A two-year retrospective
evaluation of titanium and
cobalt-chromium
metal-ceramic fixed dental prostheses
Jovan Dražić
Miloš Dražić
Supervisor:
Camilla Ahlgren
Key words: chromium, clinical trial, cobalt, fixed dental prostheses, survival,
titanium.
Masters thesis (30 credits)
Malmö University
Tandläkarprogrammet
Faculty of Odontology
1
Abstract
Aim: The aim of this retrospective study was to evaluate the clinical quality of titanium (Ti) metal-ceramic and cobalt-chromium (Co-Cr) metal-ceramic fixed dental prostheses(FDPs) with a minimum follow up period of 2 years.
Methods: In 2012, 49 patients treated with FDPs during 2007-2010 at the Department of Prosthetic Dentistry, Faculty of Odontology, Malmö University, Sweden, were contacted after auditing dental technician bills. Twenty-one patients with a mean age of 59.2 years with 25 FDPs (13 Ti and 12 Co-Cr FDPs) agreed to participate in the study (10 men and 11 women). Evaluation of the metal-ceramic FDPs was made using a modified version of the California Dental Association (CDA) evaluation system. Success and survival rates were assessed. Statistical analysis was performed using Fisher’s exact test for differences between groups and for inter-examiner reliability the kappa value was calculated.
Results: The two groups did not differ significantly concerning the ratings according to the CDA evaluation system. Seven FDPs in the Ti group were evaluated as acceptable while there were 8 in the Co-Cr group. Six Ti and 3 Co-Cr FDPs were evaluated as correct/replace. The survival rate for the Ti FDPs was 81.3% and for the Co-Cr FDPs 92.3%. Three Ti FDPs showed chip-off fractures while two were recorded in the Co-Cr group. In either group one FDP exhibited caries on the abutment teeth.
Conclusions: Within the limitations of this study the clinical quality of the fixed dental prostheses was acceptable in both groups.
2
Sammanfattning
Mål: Målet med den retrospektiva studien var att bedöma den kliniska kvaliteten av metallkeramiska broar i titan-porslin (Ti) och kobolt-krom-porslin (Co-Cr) med en minsta uppföljningstid på två år.
Material och metod: 49 patienter behandlades med metallkeramiska broar i Ti och Co-Cr på avdelningen för Oral Protetik på Odontologiska fakulteten i Malmö under perioden 2007-2010. År 2012 kontaktades dessa patienter efter att tandteknikerfakturor gåtts igenom. 21 patienter (10 män och 11 kvinnor), med en medelålder på 59,2 år och 25 broar (13 Ti och 12 Co-Cr), deltog i studien. Broarnas kliniska kvalitet bedömdes med hjälp av en modifierad version av California Dental Association (CDA) kvalitetbedömningssystem. En bedömning av lyckande- och överlevnadsfrekvens genomfördes. Statistisk analys gjordes med hjälp av Fishers’ exact test vid bedömning av skillnaden mellan grupperna. För bedömning av skillnaden mellan bedömarna beräknades kappa värdet.
Resultat: Det förelåg ingen statistiskt signifikant skillnad mellan grupperna vad gäller bedömningen med CDA kvalitetbedömningssystem. Sju broar i Ti-gruppen, och åtta i Co-Cr-gruppen bedömdes som ”acceptable”. Sex Ti-broar och tre Co-Cr-broar bedömdes vara i behov av revision (”correct/replace”). Överlevnadsfrekvensen var 81,3 % för Ti-broarna och 92,3 % för Co-Cr-broarna. Tre Ti-broar och två Co-Cr-broar hade frakturer i fasadporslinet – s.k. "chip-off”-frakturer. Inom vardera grupp fanns en bro med karies på stödtänderna.
3
Slutsatser: Broarna visade acceptabel kvalitet inom båda grupperna. Med tanke på begränsningarna för den här studien bör försiktighet vidtas när man drar slutsatser utifrån resultaten.
4
Introduction
Restoring missing teeth with metal-ceramic fixed dental prostheses (FDPs) has been a standard replacement method for a long period of time. There are numerous brands of material from several global manufacturers. The proper selection and manipulation of alloys is critical to prevent failures of expensive restorations. If abused, even the highest quality alloy may not perform well intra-orally.
In Sweden, metal-ceramic reconstructions have been used since the early 1960’s. However, it was in 1999 that it was permitted to use base-metal alloys for fixed prosthodontics (1). For a long time high-noble alloys have been, and still are, considered the gold standard for metal-ceramic FDPs. Several reasons have over the past 25 years, forced manufacturers worldwide to pursuit new suitable alloys. Three major reasons are economics, physical properties and biocompatibility. The economic incentive arose when the price of gold was deregulated in 1969. It led to price fluctuations which resulted in a strong increase in the price for gold making base-metal alloys a much cheaper alternative (2). High elastic modulus is an important physical property in prosthetic dentistry because it means that the metal
substructure flexes to a lower extent not causing fractures of the overlying porcelain(2, 3).
This characteristic becomes extra important in long-span FDPs and when anatomical or esthetical constraints force a slim design. Cobalt-chromium (Co-Cr) has an elastic modulus (228 GPa) which is more than twice as high as the strongest gold-based alloy (90 GPa) while
titanium (Ti) is comparable to type IV gold alloy (103.4 GPa)(2, 4).
