educated registered nurses regarding leadership and pedagogy. In the future patient education should target low risk patients.
ORIGINAL PAPERS I-IV
This PhD thesis is based on the following papers which are referred to by Roman numerals:
I. Annersten Gershater, M., Löndahl, M., Nyberg, P., Larsson, J., Thörne, J., Eneroth, M. & Apelqvist, J. (2009) Complexity of factors related to outcome of neuropathic and neuroischemic/ischemic diabetic foot ulcers. A Cohort Study.
Diabetologia, 52(3):398-407
II. Gershater, M.A., Pilhammar, E. & Alm-Roijer, C. (2011) Documentation of diabetes care in home nursing service in a Swedish municipality: a cross sectio-nal study on nurses’ documentation. Scandinavian Joursectio-nal of Caring Sciences, 25(2):220-6
III. Annersten Gershater, M., Pilhammar, E. & Alm-Roijer, C. (2011) Prevention of foot ulcers in patients with diabetes in home nursing settings – an interview study among registered nurses. Scandinavian Journal of Caring Sciences (submitted)
IV. Annersten Gershater, M., Pilhammar, E., Apelqvist, J. & Alm-Roijer, C. (2011) Patient education for prevention of diabetic foot ulcers: Interim analysis of a randomized controlled trial due to morbidity and mortality of participants.
European diabetes Nursing (submitted)
DEFINITIONS
Healed ulcer
Healed ulcer was defined when epithelisation has occurred, as Wagner 0 (1). See
picture 1.
Foot Ulcer
Foot ulcer was defined as Wagner 1 or more at or below the ankle. See picture 2.
Deep ulcer
Deep ulcer was defined as Wagner 2. See picture 3.
Foot infection
Foot infection was defined as Wagner 3 or deep soft tissue infection with or without osteomyelitis: an open lesion fulfilling at least three of the following criteria: cellulitis, positive bacterial culture, radiological or scintigraphic evidence, and histological diagnosis (2). See picture 4.
Gangrene
Gangrene was defined as a continuous necrosis of the skin and underlying structures indicating irreversible damage that would be unlikely to heal without loss of some part of the extremity, Wagner grades 4–5. See pictures 5 and 6.
Multiple ulcers
Multiple ulcers was defined in study I and IV as three or more ulcers on the same foot. Patients with several concurrent lesions were represented by the ulcer with the worst outcome in study I. See picture 7.
Minor amputation
Minor amputation was defined as amputation of toe(s) or fore foot below the ankle. See picture 8.
Major amputation
Major amputation was defined as amputation above the ankle. See picture 9.
Health care assistant
Health care assistant was defined as assistive nursing personnel without university education in nursing, for example upper secondary school educated nursing assistants, students or uneducated substitutes.
Home nursing
Home nursing was defined as a setting outside the hospital in the patients’ home or in an assisted living facility where registered nurses are responsible.
Professional work
Professional work was defined as work according to national legislation on nursing profession.
Chiropody
Chiropody was defined as foot care by a person without higher education.
Podiatry
Podiatry was defined as foot care by a person with a university degree in podiatric medicine.
Participant driven education
Participant driven education was defined as a group session based on participants’ own perceived problems and questions.
Picture 1 Wagner 0
Picture 3 Wagner 2
Picture 4 Wagner 3
Picture 6 Wagner 5 Picture 7 Multiple ulcers Picture 8 Minor amputation
INTRODUCTION
This thesis has been written with a particularly vulnerable patient group in mind. Patients with diabetes mellitus who have suffered from an amputation, have an ongoing or healed foot ulcer, or who are at risk for development of a foot ulcer, all have both physical and psychosocial needs that registered nurses can meet in their professional work. Prevention of foot ulcers has been considered beneficial for patients’ quality of life (3), and competent nurses in a well functioning organization are facilitating factors for meeting these needs. Amputation of a leg in patients with diabetes mellitus is a severe and feared complication as about 40-70% of all non traumatic lower extremity amputations in the world are related to diabetes. The main reasons are gangrene and/or deep infection preceded by a foot ulcer (4). Patients at greatest risk of ulceration can easily be identified by careful clinical examination of the feet. International and national guidelines state the need of targeted education and frequent follow up for these patients (4-7) . Registered nurses around the world subscribe to International Council of Nurses’ code of ethics. The code states four fundamental work areas: promoting health, preventing disease, restoring health and alleviating suffering (8). By applying this code, registered nurses can contribute greatly to the work with prevention of foot ulcers. In Sweden’s health care organization prevention has been integrated into the formal description of registered nurses competencies, and according to Board of Health and Welfare the registered nurses have four areas to fulfil this work: leadership, nursing theory and praxis, education and research & development (9). However, there has not been described what registered nurses can do to compensate for patients unable to maintain their preventive self care of the feet. This thesis is an attempt to meet these knowledge gaps.
BACKGROUND
Diabetes Mellitus
Diabetes is a chronic disease that requires continuing medical care and patient self-management education to reduce the risk for acute and long term complications. The goal of self-management education is to enable the patients to take own responsibility for treatment and control of their disease by developing problem solving skills in the various aspects of diabetes management. Diabetes type 1 has its origin in destruction of pancreatic beta cells, leading to total insulin deficiency; diabetes type 2 on the other hand is described as relative insulin deficiency resulting from a progressive insulin secretion defect on the background of insulin resistance. Both conditions require lifelong pharmacological treatment with blood glucose lowering agents, and an adjusted life style comprising a well balanced diet and regular physical exercise (7, 10). In the European Union the average prevalence of diabetes mellitus between 20-79 years of age was 8,6% in 2006, representing over 31 million people across the 27 EU member states. It is expected that the number of patients with diabetes will increase drastically within the near future. As a result patients affected by its long term complications will also contribute to increasing demands on health care organizations (11). Long term complications affect different organs of the body, depending if the complications are of micro or macro vascular origin.
Micro vascular complications
One of the most feared long term complications of diabetes is retinopathy and blindness, and another severe complication is diabetic nephropathy. Both conditions are associated with long standing hyperglycemia, damaging the small blood vessels in the eye and kidney (12, 13). Diabetes is ranked among the leading causes of blindness and diabetes renal failure is the single leading cause of end stage renal disease. For example: in the United States more than
45% of new cases of patients requiring renal replacement therapy have diabetes (11, 14). Neuropathy as a micro vascular complication will be discussed later in connection with the diabetic foot ulcer.
Macro vascular complications
The major cause of mortality and morbidity for individuals with diabetes is cardiovascular disease (coronary heart disease, ischemic stroke and peripheral arterial disease with ischemic feet), based on atherosclerosis in the major blood vessels. The background mechanisms are to be sought in common risk factors such as hypertension, obesity, physical inactivity, elevated blood lipids and smoking (15, 16). About 75-80% of patients with diabetes, die of cardiovascular events, which is the number one cause of death in Europe for both men and women. Patients with type 2 diabetes have a 2-4 times higher risk of coronary heart disease than the rest of the population (11, 14). Peripheral arterial disease in combination with infection is an important factor for amputation, and mortality in this patients group is high (17-20).
