Artificial Intelligence
in Healthcare
MASTER THESIS WITHIN: General Management NUMBER OF CREDITS: 15 Credits
PROGRAMME OF STUDY: Engineering Management AUTHOR: Julia Floruss and Nico Vahlpahl
JÖNKÖPING May 2020
Acceptance of AI-based Support Systems by Healthcare
Professionals
i
Master Thesis in General Management
Title: Artificial Intelligence in Healthcare: Acceptance of AI-based Support Systems by Healthcare Professionals
Authors: Julia Floruss and Nico Vahlpahl Tutor: Dinara Tokbaeva
Date: 2020-05-16
Key terms: Artificial Intelligence, Healthcare, Technology Acceptance, UTAUT
Abstract
Computer systems based on AI are becoming increasingly important in almost all industries, including healthcare, where AI can help doctors, medical staff, hospitals and pharmaceutical companies overcome practical challenges by providing data-based decision support to achieve efficient yet value-oriented care. Nevertheless, the acceptance of these new technologies varies widely across industries, with healthcare remaining a laggard.
The aim of this study is to gain a better understanding of the reasons why AI-based systems are not yet widely used in the healthcare sector. Therefore, the key determinants for the acceptance of AI-based systems by healthcare professionals will be investigated, with a detailed analysis of the user side based on an extended UTAUT model.
A self-administered online survey was conducted to collect data, yielding 258 responses from healthcare professionals, mostly from Germany, which were then analysed using SmartPLS. First, we employed partial least squares structural equation modelling (PLS-SEM) to ensure the reliability and validity of the measurement model, and then evaluated the structural model in terms of path coefficients and strength of relationship to test our hypotheses derived from the extended UTAUT model. In addition to testing the hypotheses, we conducted a multigroup analysis to compare the differences between several groups of participants and thus gain deeper insights into the key determinants.
In general, the results show that only about 20 percent of the respondents are currently using AI-based systems in their work. The analysis supported nine of the ten proposed hypotheses and revealed that trust is by far the most influential determinant of the behavioural intention to use AI-based systems, while social influence seems to have no effect at all. In addition, we identified four significant moderating effects based on three different demographic characteristics of the respondents, namely origin, education and work experience.
ii
Table of Contents
1
Introduction ... 1
1.1 Background... 1
1.2 Problem Statement... 2
1.3 Purpose and Research Question ... 4
1.4 Structure of Thesis ... 5
2
Theoretical Background ... 6
2.1 Literature Review Procedure ... 6
2.2 Artificial Intelligence in Healthcare ... 7
2.2.1 Disease Detection and Diagnosis... 8
2.2.2 Decision-making and Treatment... 10
2.2.3 Operations Management in Medical Institutions ... 12
2.2.4 Drug Research and Discovery ... 13
2.3 Technology Acceptance ... 14
2.3.1 Overview of Technology Acceptance Models ... 15
2.3.2 Unified Theory of Acceptance and Use of Technology (UTAUT) ... 16
2.4 Acceptance of AI-based Systems in Healthcare ... 17
2.5 Proposing an extended UTAUT for AI in Healthcare ... 19
3
Method ... 23
3.1 Research Philosophy ... 23
3.2 Research Approach ... 24
3.3 Research Design ... 25
3.4 Data Collection ... 27
3.5 Data Analysis Procedure ... 28
3.6 Research Quality ... 29
3.7 Research Ethics ... 30
4
Data Analysis ... 32
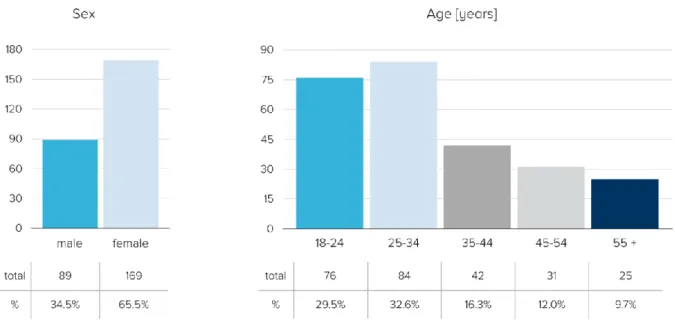
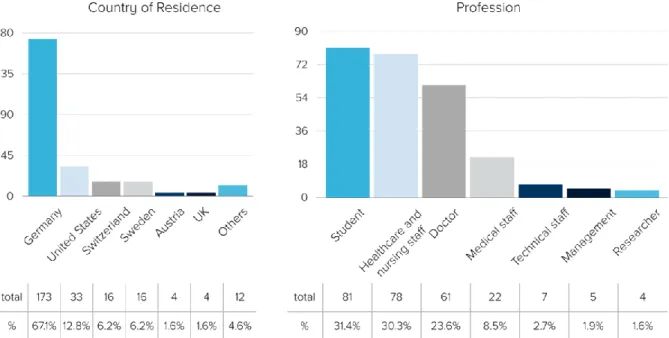
4.1 Description of Empirical Data ... 32
4.2 Partial Least Squares Structural Equation Modelling ... 36
4.2.1 Measurement Model ... 36
iii
4.2.3 Model Fit ... 42
4.3 Multigroup Analysis (MGA) ... 43
4.3.1 Measurement Invariance of Composite Models (MICOM) ... 44
4.3.2 Multigroup Analysis Results ... 46
4.4 Summary of Empirical Findings and Comparison ... 47
4.5 Results of Open Question in Survey ... 49
5
Conclusion ... 50
6
Discussion ... 52
6.1 Discussion of Findings ... 52
6.2 Implications ... 53
6.3 Limitations ... 54
6.3.1 Limitations of Theoretical Background ... 54
6.3.2 Limitations of Research Design... 55
6.3.3 Limitations of Data Set ... 56
6.3.4 Limitations of Data Analysis ... 56
6.4 Further Research ... 57
7
References ... 59
iv
List of Abbreviations
AI – Artificial Intelligence
ANN – Artificial Neural Networks
BI – Behavioural Intention
CNN – Convolutional Neural Network
CT – Computer Tomography EE – Effort Expectancy
FC – Facilitating Conditions
GLARE – Guideline, Acquisition, Representation and Execution
IT – Information Technology
MRI – Magnetic Resonance Imaging
PE – Performance Expectancy PEOU – Perceived Ease of Use
PLS – Partial Least Squares
PU – Perceived Usefulness
SI – Social Influence
SEM – Structural Equation Modelling
TAM – Technology Acceptance Model
TRA – Theory of Reasoned Action
UTAUT – Unified Theory of Acceptance and Use of Technology VIF – Variance Inflation Factor
v
List of Figures
Figure 1: Literature Review Procedure ... 7
Figure 2: Evolution of Technology Acceptance Models... 15
Figure 3: Technology Acceptance Model ... 16
Figure 4: UTAUT Model ... 17
Figure 5: UTAUT extended by Trust and Personal Innovativeness ... 20
Figure 6: Tree Metaphor of Research Philosophy... 23
Figure 7: Descriptive Statistics - Sex and Age ... 32
Figure 8: Descriptive Statistics - Education and Work Experience ... 33
Figure 9: Descriptive Statistics - Country of Residence and Profession ... 34
Figure 10: Descriptive Statistics - Medical specialty ... 34
Figure 11: Current Use of AI-based Systems ... 35
Figure 12: Formed Groups for Multigroup Analysis ... 43
Figure 13: Extended UTAUT including Results ... 47
List of Tables
Table 1: Reliability and Convergent Validity of the PLS-SEM ... 37Table 2: Heterotrait-Monotrait Ratio ... 38
Table 3: Structural Model Assessment ... 39
Table 4: Assessment of Hypotheses ... 40
Table 5: MICOM Analysis Results ... 45
Table 6: Multigroup Analysis Results ... 46
Appendices
Appendix 1: Online Survey Questionnaire ... 70Appendix 2: Fornell-Larcker Criterion for PLS-SEM ... 71
Appendix 3: Answers to Open Question in Survey ... 72
1
1 Introduction
In this chapter, we present the background to Artificial Intelligence (AI) and its adoption in healthcare. First, we give an overview of the megatrend AI in general, highlighting the growing importance of AI in our lives and in the future of many industries. Then, we present the specific topic of AI in the healthcare sector, where the diffusion despite numerous solutions is still limited and in its early stage. Furthermore, we motivate the choice of the topic, outline the purpose of the study, and present the underlying research questions. At the end of this chapter, we describe the overarching structure of the work.