According to Wataha et al, corrosion is the single most relevant property for the biocompatibility of dental casting alloys. Corrosion occurs when one or more of the
5
released into biological environments and cause adverse effects such as systemic, local toxic reactions, allergic and even neoplastic reactions. Nickel and cobalt have relatively high potential to cause adverse reactions but the true risk for this to happen when using alloys containing these elements remains undefined and there is still a lot to be learned about the biocompatibility of dental casting alloys (5).
A review by Tschernitschek et al on Ti as a bioinert material states that adverse effects due to Ti and its alloys are rare and considerably less pronounced in comparison to that of other
metals. When Ti is oxidized it forms a stable surface layer of TiO2 which makes it very
corrosion-resistant. However, under mechanical stress Ti is as corrosive as many other base metals (6).
According to a review study and meta-analysis on survival and complication rates of FDPs made of high-noble alloys from 2004 by Tan et al (7), where 19 prospective and retrospective cohort studies were analysed, most of the studies on the long-term longevity date back to the 1980s and 1990s. Tan et al stated that 7 of the 19 included studies reported on FDP design and that 11.6% of the FDPs were metal-ceramic while the others were of gold-acrylic design. Accordingly there are few studies performed in the last century with long-term follow up on recent FDP materials. The success and survival rates were estimated to 71,1% and 89,1%, respectively after 10 years (7). Other studies on the longevity of Ti and Co-Cr FDPs have shown similar results with success rates of 62-62,5% and survival rates of 81,3-92,3% after a mean follow-up time of almost 4 up to 5 years (8, 9). Reports on the longevity of single crowns made of Ti and of Co-Cr have also shown satisfying results (10, 11).
6
In recent years the interest and use of base-metal alloys of Ti and Co-Cr in fixed
prosthodontics have increased markedly. The situations where one has to select between these materials often occur nowadays. Therefore, the aim of this study was to evaluate and compare the clinical quality of metal-ceramic FDPs made from Ti and Co-Cr. To the authors’
knowledge, no clinical studies have earlier been made with the objective to compare these materials to one another.
The hypothesis was that both Ti and Co-Cr FDPs would demonstrate good clinical quality and that FDPs made from Co-Cr would prove to meet these expectations to a greater extent.
Material and method
Patients
Dental technician bills of all consecutive patients receiving fixed dental prostheses, performed by dental students and dentists, during 2007, 2008, 2009 and 2010 at the Faculty of
Odontology, Malmö University, Malmö, Sweden were collected and audited. Forty nine patients who received Ti-ceramic (n = 27) and Co-Cr-ceramic (n = 28) FDPs during this period were informed by letter about the objectives of the study, clinical procedures and possible benefits and risks for the patient. Patients were thereafter contacted over the phone to ensure that they had fully understood the letter and to set up an appointment.
All patients who agreed to participate and signed a declaration of informed consent were included. For each patient, age, gender, position of the FDP, abutment teeth, endodontically treated abutment teeth and abutment teeth treated with a post and core were recorded. This information was retrieved from the patients’ records.
7 Clinical examination
The clinical examination was performed by two dental studentsbetween March and May
2012 andconsisted of a health declaration, anamnesis, digital intraoral radiographs (of the
abutment teeth), clinical photographs, assessment of caries and periodontal status of abutment teeth and tooth wear in general.
The examiners were calibrated by examination of FDPs with supervision by a
prosthodontist.Two examiners evaluated the FDPs independently using a modified version of
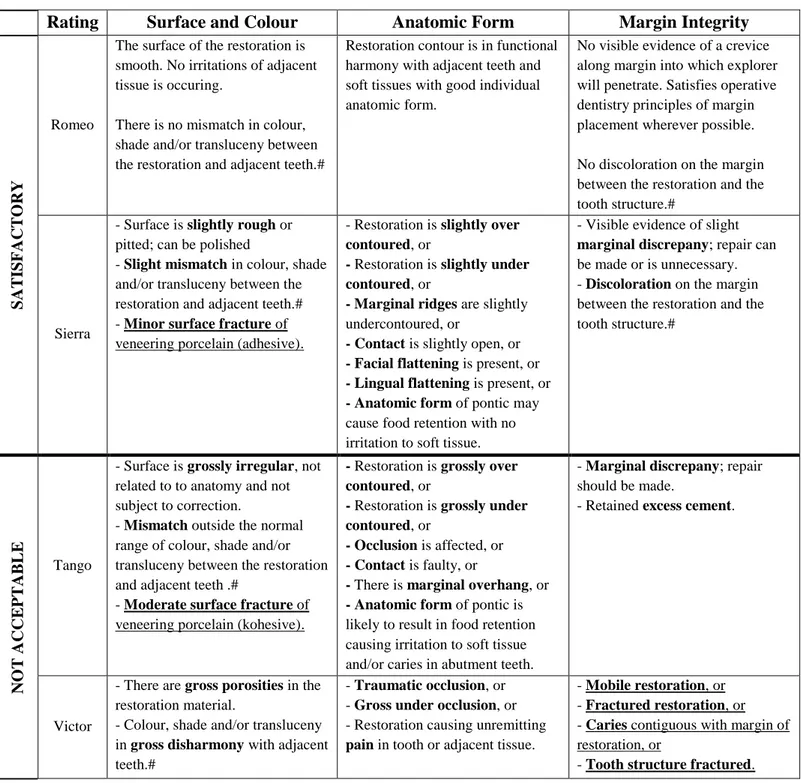
the California Dental Association (CDA) evaluation system. The criteria used are present in Table 1. The rating system provides for the rating into two main categories for each
characteristic, satisfactory and not acceptable. Within the two main categories there are two sub ratings available: the category “satisfactory” includes the sub rating “Romeo” which indicates a restoration within the “range of excellence” (“the restoration is of excellent quality and is expected to protect the tooth and the surrounding tissues”), and the sub rating “Sierra” which indicates a restoration within the “range of acceptability” (“the restoration is of acceptable quality and exhibits one or more features that deviate from the ideal”). The category “not acceptable” includes the sub rating “Tango” which indicates a restoration that “should be replaced or corrected for prevention” (“future damage to the tooth and/or
surrounding tissues is likely to occur”), and the sub rating “Victor” which indicates a
restoration that “must be replaced” (“damage to the tooth and/or its surrounding tissues is now occurring”). The overall quality rating of each FDP was based on the worst rating among the three characteristics surface and colour, anatomic form and margin integrity. If the two examiners’ evaluation differed, an agreement was reached after joint re-examination of the patient.
