DEY AR MAHMOOD MALMÖ UNIVERSIT ON C ORE AND BI-L A YERED ALL -CER AMIC FIXED DENT AL PR OS THESES, DESIGN AND MEC HANIC AL PR OPERTIES DOCT OR AL DISSERT A TION IN ODONT OL OG Y
DEYAR JALLAL HADI
MAHMOOD
ON CORE AND BI-LAYERED
ALL-CERAMIC FIXED DENTAL
PROSTHESES, DESIGN AND
MECHANICAL PROPERTIES
O N C O R E A N D B I - L A Y E R E D A L L - C E R A M I C F I X E D D E N T A L P R O S T H E S E S , D E S I G N A N D M E C H A N I C A L P R O P E R T I E S
Malmö University
Faculty of Odontology Doctoral Dissertations 2015
© Deyar Jallal Hadi Mahmood, 2015
Photographs and illustrations: Deyar Jallal Hadi Mahmood ISBN 978-91-7104-405-1 (print)
ISBN 978-91-7104-406-8 (pdf) Holmbergs, Malmö 2015
DEYAR JALLAL HADI MAHMOOD
ON CORE AND BI-LAYERED
ALL-CERAMIC FIXED DENTAL
PROSTHESES, DESIGN AND
MECHANICAL PROPERTIES
Malmö University, 2015
Department of Prosthetic Dentistry
Faculty of Odontology
Malmö, Sweden
Studies on stabilized zirconiumdioxide
This publication is also available in electronic format at: http://dspace.mah.se/handle/2043/18473
To my entire family.
Acquire knowledge, and learn tranquility and dignity Umar ibn al-Khattab
TABLE OF CONTENTS
LIST OF PUBLICATIONS ... 11
THESIS AT A GLANCE ... 12
ABSTRACT ... 13
POPULÄRVETENSKAPLIG SAMMANFATTNING ... 15
ABBREVIATIONS AND DEFINITIONS ... 18
INTRODUCTION ... 19
Treatment planning (Clinical application of dental ceramics) ...19
Dental Ceramics ...20
Ceramic classification ...20
Dental glass-based/porcelain systems ...21
Glass ceramics ...21
Glass-infiltrated oxide-ceramics (hybride-ceramics) ...23
Oxide ceramics ...23
Stabilized Zirconium Dioxide ...23
Manufacturing Procedure ...25
CAD/CAM ...26
Effects of the design of all-ceramic dental restorations and in-vitro test setup ...27
FDP core design ...27
In-vitro test setup for all-ceramic FDPs ...28
Follow up and maintenance of dental ceramic restorations ...29
What do we know today? Final remarks ...30
AIMS ... 31
MATERIALS AND METHODS ... 33 Laboratory Procedures ...33 Study I ...33 Study II ...38 Study III ...40 Study IV ...42 RESULTS ... 51 Study I ...51 Study II ...53 Study III ...55 Study IV ...56 Statistical Analyses ...61 DISCUSSION ... 62
Methods: In-vitro studies and test setup ...62
Choice of specimen design ...62
CAD/CAM system ...63
Veneer Techniques ...65
Supporting tooth analogues ...65
Cementation and water storage ...66
Artificial aging (heat treatment, thermocycling, mechanical preload) ...67
Load-to-fracture ...68
Discussion of results ...69
Intraoral loads and mechanical preload...69
FDP design ...70
The connector/radius ...70
Milling dental ceramics ...74
LTD ...75
Veneering techniques and fractures ...76
Veneer failure predictions ...79
Multifaceted factors ...79
Thermal stresses ...79
Inappropriate veneering thickness ...80
Defects in the veneering material ...81
Multifaceted bond failure ...81
Fracture mode analyse ...82 Clinical significance ...83 Future investigations ...83 CONCLUSIONS ... 85 ACKNOWLEDGEMENTS ... 87 REFERENCES ... 89 PAPERS I – IV ...103
LIST OF PUBLICATIONS
This thesis is based on the following articles, which will be referred to in the text by their Roman numerals. The articles are appended at the end of the thesis.
I. Bahat Z, Mahmood DJ, Vult von Steyern P. Fracture
strength of three-unit fixed partial denture cores (Y-TZP) with different connector dimension and design. Swed Dent J 2009;33:149-159.