Treatment
The main goal in the treatment of diabetes is to reduce the progression of micro and macro vascular complications. There is evidence that good control of blood glucose levels can substantially reduce the risk and inhibit the progression of complications in all types of diabetes (7, 12, 15). Management of high blood pressure and of raised blood lipids is equally beneficial for the patients, as well as physical activity, reduction of stress, and a smoking free lifestyle (10). The goals are believed to be reached by a physically active life style, intake of calories not exceeding expenditures, low intake of saturated fat, smoking cessation, prescription of pharmacological drugs, screening for early detection of signs of complications, and an extensive patient education program to enable the patients to take their own responsibility for treatment and control (7, 10).
Foot ulcers in patients with diabetes
One severe complication of diabetes is amputation, which is preceded by a foot ulcer. It is believed that every 30 seconds a lower limb is lost somewhere in the world as a consequence of diabetes (21). The point prevalence of foot ulcers varies between 1,5-10% in different populations; a corresponding incidence of 2,2-5,9% (4). Previous studies have revealed substantial costs for society, particularly after amputation. The most expensive share in the care of diabetic foot ulcers is the cost of institutional living that becomes necessary after losing a limb, as many patients will not be able to walk again with prosthesis due to severe co-morbidity (3).
The foot ulcer has severe consequences for patients, family, health care system and society, and many patients with foot ulcers become dependent on home nursing services. Mortality in this patient group is high especially for patients with critical ischemia (4, 5, 20-23). The most common death causes reported for these patients are cardiac diseases and cerebrovascular disease (17), and it has also been reported that peripheral arterial disease is associated with an 67% increased risk of cardiac death (24). Common direct causes of ulceration are minor trauma from ill fitting shoes, plantar stress ulcer when prominent bone press the skin from inside in absence of fat padding, or walking bare foot on a sharp item (4, 5, 25, 26). Initially a very small ulcer may not be detected for several weeks. The patient eventually is convinced that it has appeared from nowhere, having forgotten the trauma which caused it. The main background mechanisms of development of foot ulcers are neuropathy with reduced sensation muscle wasting, foot deformity and peripheral arterial disease, both conditions may develop after long diabetes duration.
Neuropathy
The most important background causes of diabetic foot ulcers are sensory, motor and autonomic neuropathies together with peripheral arterial disease. The typical polyneuropathy is chronic and symmetrical, and is developed with a background of long-standing hyperglycaemia and cardiovascular risk factors (27). Sensory neuropathy is associated with loss of pain. Motor neuropathy lead to atrophy of plantar fat padding and muscles, resulting in flexion deformity of the toes and abnormal walking pattern. Autonomic neuropathy results in reduced or absent sweat secretion leading to dry skin with cracks and fissures, and atherio-venous shunting causing a red and swollen foot (4). Regular examination of the feet in all patients with diabetes mellitus is essential to detect early signs of neuropathy and other risk factors. It can be diagnosed using vibratory pressure threshold measured by a Biothesiometer (BioMedical Instruments, New Burry, OH, USA), Monofilament (28) or Ipswich touch test (29). There is no cure for neuropathy, but metabolic control is related to progress and development of sensorimotor neuropathy (27). See picture 10.
Picture 10: Neuropathic foot.
Peripheral arterial disease
Peripheral arterial disease (PAD) is caused by arteriosclerosis in the major arterial blood vessels, and is associated with high risk for amputation, cardiovascular co-morbidity and high mortality. This indicates a severe health status of the patients and has huge impact of patients’ quality of life (19, 23, 30-32). Contributing factors are hypertension, obesity, physical inactivity, elevated blood lipids and smoking. Treatments to improve peripheral arterial blood circulation are cessation of smoking, reduction of blood pressure and weight, low intake of saturated fat, increased physical activity, pharmacological treatment of lipids, anti coagulant drugs, and vascular surgery (17, 18). In a European multicentre study, about 50% of all patients at first visit to a diabetes foot clinic presented signs of peripheral arterial disease (19). See picture 11.
Picture 11: Ischemic foot
Treatment of foot ulcers
In 1985 one of the five-year targets of the European Declaration of St Vincent was a 50% reduction in amputation caused by diabetes mellitus (33). To shorten ulcer duration and to reduce the number of amputations, multiple treatment strategies depending on type, site and cause of ulcer can be used. Infections are intensively treated by using antibiotics and surgical revisions of the ulcers. If needed, metabolic control can be improved by initiating treatment with insulin. Oedema is treated according to its predisposing cause, and vascular surgery may improve blood circulation in the ischemic foot. The affected limb can be off loaded with a total contact cast, wheel chair or other technical equipment, as well as individually adjusted shoe wear. Local wound treatment is performed with regular debridement and dressing changes. Pain relief is obtained by treating its background causes. Regular podiatry or chiropody should also be offered the patients to prevent further ulceration. This requires a close collaboration between many different professionals working in a multi disciplinary team (4).
Health care organization
Patients with diabetes and complications are frequent visitors to the different settings that constitute the health care organization. The patient with diabetes and a foot ulcer has contact with different levels of health care providers: hospitals, health care centers and home nursing organizations.
Figure 1. Health care for patients with diabetes and foot ulcers.
Hospitals
The main hospitals in Sweden are managed by the county councils (34), and all have ambulatories for adult patients with type 1 and difficult type 2 diabetes. The health care professionals work in multi disciplinary teams that can consist of physicians with specialization in internal medicine and/or other sub specialties, registered nurses with education in diabetes nursing, physiotherapists, dieticians, nursing assistants, social workers, secretaries and chiropodists. For patients with complications, there is extensive consultant collaboration with other specialties, for example renal, ophthalmology and orthopedic surgery (7, 35). It is the registered nurse who coordinates the activities in the team (36, 37). In 2004 there were 43 multi disciplinary teams defining themselves as diabetic foot teams in Swedish hospitals, which manage the patients’ feet until healing is achieved (38).
Primary health care centers
Primary health care centers are managed by the county councils, and constitute the back bone in Swedish primary care (34).The centers are of different size, and responsible for a defined population within its geographical catchment area or for a certain number of listed patients. In the health care centers general practitioners (with specialization in family medicine), as well as district nurses, with a postgraduate diploma in specialist nursing (Public health 75 credits), work
Health Care Centre
Hospital
Home Nursing Service
together with other health care professions, depending on local circumstances. Some of the registered nurses also have an exam in diabetes nursing, 15 or 30 credits (35, 39, 40).