Periodontal status was assessed on the abutment teeth by registration of probing depth and bleeding on probing on 4 surfaces of each abutment tooth. The presence of caries on abutment
8
teeth was assessed by a dental explorer and digital intraoral radiographs. Tooth wear was assessed and registered as: no tooth wear to normal tooth wear into enamel or tooth wear into dentine. The patients were also asked if they were aware of present bruxing habits and if they used an acrylic splint. The condition of the soft tissue adjacent to the FDPs was noted if it deviated from the normal healthy appearance.
When assessing the survival and success rates all the patients who stated that their FDPs were lost when contacted by phone, and therefore not examined, were looked up in the patient database to identify the reason for failure, service time, location and abutment teeth.
Definitions
Survival of FDPs
Survival was defined as an FDP that was in position at the examination visit regardless of its condition.
Success of FDPs
An FDP was defined as successful if it was assessed as unchanged from the time when it was placed and no damage to the surrounding tissues had occurred to the time of examination. When using the CDA evaluation system in order to assess whether an FDP was successful or not, the criteria underlined in Table 1 were the only criteria used (minor surface fracture, moderate surface fracture, mobile restoration, fractured restoration, caries and tooth structure fractured). Since this is a retrospective study with no baseline examination, these criteria may change over time and could therefore affect the success rate.
9 Statistical analysis
Statistical analysis was performed using Fishers exact test (SPSS version 20.0) to analyse differences between groups, and for inter-examiner reliability the kappa value (SPSS version 20.0) was calculated.
Informed consent and ethical approval
Prior to the study, ethical approval was obtained by the local ethics committee (OD 2012/56) and each participant signed a declaration of informed consent.
Results
Patients
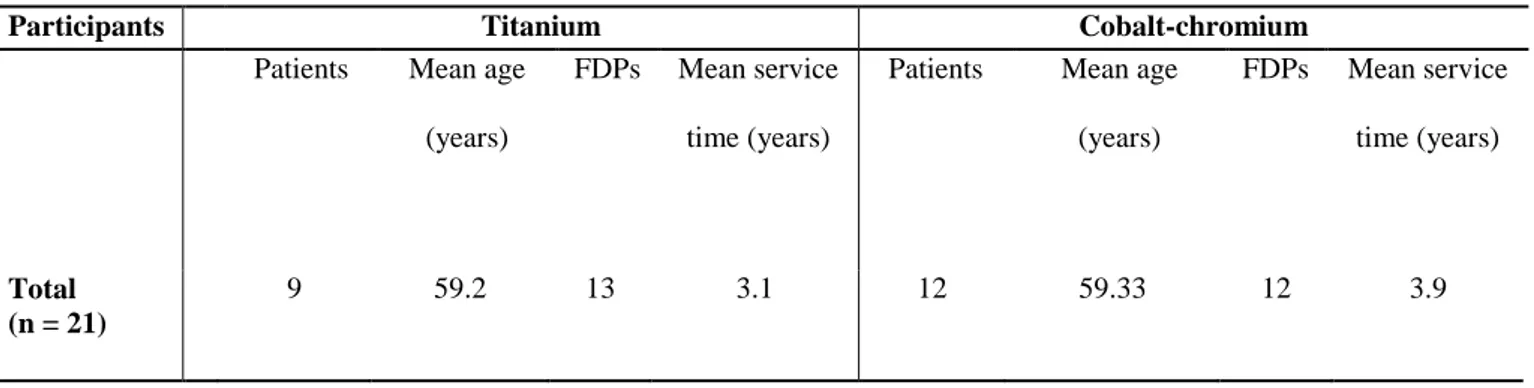
A total of 21 patients with a mean age of 59.3 years (range 38 to 89 years) participated in the study. There were 9 patients with 13 Ti FDPs and 12 patients with 12 Co-Cr FDPs, Table 2. The most frequent reason for nonparticipation was that the patients declined to participate (n=10) and because the patients were not reachable (n=9), Table 3. Four patients (with 3 Ti FDPs and 1 Co-Cr FDP) were regarded as drop out since they stated that their FDPs were lost when contacted over the phone. These FDPs were included as failures when assessing the survival rates and success rates for the two groups.