1.1 Background
People have been trying to expand their abilities by building tools ever since, which has led us to today's technological revolution that is augmenting human reasoning (Szolovits, 2019). Computers and adequate software are driving this development, with artificial intelligence being a particularly promising and far-reaching technology that has made considerable advances in recent years. It has spread to almost every industry, from autonomous vehicles to advanced manufacturing technologies, agriculture and healthcare applications, and is seen as a technology that is changing the face of virtually every aspect of life. However, it is only widely used in a few sectors, mainly in the internet and communications industry (Lu, Li, Chen, Kim & Serikawa, 2018). The overall growth is thereby driven by increasing computing power and the abundance of digitized data, combined with the strength of AI to recognize patterns among these billions of seemingly unrelated data points. This enables people in turn to think about how to analyse data, integrate information, and use the outcomes to improve decision-making (Hengstler, Enkel & Duelli, 2016).
Nevertheless, AI as a branch of applied computer science was introduced over 70 years ago by Allan Turing (1950), Warran McCulloch and Walter Pitts (1943). Since it is a broad field with a multitude of applications, there is still no generally accepted definition of AI. However, for the purpose of our research, we define AI based on the definition of the early founding fathers as a computer algorithm that performs cognitive tasks associated with human performance and intelligence (Turing, 1950). These algorithms are designed to train themselves, following the human approach to learning and, according to the latest research, are finally able to solve specific cognitive tasks even more efficiently, precisely and at lower costs than humans (Guerin, 2011; Robertson, Azizpour, Smith & Hartman, 2018).
2
In our research we focus on AI systems applied in the healthcare environment. Especially in this sector, AI is becoming more and more important and interesting due to the increasing accessibility of relevant health data and rapid progress in analytical techniques (Jiang et al., 2017). Also, the market of AI in the healthcare sector is rapidly increasing as it is expected to reach investments of about $6.6 billion by 2021 according to a study by Accenture, implicating a compound annual growth rate of 40 % (Collier, Fu, Yin & Christiansen, 2017). AI can help physicians, medical staff, hospitals and pharmaceutical companies to overcome practical challenges by providing data-based decision-making support to achieve efficient yet value-oriented care (Shinners, Aggar, Grace & Smiet, 2019). It also provides improved quality of outcomes for patients, as, for example, AI technologies can be even more accurate than radiologists in detecting malignant tumour and therefore exceed human intelligence (Liu et al., 2019). Beyond that, AI technologies can improve efficiency by optimizing processes through digital transformation, which also leads to cost reduction.
Summarizing these areas of application, we see four main use cases of AI in the healthcare sector. Firstly, the support in disease detection and diagnosis, secondly the support in decision-making and treatment, thirdly the optimization of the operations management in medical institutions and fourthly, the support in drug research and discovery (Jiang et al., 2017).
1.2 Problem Statement
According to the World Health Organization, there will be a shortage of about 13 million healthcare workers worldwide by 2035 due to the increasing disease burden, mostly driven by chronic and epidemic diseases and a steadily ageing population (Maarse, Jeurissen & Ruwaard, 2013; WHO, 2016). These general developments are lifting the cost of healthcare and thereby increasing inequalities in the provision of care among different social classes and between countries with different levels of economic maturity. One example is the recent spread of COVID-19, the largest pandemic of this century, which is putting severe pressure on the global healthcare system, as no one knows exactly who patient zero was, how many people are or were really infected and how a vaccine can be developed under extreme time pressure (Tanne, Hayasaki, Zastrow, Pulla, Smith & Rada, 2020). Therefore, the task of building a resilient and sustainable healthcare system will be more relevant than ever before.
Although the potential benefits and opportunities of using AI technologies in the healthcare sector seem promising, there are some limitations such as legal and regulatory constraints, availability of reliable and high-quality data and risks that may need to be taken
3
into account. Furthermore, not only the access to data, but also the degree of their standardization and integration into medical workflows is crucial for the development of self-learning algorithms as the quality of the data directly influences the capabilities and reliability of AI-based systems (Girshick, Donahue, Darrell & Malik, 2014). Therefore, the data quality needs to be ensured so that these technologies and solutions can be used safely and purposefully to achieve beneficial outcomes. A lack of cost-intensive infrastructure, systems or trained personnel and the high complexity and associated intransparency of such systems could also hinder their introduction. Finally, a certain degree of understanding, acceptance and trust on both sides, doctors and medical staff as well as patients, is crucial for the successful implementation of AI technologies and their mutually beneficial use (Baba, 1999; He, Baxter, Xu, Zhou & Zhang, 2019).
Besides these current limitations in the application of AI in healthcare, a growing number of companies are focusing on its integration and possible solutions to these limitations, driven by the potential impact that AI can have on public health and the healthcare sector in general. (Topol, 2019). Many large companies like Google and IBM entered this field of research years ago and already have fully functional solutions as for example Google Health1 and IBM Watson
Health2 as well as many start-ups that are emerging in this field. Those solutions are for example
medical image analysis systems using computer vision, precision medicine systems using patient data analytics or intelligent administrative workflow assistance systems.
Summarizing, it is apparent that on the one hand there is a strong need for such AI systems and on the other hand there are a lot of already existing solutions for those needs. However, the introduction of appropriate systems is generally very slow compared to the existing and constantly advancing solutions in this market and are currently limited to certain diagnosis areas such as medical image interpretation (Forsting, 2019).
Despite those practical and commercial activities, academic research is conducted in the general field of AI in healthcare. However, regardless of the specific medical field, disease or application, this research is almost exclusively conducted in the domain of medical science. In contrast, research on AI in healthcare from a business and management perspective is rare, and there is almost no literature in this limited body of research that addresses the disparity between existing solutions and actual implementation described above.