Diabetes care in hospitals and primary care centers is based on regional guidelines determined by local county councils. Regional guidelines are based on Swedish national guidelines, and the quality is systematically followed up with the aid of the national diabetes register (7, 41, 42). The patients visit the diabetes responsible physician at least once a year, and the diabetes responsible registered nurse more often, according to individual and organizational circumstances (35, 40). However, in a survey from 2008, 30% of the interviewed patients (n=199) with type 2 diabetes stated that they had never discussed complications of diabetes with their health care provider, and 36% never had visited a diabetes responsible nurse (42).
Home nursing organization
Home care can be described as care provided by professionals to patients in their own homes with the ultimate goal of contributing to their life quality and functional health status, and when needed also to replace hospital care with care in the home for societal reasons. Home care therefore covers a wide range of activities, from preventive visits to terminal care (43). In this thesis home care refers to all professional social activities performed in the patients’ home, while
home nursing service refers exclusively to the health care provided under the
auspices of the registered nurses. Patients in home nursing service (in their own home or in assisted living facilities) have become dependent on others taking care of their self care due to aging and several concomitant health conditions; such as cognitive disorders, impaired vision and impaired mobility (44). With a patient’s deteriorated health status, a burden of care is put on the next of kin. Municipality’s home care and home nursing service can provide professional nursing and social care when the family members are no longer able to meet this burden (45). Depending on local political and financial frames home nursing service differ in its organization nationally and internationally (46-52). In Sweden it is an integrated part of the extensive primary care organization, mainly organized by the municipalities under a medically responsible nurse, but in some counties organized by the county council in collaboration with the municipalities’ social service (53). Patients eligible for home nursing services are assessed for social and nursing needs, and an individual care plan is created due to re-imbursement rules (34, 52, 54). The organization uses registered nurses as the highest medical
competence with physicians employed by the county council available daytime at the health care centers. In the region where the present studies took place, one ambulant physician was available during evenings and nights (55). There is a formal specialization in geriatric nursing, but very few registered nurses working in home nursing organization have this specialization. It is more common that they are district nurses or have no specialization at all (56, 57). Registered nurses in home nursing service work under two legislations: The Health and Medical Service Act (34), and The Act of Social Service (54). The registered nurses are responsible for the nursing process, while health care assistants, beside their duties of providing social service, perform many of the nursing tasks. Health care assistants often have a 3 year secondary school education consisting of social work and health promotion, but due to shortage of staff, in many municipalities a mix of educational background is common (58). A written delegation from the registered nurse is made after some training in accordance with legislated patient safety (54, 59). The registered nurses can for example delegate administration of pre packed tablets (ApoDos®) and insulin injections, plasma glucose monitoring, and changing of ulcer dressings.
Patients with ongoing foot ulcers need regular wound management in between visits to the foot clinic. Those who are not able to perform visits to a registered nurse at the health care centre for dressing changes, have them changed at home by a registered nurse from the municipalities’ home nursing service or by a health care assistant under his/her supervision. The foot clinics provide the patients with written prescriptions about the dressings, off loading strategies, and changes in medication. Time to healing is often long; this implicates long term relationships between patients and registered nurses. If one foot is ulcerated, the other foot might be at high risk for ulceration, as the same risk factors probably are present, and the registered nurse visiting the patient has an opportunity to assess for risk factors in the home environment. The registered nurse in home nursing service also coordinates and implements treatment strategies of other co-morbidities, pain management, oedema, nutrition and off loading, and integrates these efforts into the patient’s life at home.
Registered nurses’ formal competence
According to the International Council of Nurses, registered nurses should promote health, prevent disease and help patients cope with illness (8). In many countries in Europe, the United States, and other parts of the world, legal descriptions of nurses’ professional competence illustrate these duties in different wording. They all have in common that nurses should focus on leadership, nursing
practice according to nursing theory, participate in research and development of their work and education of patients, next of kin and health care professionals
(9, 60-64). In Sweden and in many other countries, registered nurses have a three year bachelor degree in nursing as a legal pre requisite for the profession (9). The Swedish description of registered nurses’ competence is built up on recommendations of professional knowledge (technical, theoretical, and general knowledge), competence (skills based on experience, understanding, and judgment), and attitudes (engagement, courage, and responsibility), and of practical skills (9). The registered nurses should apply evidence based care that can be found in research, in national guidelines, compilations of scientific studies and accepted empirical research or local in local guidelines. They can also make decisions based on experience based knowledge and share decisions through patient participation.
Leadership
In Sweden the work around the patient is often organised in teams, which are led by the registered nurse. It is the registered nurses’ formal duty to lead and coordinate the work, depending on the patients’ needs, and to prioritize according to available resources. It is also the registered nurses’ duty to evaluate the work and to motivate other health care professionals in the team to work patient oriented and evidence based. This teamwork requires a good documentation and a quality assurance system due to the complexity of care. When different professions come together in teams, it is particularly important that the holistic nursing perspective is reflected in the professional nurse’s work, and that the registered nurses have achieved skills in reflection and critical thinking (9). Participation in quality and safety work, as well as organizational planning and follow up of the local health service are also important tasks for registered nurses (9, 62-64).
Nursing practice
The formal description of registered nurses’ competence states that they should apply the nursing process independently. This requires observation and assessment of the patients’ basal and specific nursing needs, determine nursing diagnose(s) and prescribe relevant actions to be taken, plan and perform the actions, and evaluate the effect on the patients. Changes in the patients’ physical or psychological condition should be observed, documented, and accordingly acted upon (9). To enable this, it is necessary that the work is documented according to legal requirements and that registered nurses critically assess their own documentation for quality improvement (65). By working through
the nursing process, they will be able to promote health and prevent illness: to identify and actively prevent health risks and when needed, motivate to a healthier life style. In settings outside of hospitals and health care centres, direct nursing actions are often delegated to health care assistants (59).
Nursing actions are preferably based on scientific evidence, nurses’ professional experience and patients’ expectations. However, these implementations are not frequently done in all health care settings, and in many areas the registered nurses need to develop working methods according to evidence based research, or even contribute to the research body that today is incomplete (66).
For patients with a complex disease such as diabetes mellitus, the registered nurses’ work can be facilitated by national guidelines of diabetes and local care programs (7, 67). They can also use nursing theories to support the patients’ ability to self care. In nursing practice for patients with diabetes, psychological skills and educational models have been used to structure their work; such as the
Health Belief Model or Orem’s Theory of Self Care (68, 69). Registered nurses
have also been involved in assessing the effects of pharmacological treatments such as measuring Hba1c, p-glucose profiles, blood pressure and blood lipids, as well as in the assessment of risk factors for complications of diabetes such as foot inspections, Body Mass Index, and smoking status (35, 41, 70).
This requires a documentation and communication system enabling the registered nurses to obtain knowledge about the patients’ status, nursing interventions, and evaluations. When the registered nurses have extensive districts with many patients with complex diseases, the follow up of the health care assistants’ work and its documentation is essential also for the physicians to provide adequate care (71-73).