FDP features
10
Nine out of 25 of the FDPs (3 Ti FDPs or 23%, 6 Co-Cr FDPs or 50%) had at least one
endodontically treated abutment tooth, and out of these, four (1 Ti FDP, 3 Co-Cr FDPs) had at least one tooth that had been provided with a post and core. Almost half of the FDPs (6 Ti FDPs and 6 Co-Cr FDPs) were found in patients who had tooth wear into dentine registered at the time of the examination. Four of them stated that they used an acrylic splint while three stated that they were aware of present bruxing habits. All the FDPs had antagonising teeth. Regarding periodontal status, 7 FDPs in the Ti group and 8 FDPs in the Co-Cr group had abutment teeth with periodontitis. Twelve of the FDPs in the Ti group and 10 FDPs in the Co-Cr group had bleeding on probing on at least one surface of the abutment teeth. The soft tissue adjacent to the restorations had a healthy appearance in all patients.
Evaluation according to the CDA evaluation system
Concerning the overall rating of each FDP, 7 Ti (54%) and 8 Co-Cr (67%) FDPs were rated in the satisfactory level (the sum of excellent and acceptable ratings) while 6 Ti (46%) and 4 Co-Cr (33%) FDPs were rated as not acceptable (the sum of correct/replace and replace ratings).
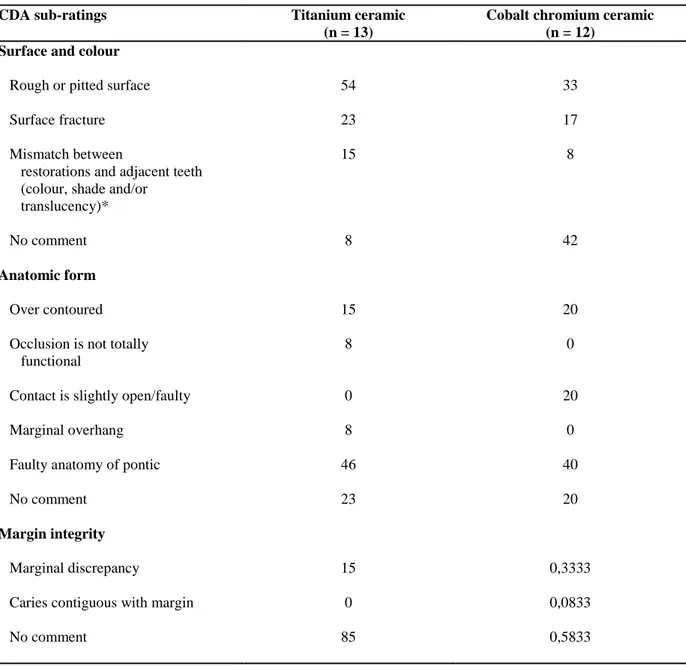
Surface and colour
In both groups the most recurrent rating of surface and colour was acceptable. The Ti FDPs had a higher percentage of both acceptable (69%) and correct/replace (23%) ratings for surfaces and colour than the Co-Cr (50% acceptable and 8% correct/replace). Consequently the Ti FDPs had a much lower percentage of excellent ratings than the Co-Cr. None of the groups had their surface and colour rated as replace (Fig. 1). The main reason for suboptimal rating for this characteristic in both groups was a rough or pitted surface (54% in the Ti group
11
and 33% in the Co-Cr) and secondly, surface fractures or “chip-off” fractures (23% in the Ti group and 17% in the Co-Cr) (Table 5).
Anatomic form
With regard to anatomic form, the Ti FDPs were most frequently rated as acceptable and correct/replace (38.5% and 38.5%, respectively) while the Co-Cr FDPs mostly represented the rating acceptable (58%). Approximately one fourth of the FDPs in both groups had the rating excellent. None of the FDPs were rated as replace (Fig. 1). Discrepancies from the optimal anatomic form were in either group mainly found to depend on pontics with faulty anatomy (46% in the Ti group and 40% in the Co-Cr) (Table 5).
Margin integrity
Regarding margin integrity the majority of the FDPs were rated in the satisfactory level. The rating excellent for margin integrity reached a high score in both groups (85% in the Ti group and 58.33% in the Co-Cr). One Co-Cr FDP got the worst possible rating due to caries
contiguous with the margin (Fig. 1). The most frequent remark on marginal integrity for the Co-Cr FDPs was marginal discrepancy. It was the single reason for reducing the rating for the Ti FDPs (Table 5).
Success and survival
Co-Cr FDP number 3 (CoCr3; Table 4) had caries contiguous with the margin of the FDP,
12
Ti5 and Ti7) showed moderate chip-off fractures after 3 years, 3 years and 10 months and 4 years of service time, respectively, resulting in framework exposure. All three FDPs were located in a posterior region of the maxilla on teeth 17-13, 24-26 and 23-27, respectively. In the Co-Cr group, CoCr9 had a moderate chip-off fracture resulting in exposed framework. The distal abutment tooth of this FDP had been endodontically treated through the occlusal surface resulting in a small composite filling, and the FDP was located in the maxilla on teeth 15-12. CoCr13 showed a minor chip-off fracture and was located in the mandible on teeth 44-47. With a total of four FDPs with moderate chip-off fractures, Ti7 had two root filled
abutment teeth, CoCr9 had two root filled abutment teeth and was placed in a patient with recorded tooth wear into dentine, Ti4 had one root filled abutment tooth and was placed in a patient with both recorded tooth wear into dentine, self-reported bruxing habits and the use of an acrylic splint (Table 4). No adverse reactions were seen on the soft tissue adjacent to the FDPs. Ten s in the Ti group and nine FDPs in the Co-Cr group showed no technical or
biological complications at the examination visit. The ratings given for these FDPs, according to the CDA evaluation system, were not based on criteria that are considered to be able to affect the success rate. Consequently, the success rate for the Ti group was 62.5% after a mean service time of 2 years and 10 months, and the success rate for the Co-Cr group was 69.2% after a mean service time of 3 years and 11 months.