1 https://health.google
4
1.3 Purpose and Research Question
The problem outlined above shows that there is a disparity between the available AI solutions for medical applications and their actual use, which is due to several current technical and people-related challenges. Moreover, the existing research is almost exclusively conducted in the field of medical science.
Our research therefore addresses this gap in the existing business and management literature to find answers to why the introduction of AI systems in the healthcare sector is hesitant. We will investigate this gap and specifically examine the following questions:
RQ1: “How do healthcare professionals perceive AI-based support systems?”
RQ2: “What are the key factors determining the acceptance of AI-based support systems
by healthcare professionals?”
By answering these research questions, we contribute to the theoretical base of existing literature in technology acceptance by providing a better understanding of the attitudes, acceptance and trust of medical professionals towards the use of AI applications in their working environment. Through a deeper understanding and the resulting insights, we are able to investigate the causes why many of the solutions that already exist are not yet established and applied in medical institutions. Thus, our findings provide valuable management insights on how to adapt commercial offers to the actual needs of healthcare professionals in this respect, while being able to distinguish between several healthcare professions and countries. These insights are then the foundation to derive recommendations for further measures to increase the acceptance and the actual use of AI applications. In addition, we contribute to the still neglected area of business and management literature in the healthcare domain by broadening the discussion about healthcare topics in this community and by stimulating further research in this economically attractive and future-oriented field.
Finally, we contribute to the wider trend of using AI in healthcare, which will eventually lead to a more accessible, accurate and sustainable way of providing medical treatment, regardless of people's origin or financial means.
5
1.4 Structure of Thesis
Having introduced the background, the problem and the purpose of our study and established our research questions in chapter one, we provide an introduction to the theoretical background of AI in health care and theories of technology acceptance in chapter two. In order to do so, we identified and reviewed the relevant literature in both areas and then combined them to propose an extended technology acceptance model adapted to the purpose of this study. The third chapter deals with the research methodology and the chosen approach for sampling and conducting the empirical study, which is based on the previously proposed model. In chapter four, we then use SPSS and SmartPLS to analyse the data obtained through the online survey in order to test the proposed hypotheses and thereby generate findings and evidence that is interpreted in chapter five and used to answer the research questions. In the final chapters we discuss the results and interpretations and highlight their implications, ethical issues and limitations, which eventually leads to further research areas.
6
2 Theoretical Background
In this chapter we introduce the theoretical framework of our thesis. Initially, the literature review procedure is explained followed by the literature review in which we examine the existing literature in the field of AI in healthcare as well as technology acceptance, ultimately leading to the proposition of an extended UTAUT model.
2.1 Literature Review Procedure
In order to find relevant and appropriate literature for the theoretical framework of our study, we used primarily Web of Science as literature database since listed articles have to go through a pre-selection process that includes criteria such as impact or peer-review to ensure a consistently good quality, trustworthiness and relevance of the articles (Thomson Reuters, 2008). For identifying relevant studies and articles, the search was divided into three parts: AI in healthcare, technology acceptance and finally the intersection of both.
Starting the search with the first part, we specifically searched for relevant literature on AI in the field of healthcare, in other words the dependent variable in our research. Therefore, as shown in Figure 1, we used the keywords “artificial intelligence”, “machine learning”, “deep learning”, “neural network”, “medic*”, “clinic*” and “health*”. These keywords were then extended by application area specific keywords like “diagnos*”, “treatment”, “drug” or “management” to find relevant literature for the individual use cases. Following these search strings results in a very large body of research on these topics in general, which was used to get a broad overview of the respective domains. We then put the focus on articles only and further narrowed down the articles to be in the Web of Science categories ‘Business’ and ‘Management’ as shown in Figure 1.
For the second part of the search, we looked for studies and articles that shed light on the topic of technology acceptance, or in other words the independent variable of our study. For this, we used the keywords “technology”, “acceptance”, “attitude”, “user”, “behaviour”, “intention” and “adoption”. Within this search we found a lot of relevant literature, as this topic is very well researched and explored.
Finally, we combined both searches, to review the literature relating our independent to the dependent variables, which led to barely any relevant search results. Therefore, we also considered studies on user acceptance of AI-based systems in other healthcare settings such as telemedical technologies, mobile health systems and hospital information systems.
7
We selected the usable articles by reading the abstract and decided whether or not the article was relevant to the specific topic, depending on the purpose of their study and the methods used to achieve it. When reviewing we also considered and reviewed references from the literature found in order to obtain more specific and topic-related literature that we could not discover with the specific search strings.
Figure 1: Literature Review Procedure
2.2 Artificial Intelligence in Healthcare
In almost all areas of science and technology, artificial intelligence is currently causing a fundamental paradigm shift including the healthcare sector and is therefore a highly discussed topic (Topol, 2019). The information technology (IT) development in this sector has rapidly evolved from products to services to solutions (Frost & Sullivan, 2016). While medical products that enable well-founded and evidence-based care have played a major role in recent decades, Frost and Sullivan (2016) see the focus today on medical platforms that enable result-oriented care in real time. In the coming decade, however, the focus will shift towards medical solutions providing intelligent approaches to enable evidence-based as well as result-oriented healthcare. AI, robotics, virtual and augmented reality will be used to achieve these goals, with a focus on collaborative and preventive care. Through this interaction of technology-based products, platforms and solutions, an unprecedented level of medical precision can be achieved, reaching
8
down to the individual level, and potentially being able to predict and thus prevent disease in the future (Frost & Sullivan, 2016).
As outlined above, there are four main application areas of AI in the healthcare sector of which we will introduce the current state of research (Arnold & Wilson, 2017).
2.2.1 Disease Detection and Diagnosis
Firstly, AI can support the descriptive disease detection and diagnosis process currently carried out by trained medical personnel. Medical image interpretation as one of the leading applications of AI in healthcare is well researched and is already commercially used. Here, AI analyses medical images from magnetic resonance imaging (MRI) or computer tomography (CT) for various diseases, primarily cancer (Bigio et al., 2000; Esteva, Kuprel, Novoa, Ko, Swetter, Blau & Thrun, 2017). In addition, by constantly monitoring health data such as patient records or data from the increasingly prevalent wearables, it is able to detect a multitude of diseases at a very early and easier treatable stage, even before severe symptoms or clinical signs occur (Piwek, Ellis, Andrews & Joinson, 2016). AI thereby surpasses human intelligence by monitoring a seemingly unlimited amount of data, especially since the dominant part, 80 percent of health data, is currently unstructured and therefore of no use in current health systems (Wang, Hripcsak, Markatou, & Friedman, 2009). This means that ultimately the diagnosis supported by AI-based systems is evidence-based, hence free of cognitive bias and nearly eliminates misdiagnosis (Wang et al., 2009).
The limited business and management literature discovered by the search appears to be devoted to concrete algorithms and either training and testing of these algorithms, comparing or optimizing them.