Education
One important nursing action is education to patients, next of kin and other health care professionals. Depending on content and timing, it can be presented as information or education, and provided in group or personal settings (74).
Patient education
In order to provide the best possible education and support, it is essential that the registered nurses are able to assess the patients’ self care capacity and previous knowledge to individualize the education, and afterwards evaluate if the patient (or next of kin, or health care assistant) has understood the information.
According to the formal description of registered nurses’ competence, the nurses should have the skill to communicate respectfully and empathically in dialogue. Patients unable to communicate, or who have particular information needs, should be acknowledged, and subsequently adjusted action should be taken (9). Education for health promotion begins with identifying and assessing patients’ resources and skills for self care. Friberg (75) states that pedagogical responsibil-ity requires pedagogical knowledge to sharpen critical reflection. Every unique pedagogical situation can lead to an opportunity for the learning patient to ex-press his/her personal needs for knowledge. Based on holistic thinking, education should be based on the patient’s life and his/her experiences, which contributes to a complex and challenging learning situation. Education can never be a routine; neither can it consist of a set of pre set pedagogical methods, as not all patients have the same needs of knowledge based on having the same diagnoses.
Patient education methods
Traditionally patient education has aimed for a change in patients’ behavior in a situation where the teaching person acts to induce a desirable behavior, through punishment or rewards. Common methods used have been information,
cognitive behavioral theory, and health belief model as described by Friberg
in Pilhammar et al. (75) and Ogden (68). Subsequently, according to several guidelines, the objective of foot ulcer preventive education has been to change the self-care behaviour of the person with diabetes and to enhance adherence to foot care advice (4, 6, 76, 77). The mentioned guidelines and education programmes are normative in its appearance; it is stated that patients with diabetes should learn to recognize potential foot problems and take appropriate action. It has not been described in the guidelines how this is to be realized. However, they all have in common that foot ulcer preventive education should cover these themes:
motivation, methods of self care, seeking help early and social consequences. The
American Diabetes Association emphasizes the importance of assessing both the patient’s knowledge of aetiology of foot ulcers and ability to perform self care, before education (77). The International Consensus group recommends education to be simple, relevant, consistent and repeated, and that it should optimally be an integral part of each diabetes related encounter between patient and care giver. They state further that lecture style education sessions on foot care have shown to improve patients’ knowledge, but have little effect on actual self care of the feet. Programs aimed at increasing motivation and skills, in which education is provided in several sessions over a period of time, seems more promising, but no studies have proved effective (4). An educational program for leprosy
patients (78), a patient group with similar risk of developing foot ulcers, has a more patient oriented focus and subsequently could also be used in education of patients with diabetes and neuropathy.
The preferred method in the Swedish national legal description of registered nurses’ competence is to use dialogue to motivate the patients (9). The purpose of registered nurses’ education of patients is to enable optimum participation in the protection of the feet. It is important to enhance patients’ own motivation and skill based on his/her life situation and experiences. According to previous studies, problem based learning has shown effect on patients’ health behaviour in chronic diseases, but it needs to be evaluated further in diabetes care (79, 80).
Research and Development
A pre requisite for all patients to receive safe and effective care is that health care professionals use methods based on scientific evidence. The professional development of the registered nurse requires skills to independently analyze strengths and weaknesses of their own professional competence, and to continuously engage in personal and professional development. This can be realized through seeking, analysing and critically assessing relevant literature. By implementing this new knowledge, from organization and economy to patients’ individual situation, they can contribute to nursing practice according to science and experience (9). During the last decades studies in evidence based nursing have increased in number, however its implementation in clinical praxis has been delayed due to organizational barriers such as lack of time and lack of autonomy to change praxis (81). In the field of prevention of diabetic foot ulcers, evidence is meagre (82) and more studies are urgently needed for improved care.
Diabetes nursing
Focus for diabetes nursing in Sweden has been on patient education at the debut of the disease, providing support for behavioural change into a healthier life style with healthy eating, physical exercise, weight loss and smoking cessation. Technical self care skills such as performing insulin injections and self monitoring of plasma glucose have also been important. The goal has been to enable the patient to take responsibility for his/her disease and the treatment (7, 35, 40). Evaluation of effects of diabetes treatments can be done in national diabetes registers, measuring parameters such as BMI, Hba1c, blood pressure, and blood lipids. There is also recorded physical activity and existing severe foot disease, but not education (41).
PREVENTION
Registered nurses’ work with prevention of disease in general and prevention in diabetes in particular can take place at different levels and in different settings, depending on the purpose of the actual intervention. Registered nurses are expected to have the skills to identify and actively prevent risk factors, and when needed motivate the individual for changed life style, using education and support as means to promote health. The registered nurse should also actively prevent complications of diseases, or of treatments (9).
Primary prevention strategies intend to avoid the development of injury or disease. In a United Nations’ resolution the member states were encouraged to develop national policies for the prevention, treatment and care of diabetes (83, 84). It is however difficult to measure effects of primary prevention in conditions that are of multi factorial origin; but in a society where choices can be based on a clear understanding of the relevant issues, politicians have the responsibility to provide these conditions (85). Subsequently, in 2009 in the European Union, 13 out of 27 member states had developed a national plan or policy framework for the prevention and treatment of diabetes (11).
Secondary prevention strategies attempt to diagnose and treat an existing disease in its early stages before it results in significant morbidity. For patients with diabetes the prevention of complications in general takes place in the primary care organization for patients with type 2 diabetes and at the hospitals’ specialist clinics for patients with diabetes type 1, according to the Swedish National Guidelines (7). Risk factors that can be treated to prevent long term complications are hypertension, elevated blood lipids, hyperglycaemia, smoking and lack of
physical exercise (16, 80). Physical inactivity, coronary heart disease and renal
impairment are factors that contribute to oedema in the lower extremities, with ill fitting shoes and decreased elasticity of the skin as risk consequences. Impaired
vision increases the risk of external trauma to the feet. Many patients are elderly
and with the above mentioned concomitant conditions, therefore the preventive initiative of registered nurses both in hospitals, health care centres and in home nursing organization is vital. The registered nurses can provide education and coordinate other nursing actions for a reduction of risk factors, as well as facilitate enhancement of a good quality of life for the patients (7, 40).
Tertiary prevention goals are to reduce the negative impact of established disease by restoring function and reducing disease-related complications. Patients with diabetes who have established late complications such as blindness, end stage renal disease, cardiovascular disease, ongoing foot ulcers, amputation, and patients who have dementia or are in terminal care, are often taken care of by a municipality’s home nursing organization. Patients can continue living in their own homes, or when needed, moved into assisted living facilities. In both cases they can receive social service, help with medicine administration, dressing changes and sometimes specific nursing activities such as peritoneal dialysis and tube feeding (54, 71, 86). With impaired mobility that many home nursing patients suffer from, comes the necessity for prevention of pressure ulcers on the heels (and other parts of the body), with different techniques and methods of off loading, and providing this is a frequent working task for registered nurses (87, 88).