Three FDPs (Ti3, Ti11 and Ti12) failed in the Ti group (Table 4 and 6). Two (Ti3 and Ti11) failed due to cusp-fractures; one with a service time of 8 months and the other, 2 years and 6 months. Both FDPs had an abutment tooth that was root filled and treated with a post and core prior to the prosthetic treatment. The fracture of Ti11 occurred on its distal cantilever in the region of tooth 24. The third FDP (Ti12) failed due to loss of retention as a result of caries in one of the abutment teeth. It had a service time of 1 year and 10 months. Consequently, after a
13
mean service time of 2 years and 10 months in the Ti group, the survival rate of the Ti FDPs was 81.3%. Only one failure (CoCr10) was registered in the Co-Cr group (Table 6). There was no information available about the service time or reason for failure for this FDP in the patient record. After a mean service time of 3 years and 11 months the survival rate for the Co-Cr FDPs was 92.3%.
There were no significant differences between the two groups regarding success rate, survival rate, overall CDA ratings or CDA sub ratings for any of the characteristic. The Ҡ-value statistics presented an inter-examiner reliability of 0.271 indicating a fair agreement between the examiners.
Discussion
The results show that the success rates, survival rates and overall CDA ratings are similar between the two groups with a slightly poorer result for the Ti FDPs, even though they have a shorter mean service time than the Co-Cr FDPs. This indicates that the research hypothesis is verified. Other studies with longer follow up times on the clinical quality and longevity of Ti, Co-Cr and other metal-ceramic FDPs, including two prospective clinical studies and one meta-analysis, show similar results to the present (7-9).
A modified version of the CDA evaluation system was used to evaluate the clinical quality and professional performance of the FDPs. This is a useful instrument but the criteria used to give the FDPs certain ratings are more or less subjective. This, together with the fact that the
14
classification system is composed of an ordinal scale, stresses the judgement of the examiner (12). The examination of the FDPs was made by two dental students and their lack of
experience in the matter may have influenced the outcome of the ratings. The CDA evaluation
system, however, is favourable from a clinical standpoint.When the CDA evaluation system
was developed, great effort was exerted to formulate criteria to reflect clinical significance making the final rating of the restoration lead to a possible treatment alternative (ex. repair is unnecessary, correct, replace/correct, replace). The developers chose to include the FDP characteristics of surface and colour, anatomic form and margin integrity since these are the characteristics most commonly considered to indicate restoration quality (12).
This study showed that the most frequent rating for surface and colour in both groups was acceptable (69% for the Ti group and 50% for the Co-Cr). One study by Lövgren et al, on Ti FDPs, showed that most of the FDPs were rated as excellent (75%) (9). Another study by Eliasson et al, on Co-Cr FDPs, showed that the majority of the FDPs were rated as acceptable (83,6%), in agreement to the current study (8). An explanation for the lower rating of the Ti group in the present study might be that there is a problem with metal-ceramic titanium reconstructions due to a poorer quality of bond strength for the low-fusing ceramics. In the last years however, several laboratory studies have presented a new generation of low-fusing ceramics that show acceptable physical properties and bond strength and even on the same level as the gold standard system of high-gold ceramics (13, 14). Lövgren et al determines that both the first and second generation of ceramics was used in their study. No attempts were in this study made to ascertain which generation of ceramics was used in the Ti group. Haag et al and Eliasson et al also reported the most frequent reasons for suboptimal rating of surface and colour as a rough or pitted surface and surface fracture of the porcelain (8, 10).
15
It is possible to design Co-Cr constructions with smaller dimensions due to the higher elasticity modulus of the material. The higher risk for over dimensioning FDPs made of Ti could explain why the present study reported that the Ti group received a lower rating (38,5% not acceptable) than the Co-Cr (17% not acceptable) with regard to anatomic form (2).
Lövgren et al reported that 97% of the Ti FDPs were rated in the satisfactory level and Eliasson et al reported that 99,6% of the Co-Cr units were rated in this level. Discrepancies from the optimal anatomic form were, in the present study, in both groups mainly found to result from a pontic with faulty anatomy - together with over contouring - with or without the presence of irritation of soft tissue. The same discrepancies were found by Haag et al while Lövgren et al almost only found over contouring to be deviating from the optimal anatomic form (9, 10).
The rating for margin integrity reached a high score in both groups (satisfactory level: 100% in the Ti group and 91,66% in the Co-Cr). The only reason for reducing the rating lower than satisfactory for the Co-Cr FDPs was a caries lesion contiguous with the margin. Similar results were found by Lövgren et al and Eliasson et al reporting that the FDPs were rated as 97% or higher in the satisfactory level, adding root fracture as a reason for rating the FDPs in the not acceptable level.
It is evident that studies show different results in CDA ratings which is also emphasized by Eliasson et al (8). Possible reasons for this could be different interpretations of the CDA guidelines, different distribution of clinical variables in the patient samples, for example,
16
bruxing habits, location of the FDPs, non-vital abutment teeth and cantilever extension pontic FDPs.