Starting with the research conducted in training and testing specific algorithm, Esteva et al. (2017) trained a deep convolutional neural network (CNN) using a dataset of 129.450 clinical images consisting of 2.032 different diseases and tested its performance against 21 board-certified dermatologists on biopsy-proven clinical images with the most common and most deadly skin cancer. They found out that the CNN achieves a performance equivalent to that of all the experts tested and demonstrates an artificial intelligence capable of classifying skin cancer with a level of competence comparable to that of dermatologists (Esteva et al., 2017). The goal of a second study by Adam et al. (2002) is to identify better biomarkers for the early detection of prostate cancer using protein profiling technologies that can dissolve and
9
analyse multiple proteins simultaneously. Therefore, they used a protein biochip surface enhanced laser desorption/ionization mass spectrometry approach coupled with an artificial intelligence learning algorithm to differentiate prostate cancer from noncancer cohorts. The result shows a positive predictive value of 96% for the study population and 91% for the general population, making this method a highly accurate and innovative approach to the early detection/diagnosis of prostate cancer (Adam et al., 2002). In the study of Ryu, Chandrasekaran and Jacob (2004), a mathematical programming approach, known as isotonic prediction, was developed for disease prognosis and prediction of patient survival time. This approach was then tested for breast cancer prognosis and myocardial infarction prognosis and showed a high degree of prediction accuracy (Ryu et al., 2004).
Furthermore, Mangasarian, Street and Wolberg (1995) deal with linear programming-based machine learning techniques used to increase the accuracy and objectivity of breast cancer diagnosis and prognosis. This allows an accurate diagnosis without the need for a surgical biopsy. Results showed that the diagnostic system, which was trained on samples from 569 patients, achieved 100% chronological accuracy in the diagnosis of 131 subsequent patients (Mangasarian et al., 1995). Another study that is covering the training and testing of AI-based systems by Lee and Park (2001) investigates the use of artificial neural networks (ANN) to classify and predict the symptomatic status of HIV/AIDS patients. Therefore, publicly available HIV/AIDS data of the AIDS Cost and Services Utilization Survey (ACSUS) datasets were used as input and output variables. The results showed which factors will influence the classification of AIDS and HIV status, thus providing decision-makers and policymakers with more accurate information to enable them to implement better health systems (Lee & Park, 2001).
It emerged, that there are two studies that deal with the comparison of different AI-based systems with Statnikov, Aliferis, Tsamardinos, Hardin and Levy (2005) investigating cancer diagnosis and found out that multi-category support vector machines (MC-SVMs) are the most effective classifiers in performing accurate cancer diagnosis from gene expression data. A second study examined different models for designing disease decision support system (DDSS) by using data mining approaches. Their results show that the hybrid model surpasses the basic learning models in nearly all cases for the initial diagnosis of the diseases (Sarkar & Sana, 2019). One last study in the field of disease detection and diagnosis investigates in the optimization of existing AI-based systems. Ghaddar and Naoum-Sawaya (2018) tested how to optimize the algorithm for medical diagnosis of tumours based on microarray data by applying
10
a specific machine learning classification and feature selection approach. The results of the study show that this approach is simple, mathematically sound and produces low error rates, which is crucial for the development of advanced decision support systems Ghaddar & Naoum-Sawaya, 2018).
If we summarise the research in the field of detection and diagnosis of diseases, it becomes apparent that this research is entirely focused on the algorithms or systems themselves. These are then examined either by testing, comparing or optimizing such systems with results that are mainly related to the performance of the systems in various ways. In conclusion, with regard to the above studies, it can be said that AI-based systems have a very high accuracy in detecting diseases in a large number of cases and are as accurate or even more accurate than humans in all studies, with one remarkable result, namely the 100% accuracy of a breast cancer detection system (Mangasarianet et al. 1995).
2.2.2 Decision-making and Treatment
Secondly, artificial intelligence can support the prescriptive area of decision-making and treatment, which is currently also carried out by healthcare professionals. Here, AI can review every medical record, health journal, symptom, the latest research and case studies on treatment and effects (Arnold & Wilson, 2017). In addition to the pure access and availability of this data, AI systems identify patterns among this data that support timely medical decisions, treatment proposals, and task prioritization through extensive data analysis (Bennett & Doub, 2016). For example, AI can predict the likely progression of diseases such as chronic conditions based on current patient status, coordinate care plans, and even help patients adhere to their treatment plans (Bennett & Doub, 2016). In this way, it helps medical staff to take a more comprehensive approach to disease management.
In this specific subdomain, we identified seven relevant studies within the business and management field which are, as in the previous sub-chapter, all related to a specific system and mainly focus on the development, training and testing of those. Hasan, Büyüktahtakın and Elamin (2019) propose new multi-criteria ranking algorithm (MCRA) that evaluates a wide variety of patient scenarios and offers the best patient-specific treatment alternatives for breast cancer. The results of the predictions were compared with the treatment proposals of five
11
different oncologists and it was found that in most cases the algorithm rankings are consistent with or statistically significantly correlated with the overall expert ranking. Thus, these multi-criteria ranking algorithm could be used as an accessible decision support tool to assist oncologists and to educate patients about appropriate and effective treatment alternatives for breast cancer (Hasan et al., 2019). Another study investigates a two-stage hybrid structure based on a multi-objective genetic programming (MOGP) algorithm and a hidden Markov model (HMM) to predict the activity status of individuals (Ni, Chen, Allinson & Ye, 2020). This algorithm is used as a decision support tool to provide real-time monitoring, statistical analysis and personalised advice as well as to promote positive attitudes towards a healthy lifestyle. The model was then tested with real data and compared to other popular two-stage hybrid models showing comparable performance (Ni et al., 2020). Gu, Deng, Zheng, Liang and Wu (2019) further examine how data-driven intelligent platforms (specifically the Case-Based Knowledge Management Systems in Healthcare) can support decision-making processes at different levels in hospitals. The results showed that the implementation of such systems has a significant and positive impact on group performance, group member satisfaction and group learning, with group member satisfaction in turn having a significant and positive impact on management performance and maintenance (Gu et al., 2019).
GLARE (GuideLine Acquisition, Representation and Execution), a domain-independent prototypical tool providing advanced artificial intelligence techniques to support medical decision-making was studied by Anselma, Bottrighi, Molino, Montani, Terenziani and Torchio (2011) and tested in real use cases, focusing on therapeutic decisions. A second application of the study by Mangasarian et al. (1995) mentioned earlier which is recently introduced into clinical practice, predicts when breast cancer is likely to recur in patients who have had their tumour removed. This gives the doctor and the patient better information about planning the treatment and can eliminate the need for prognostic surgery. Bertsimas, O’Hair, Relyea & Silberholz (2016) also uses machine learning in their study to predict the results of clinical trials for chemotherapy regimens in gastric cancer to improve the quality of clinical trials, concluding that their dataset of bygone trials needs to be supported by further research in current clinical practice. In another study an iterative data mining classification approach to improve treatment strategies was developed for chronic diseases in the case of patients with type 2 diabetes mellitus to predict and eventually eliminate treatment errors (Meyer, Adomavicius, Johnson, Elidrisi, Rush, Sperl-Hillen & O'Connor, 2014).
12
Summing up, the results of the studies in the area of decision-making and treatment are more blurred and do not provide concrete figures on the performance of the algorithms, but mainly indicate that the performance is comparable to human decisions, with only one study finding a significant positive effect.