Prevention of foot ulcers
Five key interventions have been identified to prevent the development of foot ulcers in patients with diabetes mellitus: identification of foot at risk, regular
inspection of the feet, appropriate shoe wear, regular treatment by chiropodist or podiatrist, and education of health care providers and patients (4). Referral
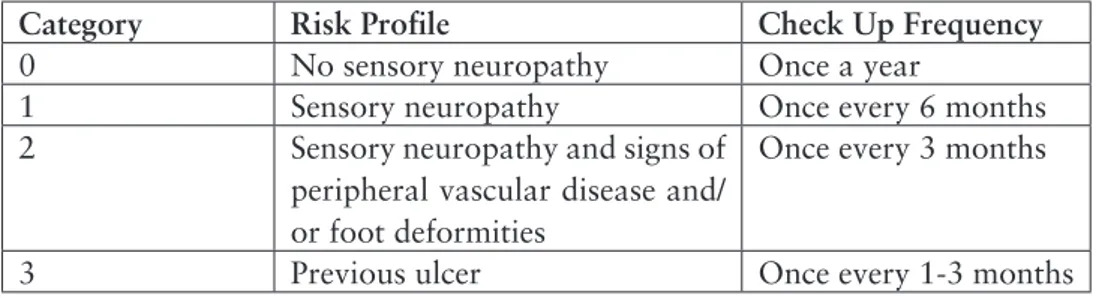
to multidisciplinary foot team for a patient with an ulcerated foot has been identified as the most important intervention to prevent amputation (4, 89). Risk factors for ulceration have been identified as previous foot ulcer, previous amputation, calluses and foot deformities, impaired protective sensation, and absent pedal pulses. After assessment of the feet, the patients can be categorized according to risk (4, 41). See table 1.
Regular inspection of the feet should ideally take place at each encounter between patient and a health care provider, being for example the regular diabetes responsible physician or registered nurse. In addition, the patient is recommended to inspect his/her feet daily to identify early signs of abnormality and the patient is recommended to use a mirror to help with the inspection of the plantar foot (4, 6, 7). If the patient is not able to perform this inspection, next of kin or home nursing service can provide support (7).
Since foot deformity is common among patients with diabetes and neuropathy, it is important that there is sufficient space for the toes in shoes. The insoles
in the shoes should also optimum reduce foot pressures below the threshold of ulceration. This requires shoes provided by orthopaedic specialist clinic and the patients need shoes for both indoor and outdoor use (80, 90). If foot wear cannot prevent recurrent ulceration, the patients’ activity level must be drastically modified (4). How this reduction of activity can be realized, has not been described in the guidelines.
It has been suggested that regular chiropody and education, provided individually by a chiropodist or podiatrist, result in improvements in knowledge, foot self-care and the prevalence of severe calluses and nail pathologies (91-93). Long term studies of the effect are missing, but in spite of this, it is believed that podiatry is beneficial for the patients (4). Regular chiropody visits contribute to a careful visual inspection of the feet, supporting patients with difficulties in performing self inspection and self care.
Education to patients and next of kin in preventive foot care, for those who have been identified as risk patients, has been described as important in several guidelines (4, 6, 76, 77). The goals of this education should optimum aim at of understanding the link between diabetes, neuropathy, and development of foot ulcer; the importance of daily inspections; practical self care actions; choice of appropriate shoe wear and the importance of seeking help early in case of any abnormality. In Sweden it is the registered nurses who have the professional responsibility to provide patient education, but sometimes also physicians and chiropodists provide the patients with information. A study by Annersten et al showed that 4% of 486 registered nurses in diabetes care working with patient education mentioned foot care as a goal for patients to achieve (35). It can therefore be assumed that foot care preventive education can be improved further in Swedish health care settings.
Once an ulcer has developed, the prevention is targeting healing without amputation. During ulceration the patients are best taken care of at specialized multidisciplinary foot clinics in close collaboration with the primary care organization or home nursing organization, when needed (89). The registered nurses at the foot clinics have a vast coordinating mission as many representatives from different specialities are working together, in and out of the hospital, and contact with home nursing organization is frequent (36).
Table 1. Risk categorization system according to International Guidelines on the Diabetic foot (4)
Category Risk Profile Check Up Frequency
0 No sensory neuropathy Once a year
1 Sensory neuropathy Once every 6 months
2 Sensory neuropathy and signs of
peripheral vascular disease and/ or foot deformities
Once every 3 months
3 Previous ulcer Once every 1-3 months
PREVIOUS STUDIES
There are a limited number of studies regarding prevention of foot ulcers in patients with diabetes mellitus and its outcome. PubMed and CINAHL were searched with support from a librarian using the Medical Subheading (MeSH) terms: [Diabetes Mellitus], [Diabetic foot ulcer], [Outcome], [Home Care], [Documentation], [Nursing]. The MeSH terms were used alone and combined. Reference lists and abstract books from the Diabetic Foot Conference in Noordwijkerhout, the Netherlands, 2003 and 2007 were also scrutinized for studies presenting data on outcome of foot ulcers in patients with diabetes (95, 96).
Factors related to ulceration and outcome
Outcome of foot ulcers can be presented as number of patients with primary healing without amputation, amputation of toe(s) or forefoot (minor amputation), amputation of leg below or above knee (major amputation) or as death before healing. Outcome of foot ulcers in patients with diabetes has been difficult to study due to differences in health care organizations around the world, with different competencies of health care professionals, different numbers of patients with many centres seeing few patients, and due to reimbursement systems that makes systematic follow up cumbersome or impossible. Different study design, selection of included patients, follow up time, and different outcomes have been used. Comparison between studies of outcome of foot ulcers therefore has been difficult.
Table 2 shows studies of cohorts with more than 100 included individuals of diabetes foot ulcers with a follow up time of maximum 12 months. The studies included between 146 and 1229 patients, with a variety of inclusion criteria and settings: from single centre assessing all new foot ulcers (97) to multicentre
studies excluding those with worst health status (19), and meta analysis of data from randomized controlled trials of topical treatment products (98, 99). Factors related to outcome in these disparate treatment systems, have been evaluated with different methodology and statistical methods and therefore numbers of patients with different outcome (primary healed, minor and major amputation and deceased before healing) cannot be compared between the studies. Data regarding number of ongoing ulcers at the time of study end is not presented here, as these patients have not yet reached the outcome. It seems though that age; ischemia and severity of ulcer have an impact on increased risk for amputation. See table 2.