Since prospective clinical studies report that FDPs and crowns of metal-ceramics are rated sub optimal at baseline (9, 10), it is impossible to know how the FDPs in this retrospective study had changed from placement to the clinical follow-up examination, except in the case of more severe complications such as chip-off fractures or caries contiguous with the margin of the FDP, since it is not likely that the FDPs were placed in these conditions. Possible interceptive treatment between placement and clinical examination, such as adjustments made by a dentist, is another reason for not knowing if, and how, the FDPs had changed. The ceramic surfaces could for example have been polished, leading to a better rating in the category surface and colour. Since the information on the failed FDPs was retrieved from dental records, we had to rely on others for accurate record-keeping.
From a clinical perspective, it is important to emphasize the difference between the categories satisfactory and not acceptable rather than the difference between the sub ratings excellent and acceptable since the previous mentioned indicate if the FDP should be corrected/replaced or not.
This retrospective study was limited by a relatively small sample size. All patients treated with FDPs made of titanium-ceramic and Co-Cr-ceramic during 2007, 2008, 2009 and 2010 at the Faculty of Odontology, Malmö University, Malmö, Sweden were contacted. Due to the small number of patients (n=49) and FDPs (Ti, n=27 and Co-Cr, n=28), all patients who
17
agreed to participate (n=21) were included. Consequently, the patient selection in this study, which was not matched between the two groups, was not ideal when it comes to comparing the clinical performance of FDPs. The fact that all patients were treated by several dentists and dentist students, unlike some prospective studies where all FDPs were placed by one or two dentists, makes the results more representable to everyday conditions in general dentistry. After all, the idea is that all dentists should be able to handle an FDP of a certain material.
The systematic review by Tan et al (7) estimated the 10-year risks for biological (caries at abutments and loss of abutment vitality, FDP loss due to periodontitis) and technical complications (loss of retention, abutment fracture and material fractures). That study concluded that the complications with the highest risk were loss of abutment vitality (10%), caries at abutment teeth (9,5%), loss of retention (6,4%) and material fractures (3,2%). Only one FDP in either group had caries in one abutment tooth in the present study and the only technical complications were chip-off fractures of the veneering porcelain (two of the failed Ti FDPs had material fractures without information in the patients’ records about the nature of the fractures). The difference between this study and the review by Tan et al in terms of presence of biological and technical complications can be due to differences in mean service time and that Tan et al included studies on FDPs of gold acrylic or metal-ceramic design, where the latter probably is gold-porcelain.
One study has reported that prosthetic therapy can cause pulpal necrosis after several years. This study reported that 9% of the abutment teeth developed pulpal necrosis, probably due to preparation procedures during prosthetic therapy. The majority of the non-vital abutment teeth
18
developed the lesion after 7 to 12 years (15). The present study did not investigate if abutment teeth, without endodontic therapy, were vital or not.
Clinical experiments have led to the understanding that a non-vital tooth can withstand the double amount of load in comparison with a vital tooth before any experience of pain is present (16). This would mean that absence of a possible function of mechanoreceptors in the pulp, which through reflexes modulate muscular activity, would allow non-vital teeth to undergo higher load during mastication than vital teeth. An increased risk of technical
complications for FDPs with non-vital distal abutment teeth such as fracture of the FDP, loss of retention or fracture of the distal abutment teeth has been found in an epidemiological study of long-term clinical quality of FDPs (17). Two out of three fractured FDPs in the Ti group and the only fractured FDP in the Co-Cr group had one or more root filled abutment teeth.
Although the numerical difference between the two groups regarding chip-off fractures is relatively small (3 in the Ti group and 2 in the Co-Cr) the occurrence rate is higher in the Ti group. This could be due to the reason discussed about the characteristics of the different generations of ceramics used for Ti FDPs. Other possible factors affecting the occurrence of chip-off fractures is the prevalence of bruxing habits and posterior placement resulting in higher load during mastication. All of the 5 fractured FDPs had posteriorly located units but only Ti4 was placed in a patient with self-reported bruxing habits. Another study reported that 7 out of 36 Ti FDPs had fractures of the veneering porcelain and all of them occurred at posterior units during a 3-year follow up period (18). Eliasson et al found that the majority of the surface fractures of the Co-Cr FDPs occurred in patients with bruxing habits (8).
19
Direct relationships have been found between the technical failure rate and the sum of all cantilever extension pontics. The technical failure rate increased with the increasing number of cantilever extension pontics in each of the FDPs (17). Two FDPs in the Ti group had single unilateral cantilever extension pontics. One of these failed (Ti11) and the other one (Ti1) was free from technical complications.
It is evident that a majority of the FDPs in the present study had periodontitis around the abutment teeth at the examination visit. Even if this was the case, this parameter was not included when calculating the success rates for the FDPs in either group. This is a
retrospective study with no baseline examination, which makes it impossible to know whether the cause of the periodontitis is related to the FDP, or if it was present already when the FDP was placed in the patient.
When further studies are conducted with the purpose of evaluating the clinical quality and longevity of FDPs made from Ti or Co-Cr, they should be prospective with an observation time of at least 5 to 10 years and include patient acceptance values. It would be beneficial to include a control group consisting of matched patients treated with metal-ceramic FDPs made from a high-noble alloy since it is considered the golden standard (19).
20
Conclusions
The ratings of the FDPs, according to the CDA evaluations system, as well as success and survival rates showed similar results for the FDPs in both groups, with slightly better results for the Co-Cr group.
In the Ti group the complications were restricted to 5 material fractures and one carious lesion. The complications in the Co-Cr group accounted for 2 material fractures and one carious lesion contiguous with the margin of the restoration.
The success rate, survival rate and clinical quality of FDPs made from both Ti and Co-Cr was acceptable. The limited sample size necessitates, however, caution when conclusions are drawn from this study.