2.2.3 Operations Management in Medical Institutions
Thirdly, AI-based systems can support the management of clinical facilities, their operation and the handling of patients. The main leverage of AI-based systems in this area is patient management, on the one hand to schedule appointments, determine appointment lengths, predict no-shows and thereby streamlining the influx of patients into the hospital (Hadavandi, Shavandi, Ghanbari & Abbasian-Naghneh, 2012; Kheirkhah, Feng, Travis, Tavakoli-Tabasi & Sharafkhaneh, 2016). As an example, an individual no-show costs around $200 and add up to a total problem of $150B in the U.S. alone. On the other hand, the internal planning of operating rooms or other laboratory facilities, which are a major profit driver and bottleneck for hospitals, can be streamlined and the right amount of time allocated to each procedure based on the individual patient and physician and thus reduce idle times (Marinagi, Spyropoulos, Papatheodorou, & Kokkotos, 2000). In addition, the time and labour-intensive pre-authorization process, which is a major financial burden, can be further automated by AI-based systems to automatically identify and collect key clinical information from patient records and provide staff with summaries of information to help them answer questions more quickly and accurately (Marinagi et al., 2000). Other use cases such as predictive denial management are less relevant, but all these technologies together can optimise the entire clinical operation and improve patient satisfaction and the quality of care provided by the staff (Spyropoulos, 2000).
Systematically reviewing the business and management in this subdomain revealed four studies, focusing on the development, implementation and testing of specific AI based systems. In a study by Soltani, Samorani and Kolfal (2019), machine learning techniques and an effective heuristic method were used to identify patterns in optimal or near-optimal schedules to optimize the appointment scheduling system by minimizing patients’ waiting time, providers’ idle time and overtime. The results showed an average schedule cost reduction of 16% per day as they tested their model on both simulated data and on a real-world application (Soltani et al., 2019). These results are confirmed by another study from Lee et al. (2015) which developed a decision
13
support system for the emergency department that combines machine learning, simulation and optimization to enable healthcare administrators to optimize workflows globally and improve the quality of care. When they tested their decision support system at a hospital in Atlanta, USA, the results showed that the efficiency improved throughput by more than 16 percent and reduced the number of patients leaving the emergency department without being seen by more than 30 percent (Lee et al. 2015). Liao and Chang (2011) further created a simulation model for the supply chain of the hospital logistics system (SCHLS) in their study which is based on neural networks and a genetic algorithm. This model was based on the dynamic Taguchi method and derived optimal combinations at factor level to optimize the adjustable contract capacities between the SCHLS and the pharmaceutical company. The research results show that the predicted response of the multi-performance in the optimal approach is better than that using the Taguchi method (Liao & Chang, 2011). In another setup, Schleyer (1994) optimized the development of a complex schedule with several demands for students’ clinical rotations in seven clinics by using a custom-coded algorithms and expert systems. The results saved 11 to 19 person days for programming and schedule development (Schleyer, 1994).
Summarising the research in this subdomain, the results indicate a noticeable reduction in the costs and time required for operational management in a clinical setup, thus suggesting that the implementation of AI-based systems is advantageous in this environment.
2.2.4 Drug Research and Discovery
Fourthly, AI can assist pharmaceutical companies in drug research and discovery. It can assist in drug development by helping to understand the relationship between the structure of a molecule and its activity in the human body, and thus predict the activity of a known or previously unseen molecule (Agatonovic-Kustrin & Beresford, 2000). This rather new field of application of AI is very promising to shorten the current 12 years a drug needs from the research lab to reach patients and thereby reduce the cost of developing new drugs (Weinstein et al., 1992). It will help ease the burden on healthcare systems and even make drugs available in parts of the world where they are necessary but currently unaffordable (Agatonovic-Kustrin & Beresford, 2000; Weinstein et al., 1992).
14
Here, the business and management literature is very sparse and includes two relevant studies that focus on testing specific AI-based systems. The first study by Turki and Taguchi (2019) proposed three transfer learning approaches for machine learning algorithms to improve the performance of drug candidate prediction, in order to avoid the expensive and time-consuming experimental process of high-throughput screening and to accelerate the drug discovery process by automatically assigning drug candidates. The results show that the proposed transfer learning approaches are performing better than the basic approaches in both predictive performance and statistical significance (Turki & Taguchi, 2019). A second study used decision tree induction and an artificial neural network to optimize decision support systems for predicting how antibiotic drugs should be taken (Hu, Wei, Cheng, & Chen, 2007). The results showed that the overall accuracy of the decision support system is significantly higher than that of the benchmark one-compartment pharmacokinetic model (Hu et al., 2007).
Summarizing this particular application of AI-based systems, very clear results can be seen, whereby the process of drug discovery is significantly accelerated by the use of such systems. The key points of the limited business and management literature on AI in health care indicate that AI-based systems are very accurate in detecting diseases, often remarkably better than humans, but at least as good in all studies, also in supporting decision-making. They also show that remarkable cost and time savings can be achieved in operational management and in drug research. However, it must be noted that there are no further studies that do not refer to the systems themselves, such as what effects these systems generally have on the financial situation of the medical institution or how these systems are perceived by doctors or patients.
2.3 Technology Acceptance
Technology must not only exist, work and deliver benefits in order to have an impact on society, but it must also be perceived as useful, accepted and ultimately used by someone to do so (Rogers, 2010). Following this path, the attitude of users toward new technologies is critical for the actual adoption of it and consequently its success (Davis, Bagozzi & Warshaw, 1989). In addition to the acceptance of the technology and its impact on the actual use, user feedback is a crucial source of information for improving a technology based on the needs and pains of users, which in turn makes acceptance of the technology more likely as the user, directly or indirectly, was involved in its creation (Cui & Wu, 2016).
15
In the following, we first introduce the origins of technology acceptance, followed by advanced technology acceptance models that are more case-specific, and finally we adapt the UTAUT model proposed by Venkatesh and Davis (2000) for our specific case of technology acceptance in healthcare.
2.3.1 Overview of Technology Acceptance Models
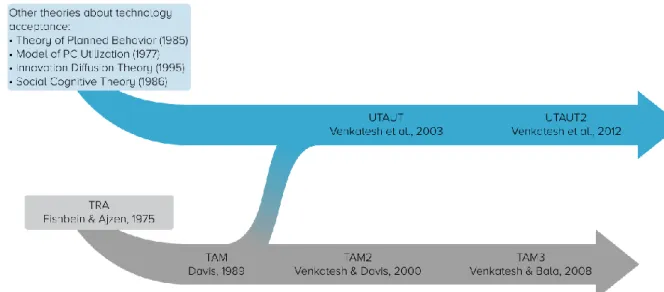
Together with the development of computers to become prevalent in all areas of life the question on why people accept or reject these new technologies emerged. Starting with Fishbein and Ajzen’s (1975) Theory of Reasoned Action (TRA), this stream of research began and a multitude of different theoretical models appeared to address this problem and improve these explanatory models as illustrated in Figure 2.