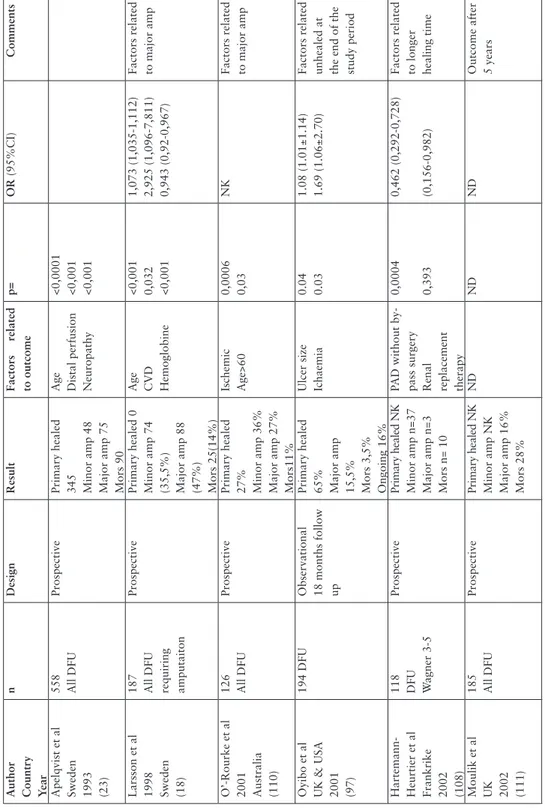
Table 3 describes studies of cohorts of patients with more than 100 included individuals on outcome of diabetes foot ulcers with a follow up time of more than 12 months. The studies included 126-706 patients, and the selection seem to be targeting patients with more severe health status than in the studies with shorter follow up time: patients with diagnosed ischemia (107), deep ulcers (108), inpatients with infections (109), and patients requiring amputation (18). Subsequently, factors related to outcome are more patient related than ulcer related: Age, cardio vascular disease, ischemia, end stage renal disease, and Hba1c, blood lipids, Haemoglobin, White Blood Cells and sCReactive Proteine (CRP) outside normal ranges indicate that patients affected by general poor health status have increased risk for amputation. See table 3, pages 39 and 40.
Author Country Year
n
Design
Result
Factors related to outcome
p=
OR (95%CI)
Comments
Margolis et al USA 1999 (98)
622 DFU
Review of control group patients from RCT
s
Primary healed 30,9% Age (years) Wound size (cm2) Wound duration (weeks)
NK
1,13 (0,69-1,84) 0,93 (0,82-1,04) 0,98(0,98-1,01)
Oyibo et al UK/USA 2001 (97)
194 New DFU
Prospective
Primary healed 65% Minor +Major amp 15,5% Mors 3,5% Ulcer size 3,9 vs 1,2 cm2 <0,0001 ND Beckert et al 2006 Germany (100) 1000 All DFU Prospective
Primary healing NK Minor amputation 99 (9,9%) Major amputation 26 (2,6%) Mors NK Multiple ulcers Probing to bone Location Non-palpable pulse
0,0001 0,025 0,0001 0,0001
0,648 (0,540- 0,778) 0,777 (0,623- 0,968) 0,483 (0,4,2- 0,580) 0,723 (0,603- 0,868) Factors related to amputation
Marston USA 2007 (99)
245 Neuropatic DFU 1-20 cm2 RCT human dermal dressing vs saline gauze Primary healed: Intervention 30% Control: 18% Intervention group healed faster than control group
0,04
ND
Drop out at 12weeks: 19%
Pound & Chipchase UK 2005 (101) 320 New DFU
Prospective
Primary healed 135 Amputated 12 Mors 51 Intact arterial blood supply vs not intact
<0,0001
ND
Factors related to amputation. Lost to follow up: 4,9%
T
reece et al UK 2004 (102)
300 DFU
Prospective
Primary healed 209 (69,7%) MajorAmp 8 (2,7%) Minor amp 22 (7,3%) Mors 32 (10,7%) Ulcer area Ulcer depth Arteriopathy
<0,0001 <0,0001 <0,0001
ND
Prompers et al Europe 2006 (103) 1229 DFU with expected survival >12 months
Prospective
Primary healed 77% Minor amp 13% Major amp 5% Mors 6% Age Ulcer size Inability to walk ESRD PA
D
0,001 <0,001 0,003 0,002 0,001
1,28 (1,11-1,47) 3,88 (2,37-6,34) 2,00 (1,27-3,14) 2,51 (1,41-4,48) 1,71 (1,23-2,37) Factors related to amputation. Drop out: n=144
Jeffcoate et al 2006 UK (104)
449 All DFU
Prospective
Primary healed 65,7% Amputation 8% Mors 10,9%
ND
ND
ND
Lost to follow up: 3,8%
Shojaiefard Iran 2008 (105)
146 All DFU
Prospective
Primary healed 71,2% Minor amp 22,6% Major amp 5,5% Mors 1,3% Hyperglycaemia Ischemia Nephropathy
0,0109 0,0101 0,0345
3,01 (1,32-6,83) 3,03 (1,28-7,18) 2,64 (1,6-6,60) Factors related to amputation
Richard et al France 2010 (106) 304 DFU inpatient with infected wound
Prospective
Primary healed 33% Minor amp 33% Major amp 8% Mors 8% Multiple toes involved Deep ulcer Osteomyelitis
NK
NK
Outcome after 12 months Drop out: n=13
DFU = Diabetes foot ulcer DM = Diabetes Mellitus NK Not known ND Not Done ESRD = End Stage Renal Disease
T
able 2. Overview of studies assessing outcome of foot ulcers
≤ 12 months.
T
T
able 2. Overview of studies assessing outcome of foot ulcers
≤
12 months.
Author Country Year
n
Design
Result
Factors related to outcome
p= OR (95%CI) Comments T reece et al UK 2004 (102) 300 DFU Prospective
Primary healed 209 (69,7%) MajorAmp 8 (2,7%) Minor amp 22 (7,3%) Mors 32 (10,7%) Ulcer area Ulcer depth Arteriopathy
<0,0001 <0,0001 <0,0001
ND
Prompers et al Europe 2006 (103) 1229 DFU with expected survival >12 months
Prospective
Primary healed 77% Minor amp 13% Major amp 5% Mors 6% Age Ulcer size Inability to walk ESRD PA
D
0,001 <0,001 0,003 0,002 0,001
1,28 (1,11-1,47) 3,88 (2,37-6,34) 2,00 (1,27-3,14) 2,51 (1,41-4,48) 1,71 (1,23-2,37) Factors related to amputation. Drop out: n=144
Jeffcoate et al 2006 UK (104)
449 All DFU
Prospective
Primary healed 65,7% Amputation 8% Mors 10,9%
ND
ND
ND
Lost to follow up: 3,8%
Shojaiefard Iran 2008 (105)
146 All DFU
Prospective
Primary healed 71,2% Minor amp 22,6% Major amp 5,5% Mors 1,3% Hyperglycaemia Ischemia Nephropathy
0,0109 0,0101 0,0345
3,01 (1,32-6,83) 3,03 (1,28-7,18) 2,64 (1,6-6,60) Factors related to amputation
Richard et al France 2010 (106) 304 DFU inpatient with infected wound
Prospective
Primary healed 33% Minor amp 33% Major amp 8% Mors 8% Multiple toes involved Deep ulcer Osteomyelitis
NK
NK
Outcome after 12 months Drop out: n=13
T
able 3. Overview of studies assessing outcome of foot ulcers
> 12 months.