Acknowledgements
The authors would like to thank the staff of the Department of Oral Prosthetics, Faculty of Odontology, Malmö University for making the clinical examinations possible.
21
References
1. Bessing C. Oädla legeringar för metallkeramik: Basmetallegeringar 2007.
2. Wataha JC. Alloys for prosthodontic restorations. J Prosthet Dent. 2002; 87: 351-363.
3. Karlsson S, Nilner K, Dahl B. A textbook of fixed prosthodontics: the Scandinavian approach. Stockholm: Gothia; 2000.
4. Wang RR, Fenton A. Titanium for prosthodontic applications: a review of the literature. Quintessence Int. 1996; 27: 401-408.
5. Wataha JC. Biocompatibility of dental casting alloys: a review. J Prosthet Dent. 2000; 83: 223-234.
6. Tschernitschek H, Borchers L, Geurtsen W. Nonalloyed titanium as a bioinert metal--a review. Quintessence Int. 2005; 36: 523-530.
7. Tan K, Pjetursson BE, Lang NP, Chan ES. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004; 15: 654-666.
8. Eliasson A, Arnelund CF, Johansson A. A clinical evaluation of cobalt-chromium metal-ceramic fixed partial dentures and crowns: A three- to seven-year retrospective study. J Prosthet Dent. 2007; 98: 6-16.
9. Lövgren R, Andersson B, Carlsson GE, Odman P. Prospective clinical 5-year study of ceramic-veneered titanium restorations with the Procera system. J Prosthet Dent. 2000; 84: 514-521.
22
10. Milleding P, Haag P, Neroth B, Renz I. Two years of clinical experience with Procera titanium crowns. Int J Prosthodont. 1998; 11: 224-232.
11. Örtorp A, Ascher A, Svanborg P. A 5-year retrospective study of cobalt-chromium-based single crowns inserted in a private practice. Int J Prosthodont. 2012; 25: 480-483.
12. California Dental Association. Guidelines for the assessment of clinical quality and professional performance. 1977.
13. Gilbert JL, Covey DA, Lautenschlager EP. Bond characteristics of porcelain fused to milled titanium. Dent Mater. 1994; 10: 134-140.
14. Persson M, Bergman M. Metal-ceramic bond strength. Acta Odontol Scand. 1996; 54: 160-165.
15. Bergenholtz G, Nyman S. Endodontic complications following periodontal and prosthetic treatment of patients with advanced periodontal disease. J Periodontol. 1984; 55: 63-68.
16. Randow K, Glantz PO. On cantilever loading of vital and non-vital teeth. An experimental clinical study. Acta Odontol Scand. 1986; 44: 271-277.
17. Randow K, Glantz PO, Zoger B. Technical failures and some related clinical
complications in extensive fixed prosthodontics. An epidemiological study of long-term clinical quality. Acta Odontol Scand. 1986; 44: 241-255.
18. Boeckler AF, Lee H, Psoch A, Setz JM. Prospective observation of CAD/CAM titanium-ceramic-fixed partial dentures: 3-year follow-up. J Prosthodont. 2010; 19: 592-597.
19. Kellerhoff RK, Fischer J. In vitro fracture strength and thermal shock resistance of metal-ceramic crowns with cast and machined AuTi frameworks. J Prosthet Dent. 2007; 97: 209-215.
23
Appendix
Figure legend
24 0% 10% 20% 30% 40% 50% 60% 70% 80% 90%
Ti CoCr Ti CoCr Ti CoCr Ti CoCr
Excellent Acceptable Correct/replace Replace
Perc en ta ge o f CD A s u b ra tin gs o f each ch ar act eris tic CDA subrating
Surface and colour Anatomic form Margin integrity
25
Rating Surface and Colour Anatomic Form Margin Integrity
SA T ISFA C T O R Y Romeo
The surface of the restoration is smooth. No irritations of adjacent tissue is occuring.
There is no mismatch in colour, shade and/or transluceny between the restoration and adjacent teeth.#
Restoration contour is in functional harmony with adjacent teeth and soft tissues with good individual anatomic form.
No visible evidence of a crevice along margin into which explorer will penetrate. Satisfies operative dentistry principles of margin placement wherever possible. No discoloration on the margin between the restoration and the tooth structure.#
Sierra
- Surface is slightly rough or pitted; can be polished
- Slight mismatch in colour, shade and/or transluceny between the restoration and adjacent teeth.# - Minor surface fracture of veneering porcelain (adhesive).
- Restoration is slightly over contoured, or
- Restoration is slightly under contoured, or
- Marginal ridges are slightly undercontoured, or
- Contact is slightly open, or - Facial flattening is present, or - Lingual flattening is present, or - Anatomic form of pontic may cause food retention with no irritation to soft tissue.
- Visible evidence of slight marginal discrepany; repair can be made or is unnecessary. - Discoloration on the margin between the restoration and the tooth structure.# N O T A C C E PT A B L E Tango
- Surface is grossly irregular, not related to to anatomy and not subject to correction.
- Mismatch outside the normal range of colour, shade and/or transluceny between the restoration and adjacent teeth .#
- Moderate surface fracture of veneering porcelain (kohesive).
- Restoration is grossly over contoured, or
- Restoration is grossly under contoured, or
- Occlusion is affected, or - Contact is faulty, or
- There is marginal overhang, or - Anatomic form of pontic is likely to result in food retention causing irritation to soft tissue and/or caries in abutment teeth.
- Marginal discrepany; repair should be made.