Figure 2: Evolution of Technology Acceptance Models (own elaboration based on Rondan-Cataluña et al., 2015)
Based on the TRA, Davis (1989) first proposed the Technology Acceptance Model (TAM) which was then advanced by Venkatesh and Davis (2000), investigating the acceptance of information systems by individual users and which was over time applied not only in this environment but also in a variety of user acceptance situations. This broad applicability turned the TAM into one of the most influential and widely established, yet simple, robust and powerful tools to investigate user acceptance of technologies in general (King & He, 2006; Lee, Kozar & Larsen, 2003).
16
This model, as illustrated in Figure 3, consists of two main factors: the perceived usefulness (PU) and the perceived ease of use (PEOU). PU refers to the assessment of a person to what extent the use of the new technology will improve work performance and the overall process. PEOU refers to a person's perception of how easy the use of the technology is to learn. These two factors determine the intention of a person to use the technology, eventually deriving the actual usage behaviour. In addition, the PEOU influences the PU positively, since easier usability of a technology represents a simplification and creates an increased benefit (Venkatesh & Davis, 2000).
Figure 3: Technology Acceptance Model (own elaboration based on Davis, 1989; Venkatesh & Davis, 2000)
The TAM was subsequently further developed firstly into the TAM2, adding constructs to precede PU and secondly adding antecedents to PEOU resulting in the TAM3. Those models are, however, more complex and specific to certain use cases and therefore not as relevant for general purposes as the original TAM (Venkatesh & Bala, 2008; Venkatesh & Davis, 2000). 2.3.2 Unified Theory of Acceptance and Use of Technology (UTAUT)
Due to the availability of different models and theories, many researchers have started to combine several theories ad hoc and adapt them specifically to their research. In order to maintain a coherent and consistent view of user acceptance, Venkatesh, Morris, Davis and Davis (2003) proposed a revision and synthesis of different models, which resulted in the Unified Theory of Acceptance and Use of Technology (UTAUT), as illustrated in Figure 4. This synthesis is based on an empirical comparison of eight earlier models, as shown in Figure 2, and includes parts from across all these models and their extensions to make it as complete as possible while maintaining its parsimony.
The resulting model (Figure 4) consists of four main factors: performance expectancy (PE), effort expectancy (EE), social influence (SI) and facilitating conditions (FC) (Venkatesh
17
et al. 2003). PE, EE and SI directly influence the behavioural intention (BI), which in turn, as in the case of the TRA and TAM, directly influences the actual use of the technology. The facilitating conditions (FC), however, do not influence BI, but, unlike TRA and TAM, directly influence the usage (Venkatesh et al. 2003). This model was also further developed and extended by Venkatesh et al. (2012), resulting in the UTAUT2 which incorporates additional factors that influence BI, but is again more specific and thus only has a limited applicability.
Figure 4: UTAUT Model (own elaboration based on Venkatesh et al., 2003)
2.4 Acceptance of AI-based Systems in Healthcare
In the two previous chapters, we presented the existing literature on the two domains of AI-based systems in healthcare and the models for technology acceptance separately. This chapter now offers an overview of the literature at the intersection of the two domains and provides a basis to compare our subsequent research against.
In an integrative review, Shinners et al. (2019) explored healthcare professionals’ understanding and experiences of artificial intelligence technology use in the delivery of healthcare, finding only one study that was fulfilling all inclusion criteria. Our systematic review revealed one more highly relevant study for exactly our purpose which we will both present below.
The first study by Fan, Liu, Zhu and Pardalos (2018) focuses on the acceptance of artificial intelligence-based medical diagnosis support systems by Chinese medical professionals. For this purpose, they extended the UTAUT model by several factors, including
18
trust. The main findings are that both initial trust (TR) and performance expectancy (PE) have the greatest influence on the behavioural intention (BI), with TR showing the strongest influence. Furthermore, their analyses show that effort expectancy (EE) and social influence (SI) have no significant effect on BI, which is contrary to the original position of UTAUT. These results show the importance of trust in the healthcare sector and that technology acceptance in this area is based more on personal concerns than initially intended by the originators of the technology acceptance models (Fan et al., 2018).
Alhashmi, Salloum and Mhamdi (2019) addressed in a second study specifically the adoption of AI in the field of patient monitoring in Dubai’s governmental health system. They proposed an extended TAM, which includes a multitude of external variables that are preceding the original TAM, investigating in a more technical and strategic direction of technology acceptance. Key findings are, that almost all hypotheses were confirmed showing a general confirmation of the original TAM model but rarely any new insights in the deeper reasons of acceptance or denial of AI in healthcare (Alhashmi et al., 2019).
Summarizing the limited literature in our research domain, it becomes apparent, that the two studies introduced above are both focused on a very specific part of the healthcare system, the diagnosis and the patient monitoring respectively. Our purpose in contrast is to investigate the broader acceptance of AI-based systems regardless of their actual use and therefore complement the existing research while contributing to open up towards all use cases presented in 2.2. Nevertheless, these studies confirm our approach to use an adapted UTAUT model, including trust, to investigate our research questions.
In addition to these two studies, which have a comparable purpose to our study, another study by Pan, Ding, Wu, Yang and Yang (2019) was conducted in a more specific area, namely the technology transfer from mHealth systems to the use of smart health services. They successfully extended the TAM with an antecedent "experience in the use of mHealth" to examine the attitudes of healthcare professionals and found that the level of this experience was the most influential determinant of behavioural intention (BI) for smart health services (Pan et al., 2019). This extension is very interesting, though, not applicable in our research due to a lack of existing AI-based systems in the clinical environment.
Furthermore, research has been conducted from other perspectives such as the patient perspective rather than the practitioner perspective (Hoque & Sorwar, 2017; Huang, 2010), which are however not relevant to our research. In addition to research on the acceptance of
AI-19
based systems, there are numerous studies that investigate the acceptance of other technologies in the healthcare sector, such as the research by Hu, Chau, Sheng & Tam (1999), who examined the applicability of TAM in explaining doctors' decisions for the acceptance of telemedical technologies. Two other studies presented a revised TAM model to examine the acceptance of mobile health systems (Wu, Wang & Lin, 2007) and hospital information systems (Handayani, Hidayanto, Pinem, Hapsari, Sandhyaduhita & Budi, 2017) from the perspective of healthcare professionals. Kim, Lee, Hwang and Yoo (2015) further considered the UTAUT model to examine the factors influencing the intention to use a mobile electronic patient record system among healthcare professionals, which overall underlines the importance and applicability of revised acceptance models in our research area.
Summarising the literature on the acceptance of AI-based systems in the healthcare sector, it becomes clear that this branch of research is rather backward in the field of business and management. There are only two articles that meet all inclusion criteria of our search and are reasonably relevant for our purpose, as they extend technology acceptance models to examine the acceptance of AI-based support systems by healthcare professionals. The other articles either examine more specific areas of AI applications in healthcare or user acceptance of other technologies and are therefore less relevant for our research.