Author Country Year
n
Design
Result
Factors related to outcome
p= OR (95%CI) Comments Apelqvist et al Sweden 1993 (23) 558 All DFU Prospective
Primary healed 345 Minor amp 48 Major amp 75 Mors 90 Age Distal perfusion Neuropathy <0,0001 <0,001 <0,001
Larsson et al 1998 Sweden (18)
187 All DFU requiring amputaiton
Prospective
Primary healed 0 Minor amp 74 (35,5%) Major amp 88 (47%) Mors 25(14%)
Age CVD Hemoglobine
<0,001 0,032 <0,001 1,073 (1,035-1,112) 2,925 (1,096-7,811) 0,943 (0,92-0,967) Factors related to major amp
O’-Rourke et al 2001 Australia (110) 126 All DFU
Prospective
Primary healed 27% Minor amp 36% Major amp 27% Mors11% Ischemic Age>60 0,0006 0,03
NK
Factors related to major amp
Oyibo et al UK & USA 2001 (97)
194 DFU
Observational 18 months follow up Primary healed 65% Major amp 15,5% Mors 3,5% Ongoing 16% Ulcer size Ichaemia
0.04 0.03
1.08 (1.01±1.14) 1.69 (1.06±2.70) Factors related unhealed at the end of the study period
Hartemann- Heurtier et al Frankrike 2002 (108)
118 DFU Wagner 3-5
Prospective
Primary healed NK Minor amp n=37 Major amp n=3 Mors n= 10 PAD without by- pass surgery Renal replacement therapy
0,0004 0,393
0,462 (0,292-0,728) (0,156-0,982) Factors related to longer healing time
Moulik et al UK 2002 (111)
185 All DFU
Prospective
Primary healed NK Minor amp NK Major amp 16% Mors 28%
ND
ND
ND
Outcome after 5 years
Faglia et al Italy 2006 (107)
564 DFU with >50% stenosis
Retrospetive
Primary healing NK Minor amp NK Major amp 9,7% Mors 30,7%
No revascularizat. Occlusion of each crural arteries Wound infection Dialysis TcPO2 increase (1mmHg)
<0,001 0,022 0,004 0,001 <0,001
35,9 (12,9-99,7) 8,20 (1,35-49,6) 2,1 (1,3-11,7) 4,7 (1,9-11,7) 0,80 (0,74-0,87) Factors related to major amp
Gul et al Pakistan 2006 (112)
383 DFU
Prospective
Primary healed: 148 (74%) Minor amp NK Major amp 3 (1,5%) Mors 49 (24,5%)
W
agner
UT 2 UT3
45,5 (3,48-594,68) 2,9 (0,37-23,83) 9,5 (1,15-77,27) Factors related to major amp
Li et al China 2011 (109)
520 DFU in patients 2000-2009 Cross sectional Retrospective
Primary healed 78% Minor amp 14,8% Major amp 6,7% Mors NK WBC count sCRP PVD Triglyceride
<0,0001 0,037 0,007 0,006
1,146 (1,075-1,222) 1,041 (1,002-1,082) 4,529 (1,500-13,676) 0,614 (0,433-0,869) Assessment of medical records Factors related to amputation
Taylor et al USA 2011 (113)
706 DFU (917 ulcers)
Prospective
Primary healed 27% Minor amp 34% Major amp 25% Mors 66%
Healing Ischemia Age ESRD Hyperlipidemia
NK
0,42 (0,33-0,53) 1,57 (1,27-1,93) 1,03 (1,02-1,03) 2,20 (1,79-2,70) 0,70 (0,58-0,85) % per 917 ulcers, Mors% per 706 persons Predictors of amputation free survival
DM = Diabetes Mellitus DFU = Diabetes Foot ulcer UT
= University of
Texas ulcer classification score
NK Not Known ND Not Done
T
T
able 3. Overview of studies assessing outcome of foot ulcers
> 12 months.
Author Country Year
n
Design
Result
Factors related to outcome
p=
OR
(95%CI)
Comments
Faglia et al Italy 2006 (107)
564 DFU with >50% stenosis
Retrospetive
Primary healing NK Minor amp NK Major amp 9,7% Mors 30,7%
No revascularizat. Occlusion of each crural arteries Wound infection Dialysis TcPO2 increase (1mmHg)
<0,001 0,022 0,004 0,001 <0,001
35,9 (12,9-99,7) 8,20 (1,35-49,6) 2,1 (1,3-11,7) 4,7 (1,9-11,7) 0,80 (0,74-0,87) Factors related to major amp
Gul et al Pakistan 2006 (112)
383 DFU
Prospective
Primary healed: 148 (74%) Minor amp NK Major amp 3 (1,5%) Mors 49 (24,5%)
W
agner
UT 2 UT3
45,5 (3,48-594,68) 2,9 (0,37-23,83) 9,5 (1,15-77,27) Factors related to major amp
Li et al China 2011 (109)
520 DFU in patients 2000-2009 Cross sectional Retrospective
Primary healed 78% Minor amp 14,8% Major amp 6,7% Mors NK WBC count sCRP PVD Triglyceride
<0,0001 0,037 0,007 0,006
1,146 (1,075-1,222) 1,041 (1,002-1,082) 4,529 (1,500-13,676) 0,614 (0,433-0,869) Assessment of medical records Factors related to amputation
Taylor et al USA 2011 (113)
706 DFU (917 ulcers)
Prospective
Primary healed 27% Minor amp 34% Major amp 25% Mors 66%
Healing Ischemia Age ESRD Hyperlipidemia
NK
0,42 (0,33-0,53) 1,57 (1,27-1,93) 1,03 (1,02-1,03) 2,20 (1,79-2,70) 0,70 (0,58-0,85) % per 917 ulcers, Mors% per 706 persons Predictors of amputation free survival
DM = Diabetes Mellitus DFU = Diabetes Foot ulcer UT
= University of
Texas ulcer classification score
Previous studies on factors related to ulceration, and the probability for ulceration, as well as re-ulceration rates are scarce. See table 4. These studies have required large samples (n=400-6613). In order to organise such studies, postal questionnaires (114, 115) have been used, for patients to self report the number of ulcers on their feet. This method might have excluded patients with health status impairing their ability to fill in and mail a postal survey which constitutes a limitation of the results, and may explain the relatively low incidence 2,2 per annum (114) and 5,0 per 100 person years (115) respectively. Reiber et al (25) and Smith et al (116) assessed per definition high risk patients, as the inclusion criteria was to have had a previous foot ulcer, while Abbott et al (114) and Oyibo et al (97) did not assess the cohorts according to risk classification. However, Smith et al (116) did not report ulceration rates in this identified group, only the number of amputations after a 2 year follow up. Amputation rates might be affected by the health care organization and not always by patient related factors. The four studies stated neuropathy, prior foot ulcer, foot deformity and ischemia as background factors for ulceration, while Reiber et al identified shoe wear and external trauma, often in the household, as direct ulcerating causes (25). See table 4. There is a need for more robust follow up until a defined endpoint (complete healing or death) for a more holistic view of the patients’ health status and its impact of outcome of the foot ulcer.