- Retained excess cement.
Victor
- There are gross porosities in the restoration material.
- Colour, shade and/or transluceny in gross disharmony with adjacent teeth.#
- Traumatic occlusion, or - Gross under occlusion, or - Restoration causing unremitting pain in tooth or adjacent tissue.
- Mobile restoration, or - Fractured restoration, or - Caries contiguous with margin of restoration, or
- Tooth structure fractured.
Table 1. Modified criteria from the CDA evaluation system. The underlined criteria were used in
26
Participants Titanium Cobalt-chromium
Patients Mean age
(years)
FDPs Mean service
time (years)
Patients Mean age
(years) FDPs Mean service time (years) Total (n = 21) 9 59.2 13 3.1 12 59.33 12 3.9
Drop out Titanium Cobalt-chromium
Patients Mean age
(years)
FDPs Mean service
time (years)
Patients Mean age
(years) FDPs Mean service time (years) Death (n = 1) 1 - 1 - 0 - - - Declined to participate (n = 10) 6 68.33 6 - 4 45.8 6 - Failed to come to the appointment (n = 4) 0 - - - 4 54.0 4 - No response (n = 9) 4 67.3 4 - 5 50.8 5 - FDP lost or replaced (n = 4) 3 64,33 3 1,67 1 No data 1 - Total (n = 28) 14 14 14 16
Table 2. Patients and FDPs participating in the clinical examination
27 T ab le 4 . Dist ributi on of s ervic e ti me, loc ati on, a bu tm ent tee th, ca nti leve rs, root fil led te eth, pos ts and cores, ca ri es, chip -of f f ra cture s, too th we ar, br ux ing ha bit s a nd the use of a cr y li c spl int s. C hi p -off : m inor/c ohe sive c hip -off (1 ), mode ra te/a dhe sive c hip -o ff ( 2). Too th wea r: no w ea r to no rmal wea r into enamel (0) , we ar in to dent in e ( 1) . * Fa il ed. (T able ne x t pa g e)
28
FDP no. Service time Locatio
n
Abutment teeth Cantileve
r Root filled teeth Post and core Carie s Chip-off
Tooth wear, bruxing habits, splint
Ti1 3 years 11
months
13-15 14, 15 13 - - - - 1
Ti2 3 years 3 months 15-17 15, 17 - - - 0
Ti3* 8 months .11-15 11, 13, 16 - 16 16
Ti4 4 years 13-17 13, 17 - 15 - - 2 1, bruxing habits, splint
Ti5 3 years 24-26 24, 26 - - - - 2 0
Ti6 3 years 1 month 15-17 15, 17 - - - 0
Ti7 3 years 10
months
23-27 23, 24, 27 - 23, 24 - - 2 0
Ti8 2 years 4 months 14-16 14, 16 - - - 1
Ti9 3 years 3 months 12-21 12, 21 - - - 1
Ti10 2 years 13-18 13, 14, 18 - - - 0
Ti11* 2 years 6 months 22-24 22, 23 24 23 23
Ti12* 1 year 10 months 44-46 44, 46 - 46 46
Ti13 3 years 44-47 44, 47 - - - 0
Ti14 3 years 15-17 15, 17 - - - 0
Ti15 2 years 9 months 45-47 45, 47 - 17 17 - - 0
Ti16 3 years 23-26 23, 26 - - - 1, bruxing habits, splint
CoCr1 4 years 3 months 45-47 45, 47 - 47 - - - 1, bruxing habits, splint
CoCr2 4 years 10 months 11-27 11,21,22,23,26,2 7 - 21, 26 21, 26 - - 0 CoCr3 3 years 10 months 12-15 12, 13, 15 - 12 12 12 - 0 CoCr4 3 years 16-24 16, 15, 11, 23, 24 - 11 - - - 1
CoCr5 4 years 1 month 34-38 34, 35, 38 - - - 0
CoCr6 4 years 3 months 44-47 44, 47 - - - 1
CoCr7 4 years 14-17 14, 17 - - - 0 CoCr8 2 years 11 months 44-47 44, 47 - 44 44 - - 1 CoCr9 3 years 11 months 12-15 12, 15 - 12, 15 - - 2 1 CoCr10* * No data 22-25 22, 23, 25 - 23, 25 25 0
CoCr11 3 years 1 month 43-48 43, 45, 48 - - - 0
CoCr12 3 years 11
months
12-22 12, 21, 22 - - - 1, splint
29
* Criteria apply to anterior teeth.
CDA sub-ratings Titanium ceramic
(n = 13)
Cobalt chromium ceramic (n = 12)
Surface and colour
Rough or pitted surface 54 33
Surface fracture 23 17
Mismatch between
restorations and adjacent teeth (colour, shade and/or
translucency)*
15 8
No comment 8 42
Anatomic form
Over contoured 15 20
Occlusion is not totally functional
8 0
Contact is slightly open/faulty 0 20
Marginal overhang 8 0
Faulty anatomy of pontic 46 40
No comment 23 20
Margin integrity
Marginal discrepancy 15 0,3333
Caries contiguous with margin 0 0,0833
No comment 85 0,5833
FDP no. Service time Reason for failure
Ti3 8 months Fractured corner of tooth 11
Ti11 2 years 6 months Fractured buccal cusp of tooth 24
Ti12 1 year 10 months Loss of retention due to caries
CoCr10 No data No data
Table 5. Reasons for suboptimal rating (in %) for the Ti and Co-Cr metal-ceramic FDPs