2.5 Proposing an extended UTAUT for AI in Healthcare
After thoroughly reviewing relevant literature about various use cases of AI in healthcare as well as technology acceptance, we can conclude that for our research purpose, the UTAUT model is better suited than the TAM to assess the acceptance of AI-based systems by healthcare professionals. This is due to the more comprehensive view of the user's attitude offered by the UTAUT, allowing a more detailed analysis which in turn can lead to more valuable insights into the user's perception and ultimately facilitate more precise business-related conclusions (Venkatesh, Aliferis, Tsamardinos, Hardin & Levy, 2011). Further, UTAUT has become the most prevalent model in in the research domain of technology acceptance within healthcare (Fan et al., 2018). This leads us to propose an extended UTAUT model adapted to our specific purpose, which we present below together with the corresponding hypotheses.
Since AI-based systems are not yet widely available or used in practice, it is assumed that only very few medical professionals use these systems, and consequently we will presumably
20
not be able to collect valid data on the dependent variable use behaviour (U). Considering the literature and their key findings, however, we keep all four main independent variables as introduced above and subsequently extend them by two additional variables. Based on the original UTAUT model proposed by Venkatesh et al. (2003) we firstly propose the following hypotheses corresponding to three of these four variables, as illustrated in Figure 5.
Figure 5: UTAUT extended by Trust and Personal Innovativeness
Performance expectancy (PE), the degree to which a person believes the new technology would enhance his or her job performance, is directly influencing the behavioural intention and thus leading to our first hypothesis:
H1a: Performance expectancy positively influences the behavioural intention to use
AI-based systems.
Effort expectancy (EE), the degree to which a person believes it is easy to use of the technology, also directly influences the behavioural intention, leading to the second hypothesis:
H2a: Effort expectancy positively influences the behavioural intention to use AI-based
systems.
Social influence (SI), the degree to which a person believes his or her social environment wants him or her to use the technology, results in the third hypothesis:
21
H3: Social influence positively influences the behavioural intention to use AI-based
systems.
Facilitating conditions (FC), the degree to which a person believes all technical and organisational prerequisites exist to use the technology, has a direct influence on use behaviour (U) in the original model, which however becomes obsolete in our model due to the omission of U. Nevertheless, FC represents in general an interesting and important factor for technology acceptance, especially as a predecessor of performance expectancy (PE) and effort expectancy (EE). Many studies discuss this relationship and show the relevance and validity of this approach, even as it differs from the original model (Aggelidis & Chatzoglou, 2009; Maillet, Mathieu & Sicotte, 2015), leading to the following two hypotheses:
H4a: Facilitating conditions positively influence the effort expectancy of using AI-based
systems.
H4b: Facilitating conditions positively influence the performance expectancy of using
AI-based systems.
However, UTAUT itself lacks an important contextual predictor of technology acceptance in healthcare - trust - since healthcare is a personal subject that requires an empathetic layer beyond the existing, more technical factors (Gilson, 2003). Shinners et al. (2019) also concluded, that due to concerns about the impact on their patients, healthcare professionals' trust in emerging AI becomes an important determinant of their intention to use the technology. This extension was also examined by other studies in other technological fields, showing its general applicability and importance in some domains (Alharbi, 2014; Slade, Dwivedi, Piercy & Williams, 2015). Considering the impact of trust on the acceptance of AI systems, we consider trust (TR) as a factor, directly influencing the behavioural intention (BI) as illustrated in Figure 5, and propose the following hypothesis:
H5: Trust positively influences the behavioural intention to use AI-based systems.
In addition to this direct influence of trust (TR) on behavioural intention (BI), it can also be seen as a mediating variable for performance expectation (PE) and effort expectation (EE), as shown in Figure 5. First, several studies investigate the relationship between PE and TR, including Oliveira, Faria, Thomas and Popovič (2014) examining user acceptance of mobile banking with 194 participants and Gu, Wei and Xu (2016) investigating the acceptance of
22
wearable commerce with 266 participants. These studies show that PE has a significant influence on the formation of trust (TR) and thus underline our intention to investigate this relationship.
Secondly, the relationship between EE and TR was also previously investigated in different setups such as medical logistics systems (Tung, Chang & Chou, 2008) and E-commerce (Gefen, Karahanna & Straub, 2003) acceptance. These studies confirm that PE has a significant influence on TR, which in summary leads to the following two hypotheses:
H1b: Performance expectance positively influences the trust in AI-based systems. H2b: Effort expectance positively influences the trust in AI-based systems.
Another important factor in adopting new technologies is the personal innovativeness (PI), referring to the willingness of each individual to try out new technologies (Agarwal & Prasad, 1998). According to the classification of innovation adaptors in five categories: innovators, early adopters, early majority, late majority, and laggards, people tend to react differently on new technologies based on this inherent propensity (Rogers, 2010). This extension has shown to be useful and significant in prior technology acceptance studies in the field of healthcare (Fan et al., 2019) as well as in other domains (San Martín & Herrero, 2012; Slade et al., 2015) and not only in voluntary use cases (Leue & Jung, 2014) but also in organisational settings (Larsen & Sorebo, 2005). Given these prior use cases, we include personal innovativeness (PI) as a preceding factor to performance expectancy (PE) and effort expectancy (EE) in our extended UTAUT model as shown in Figure 5 and propose the following hypotheses:
H6a: Personal innovativeness positively influences the performance expectancy of using
AI-based systems.
H6b: Personal innovativeness positively influences the effort expectancy of using
23
3 Method
In the following chapter we introduce the research method and explain its connection to the purpose. Thereby, we describe the research philosophy, outline our systematic approach to the investigation as well as explain our choice of approach and how it fits into existing paradigms of research methods. We further present our research design and approach to data collection as well as data analysis, also regarding research quality and ethics.
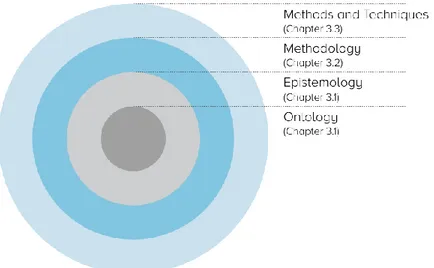
To structure this chapter, we will follow the tree metaphor proposed by Easterby-Smith, Thorpe and Jackson (2015) illustrated in Figure 6.
Figure 6: Tree Metaphor of Research Philosophy (own elaboration based on Easterby-Smith et al., 2015)
3.1 Research Philosophy
In scientific terms, the definition of research philosophy refers according to Easterby-Smith et al. (2015) to a system of beliefs and assumptions about the development of new knowledge. The innermost ring shown in Figure 6, ontology, is the core of the research philosophy as it represents the basic assumptions about the nature of reality, in other words, the way we think the world is. Ontological positions are situated on a continuum reaching from realism, which assumes that the world exists independent of perception and observations made about it, to nominalism, which assumes that there is nothing like reality as it is created in the human mind and depended on our perception (Easterby-Smith et al., 2015). The second ring, epistemology, describes the assumptions about the nature of knowledge and justified beliefs and thus the way of inquiring into the world, in other words, the things about it we believe can be known.
24
Positivists see the world as externally existing and its properties measurable through objective methods whereas social constructivists believe that reality is not objective and thus focus on how people make sense of it, representing the two standpoints within epistemology (Easterby-Smith et al., 2015).