T
able 4. Overview of studies describing factors related to ulceration. Author Country Year
n
Design
Result
Factors related to ulceration
p=
OR (95%CI)
Comments
Abbot et al UK 2002 (114)
6613 DM of whom 165 with DFU Descriptive 2 years follow up 2,2%average annual incidence (n=291) Ongoing DFU Neuropathy Reduced pulses Foot deformities Age <0,0001 <0,0001 <0,0001 <0,0001 0,003 5,32 (3,71-7,64) 2,32 (1,61-3,35) 1,80 (1,40-2,32) 1,57 (1,22-2,02) 0,99 (0,98-1,00) Postal questionnaire
Reiber et al USA 2002 (25)
400 History of DFU
RCT Therapeutic shoes vs usual shoes 2 years follow up
21% vs 24%
Shoe wear 28,6% External trauma 30,9%
ns
Smith et al USA 2003 (116)
400 Previous DFU Age 45-84 Ability to walk Observational 2 years follow up
Major amp 3%
Smoking Neuropathy Absernt pulses
NK
4,1 (0,5-34,3) 7,43 (1,0-59,5) 4,0 (1,2-13,6) Foot exam every 17 weeks Factor related to amputation.
Boyko USA 2006 (115)
1285 DM
Descriptive 3,38 years Incidence 5,0/100 person years (n=
216)
Hba1c Impaired vision Prior foot ulcer Prior amputation Neuropathy Tinea pedis Onychomycosis
<0,0001 0,05 <0,0001 <0,0001 <0,0001 0,035 0,004
1,10 (1,06-1,15) 1,48 (1,00-218) 2,18 (1,61-2,95) 2,57 (1,60-4,12) 2,03 (1,50-2,76) 0,73 (0,54-0,98) 1,58 (1,6-2,16) Postal questionnaire
Nursing in home nursing setting
Few relevant studies were identified regarding diabetes in home nursing, and the conclusion was drawn that there has been performed a limited amount of research.
Löfgren et al has identified overtreatment with blood glucose lowering pharmacological treatment in assisted living facilities in a Swedish county (117), and diabetes was identified as being a risk factor for pressure ulcers on the heels by Pham et al (118). Studies regarding the professional work of the registered nurse in home nursing settings, have not covered diabetes care in particular, but five Swedish thesis describe the home nursing nurses’ work situation in general: Gustafsson, Josefsson, Törnvall, and Modin (56, 71, 72, 86). All together they reveal a work setting with extensive responsibilities for registered nurses, an important coordinating role and huge medical responsibility (86). The registered nurses were described as in a vulnerable situation with risk of physical threats and psychological distress, they have older educations and long professional experience (56). Modin has described the importance of interdependency and collaboration between district nurses and family physicians (71). Törnvall and Modin stated that physicians use the nursing records as a source of information about the patients’ status, but also that this intention was hampered by deficiencies in the records (71, 72). Törnvall described in a study of district nurses’ documentation that these were incomplete as they lacked nursing status, diagnosis and goals for the activities performed, while on the other hand medical facts were carefully documented (72). In another study Janson has pointed out the importance of structured care plan documentation’s impact on quality of care. It was shown that registered nurses who applied a process oriented method of working adopted a nursing perspective in the assessment and decision making pertaining to the patients’ nursing needs, while this was not the case for registered nurses who worked in a more medical way (119).
Prevention
A recent systematic review by Arad et al (120) of randomized trial studies on preventing the occurrence of diabetic plantar foot ulcers concluded that most studies were small, of poor quality and applied only to high risk patients. Ragnarsson Tennvall compared in a Markov-based 5-year cost-utility simulation current versus optimal prevention of foot ulcers in patients with diabetes. In the model hypothetical cohorts of patients older than 24 years, with eight possible health states in four risk groups of foot ulcers were included. Optimal
prevention was defined according to the International Consensus on the Diabetic Foot. The simulation concluded that intensified prevention strategy including patient education, foot care and appropriate footwear is cost-effective if the risk for foot ulcers and lower extremity amputations can be reduced by 25 %, and that providing all patients with diabetes at risk or high risk for foot ulcers and amputations with adequate prevention would be a effective or even cost-saving strategy. This would be valid for all patients with diabetes except those with no specific risk factors (22).
Patient education
Hjelm has described that one of the main obstacles for patients to prevent foot ulcers, is that they do not understand the connection between diabetes and neuropathy and its impact on daily life. This lack of understanding complicates for the patients’ self care (121).
A systematic review based on randomized controlled trials of the effectiveness of education in preventing foot ulceration in patients with diabetes was performed 2010 by Dorrestejn et al (82). Primary outcomes of the included studies were: incidence of foot ulceration, incidence of infection, incidence of amputation and ulcer recurrence. Secondary outcomes were: callus development, resolution of callus, number of and duration of hospitalizations due to foot problems, foot care knowledge scores, and patient behaviour assessment scores. Methodological problems the authors faced were: how to assess comparability between patient groups with or without ongoing ulcers; different durations of diabetes; different types of health care settings; different outcomes in the studies; different quality of the studies; and different educational interventions. Nine studies were identified meeting the inclusion/exclusion criteria, and the overall conclusion was that little evidence is available to support patient education for the prevention of foot ulcerations and amputations. The authors concluded this amount to an absence of evidence rather than evidence of in-effectiveness (82). Lincoln et al investigated the effect on ulceration, using two educational interventions in patients with previous foot ulcers in a randomized trial on 167 patients. The study did not reveal statistical significant differences in re-ulceration in the two groups, in spite of improved self care habits. However, methodology was more concentrated on content of education, than pedagogical methods for the transfer of information they provided (122).Thus the question of which patient education method is most effective remains unanswered.
Previous studies have failed to prove the effect of patient education on the development of foot ulcers. It must be explored whether the problem is patients’ knowledge and understanding, registered nurses’ inability to teach, or patients’ inability to follow given instructions, alone or in combination. Co-morbidity is a limiting factor for education intervention, being either for cognitive reasons (some cognitive disorders may require specialized competence of the educator) or physical reasons (the patients have learned and understood what is needed but is incapable of performing the required actions due to co-morbidity) or lack of power, if patients’ life situation does not allow him/her to make independent decisions (74). The above mentioned studies all cover patients who are able to take care of their own self care. Patients with co-morbidity who are dependent on home nursing service were excluded (122), which constitutes a selection bias.