As we introduced in Chapter 2, Theoretical Background, we base our research on the existing literature in the field of technology acceptance in general, in the specific case of AI-based systems in healthcare and current extensions to existing technology acceptance models. Based on this knowledge, we propose an adapted technology acceptance model, which is presented in 2.5 and which corresponds to a realistic and positivistic view, since with this approach we create a framework to explore the world from an external and observing view. This also enables us to draw generalisations from the sample to a larger population based on the collected and statistically analysed survey data from a viewpoint that is as objective as possible. Following the path of data collection and statistical analysis, there are no or very few possibilities to alter the data, so that they represent an objectified snapshot of the independently existing world in the form of likewise interpretation-free answers based on the Likert scale. Finally, the testing of predefined hypotheses implies an independent observer and thus, in combination with the preceding points, a strongly realistic and positivistic perspective.
3.2 Research Approach
Grounded on that core philosophy, we are following the tree metaphor to the third ring, methodology, where the literature presents three main approaches: deductive, inductive and abductive (Saunders, Lewis & Thornhill, 2012). A deductive approach is in essence about testing an established theory. On the basis of this theory, hypotheses are formulated and tested using logical and statistical methods applied to representative data, leading to the confirmation or rejection of it. An inductive approach is in essence about creating theory. Based on the collected data, patterns or themes are identified and generalized to develop new theories and hypotheses. An abductive approach is in between deduction and induction and explains 'incomplete observation' or 'surprising facts' based on data analysis (Saunders et al., 2012).
In the beginning of our study, we define all relevant terms based on existing and accepted literature within each field, AI in healthcare and technology acceptance, separately as well as combined in the field of technology acceptance in healthcare. Based on this strong theoretical focus in the beginning of our study we propose an extended UTAUT model, formulate
25
hypotheses and consequently fix our research objectives prior to the empirical data collection. This aligns with a deductive approach as well as the above described realistic and positivistic philosophy, ultimately leading to a quantitative approach (Creswell & Creswell, 2017; Easterby-Smith et al., 2015). According to Creswell and Creswell (2017), a quantitative approach focuses on the careful evaluation of a fixed set of variables that can be represented by quantifiable data to systematically answer theory-based hypotheses and the underlying research questions. This is contrasted by a qualitative approach that focuses more on individuals based on open-ended or conversational data collection and unique ways of data analysis. In general, the quantitative and qualitative approach corresponds to the deductive and inductive approach respectively and underlines the chosen quantitative methodology (Creswell & Creswell, 2017).
3.3 Research Design
Within a quantitative methodology the literature mainly distinguishes between a survey design and an experimental design (Creswell & Creswell, 2017; Easterby-Smith et al., 2015). Based on a theoretical framework, surveys intend to provide a quantitative description of regular and verifiable behavioural patterns to answer descriptive questions, questions about the relationship between variables and questions about their predictive relationship over time (Creswell & Creswell, 2017). Experiments, on the other hand, intend to manipulate single variables to study the effects of this manipulation on other variables or results of interest, while keeping all other variables constant, in order to isolate the effects and derive distinct causalities (Creswell & Creswell, 2017).
We propose an extended UTAUT model, which consists of several factors that ultimately influence the acceptance of AI-based systems by medical professionals. Based on this, we formulate hypotheses about each of these factors and their effects (see 2.5) in order to identify the subtle and difficult to explain relationships between them. According to Easterby-Smith et al. (2015), such relationships can best be deduced from a large sample of the population obtained through a survey and thus from a detached observational position. This is also consistent with other literature which states that a survey is tightly linked to a positivistic and realistic position (Creswell & Creswell, 2017; Saunders et al., 2012).
In order to follow our research strategy and answer our research questions, we conducted a survey using a self-administered online questionnaire. We used Google Forms for this purpose
26
as it is a reliable, free and easy-to-use tool to create an online survey that is compatible with both desktop and mobile devices. For designing the survey, we have formulated several questions or statements for each variable, which are based on the theoretical background as well as demographic questions that are relevant for our study. To determine the respondents' assessment of to what extent they agree or disagree with the given statements, we used a seven-point Likert scale with anchors ranging from “strongly disagree” to “strongly agree”.
An assessment using a Likert scale with seven levels has the advantage that tendencies of the respondents can be revealed, since there are three levels of agreement and disagreement and the respondents also have the opportunity to take a neutral position. All statements are mandatory and must be evaluated by the respondent in order to complete the survey.
The survey started with an introductory part in which we informed the respondents about the research topic to ensure that they have a basic understanding of the topic and also to stimulate their interest in participating. We have also informed them about the duration of the survey and explained that all data will be evaluated anonymously and will only be used for research purposes. This was followed by certain demographic questions such as gender, age, job title, medical field and others. After an initial question whether the respondent is already using AI-based systems or not, the statements for each factor of the extended UTAUT model are given. The complete questionnaire can be found in Appendix 1. Besides these general questions and statements in form of closed or rating questions, we included one open question to leave comments or thoughts of any related kind allowing us to collect not only quantifiable data but also some qualitative data, shedding light on why respondents hold their specific position.
The questionnaire was first developed in English, then pre-tests were conducted with ten different persons with a medical background to check the understanding and logic of the questionnaire. The suggested changes where evaluated with regard to the theoretical background and if possible integrated in the survey to improve its quality, consistency and validity. After this validation process the questionnaire was translated into German and made accessible online in both languages.
27
3.4 Data Collection
Considering the purpose of our study, which is to investigate the acceptance of AI-based systems by healthcare professionals, our target group implicitly emerges as all professionals working in the healthcare sector, since their acceptance is also the first prerequisite for the introduction of such systems. This target group was deliberately chosen to be as broad as possible and includes doctors, nurses, clinical management and other practitioners in order to identify differences between various professions, countries and other specifics. As there is a lack of existing literature on this topic in the field of business and management research, and as we want to introduce this topic into this area, it is evident that the target group should be studied on a broad scale in order to create a basis on which future research can build and examine the topic more specifically. Due to the current circumstances, which are explained below, we have expanded our initial target group to include medical students, as they represent the future medical professionals and in the dominant cases already have gained practical medical experiences.
In general, as well as in our case, this target population is too large to reach all individuals that compose it, which means that only a part, namely the sample, is used to answer the research questions with a reasonable amount of time and effort (Saunders et al., 2012). Sampling procedures can generally be divided into probability sampling and non-probability sampling. The choice of the sampling method in turn depends on how feasible and sensitive the data collection is in terms of answering the research questions (Saunders et al., 2012). In our study, we used non-probability sampling, or more precisely, a combination of snowball sampling and self-selection sampling, both voluntary sampling procedures. This choice allowed us to more specifically target our sample and allowed us to attract hard-to-reach members of the target population (Saunders et al., 2012).
To investigate our target population firstly using the snowball sampling method, we initially identified the largest hospitals both in Sweden and Germany and contacted the board or medical directors via E-mail. In this way we selected the first respondents and asked them to complete and distribute the survey as well as to identify and attract new respondents and ask them to repeat this process. However, it was difficult to reach a large number of respondents in this way because only few were willing to identify and attract new potential participants due to the current situation of COVID-19, thus breaking the sampling chain. Therefore, we also approached specialized clinics that do not currently have to deal with COVID-19. Additionally,