II. Mahmood DJ, Linderoth EH, Vult Von Steyern P. The influence
of support properties and complexity on fracture strength and fracture mode of all-ceramic fixed dental prostheses. Acta Odontol Scand. 2011 Jul;69(4):229-37.
III. Mahmood DJ, Linderoth EH, Vult von Steyern P, Wennerberg A. Fracture strength of all-ceramic (Y-TZP) three- and four-unit fixed dental prostheses with different connector design and production history. Swed Dent J 2013;37, 4:179-187.
IV. Mahmood DJ, Linderoth EH, Wennerberg A, Vult von Steyern P.
Influence of core design, production technique and material selection on fracture behavior of Y-TZP FDPs produced using different multi-layer techniques: split-file, over-pressing and manually built-up veneers. Submitted.
THESIS A T A GL AN CE Study Aim Met hods Illus tr ation Main F indings
I: Fracture strength of three- unit fixed par
tial dental cores (Y -TZP) with different co nn ec tor d im en si on an d design.
Evaluate the effect of various connector dimensions and whether different radii of cur
vature in the
embrasure area of the connector could affect the fracture strength of three-unit all-ceramic fixed dental prostheses (FDPs) made of Y
-TZP
.
48 three-unit FDPs with Y
-TZP
frameworks with three connector dimensions var
ying from 2.0
mm to 3.0 mm and two radii of gingival embrasure, 0.6 mm and 0.9 mm.
CAD design there-unit FDP
Fracture strength was significantly higher with each increase in connector dimension. Increasing the radius of the gingival embrasure from 0.6 mm to 0.9 mm in the 3 mm × 3 mm connector group increased fracture strength by 20%.
II: Influence of suppor
t pr op er tie s a nd co m pl ex ity
on fracture strength and fracture mode of all-ceramic fixed dental prostheses. Evaluate the effect of various tooth analogues used for
in-vitro
studies
and how these influence test results relating to the fracture strength of FDPs made of Y
-TZP
.
24 three-unit FDPs with Y
-TZP
frameworks, tested on three types of tooth-suppor
ting analogue ma de fro m a lum inu m, pol yme r, or DuraLay . Aluminum with Y -TZP fracture
There should be a standardized, simple test set-up when
in-vitro
testing all-ceramic
FDPs. T
ooth analogues with high E-modulus
gave high and unrealistic load-at-fracture values together with adverse fracture modes compared to FDPs involved in clinical failure.
III: Fracture strength of all-ceramic (Y
-TZP) three-
and four
-unit fixed dental
prostheses with different connector design and production histor
y.
Evaluate different CAD/CAM systems and compare core designs, increasing the length of the FDPs (i.e. the number of pontics) to deter
mine how this
affects the fracture strength of all-ceramic FDPs made from Y
-TZP
.
16 three-unit and 16 four
-unit
FDPs with Y
-TZP frameworks
and var
ying connector designs
generated by a mechanical scanner or a laser displacement gauge scanner
.
Four
-unit Y
-TZP
Default settings of the various CAD/CAM systems had a great impact on fracture strength. A crucial factor for load-bearing capacity is the design of the radius of the gingival embrasures. Increasing the number of pontics from three to four decreases the load-bearing capacity by nearly half.
IV: The influence of core design, production technique and material selection on fracture behavior of Y
-TZP FDPs
produced with different multi-layer techniques; spli
t-f ile, o ver -pr ess in g an d
manually built-up veneers.
Evaluate the effect of various veneering materials, techniques, and core designs with respect to the fracture strength and fracture mode of currently used multilayer all-ceramic Y
-TZP . 110 three-unit Y -TZP FD Ps wi th two fra me wo rk des ig ns:
40 with layered veneering 30 with milled veneering 10 with pressed veneering 30 w
ith c or e d es ig ns g en era te d
by two different CAD/CAM systems.
Fracture patter
n
The design of a framework is a crucial factor for the load bearing capacity
. The
state-of-the-ar
t design are preferable since the
split-file designed cores call for a cross-sectional connector area, at least 42% larger
, to have
the same load bearing capacity
. Analysis
of the fracture patter
n shows differences
between the milled veneers and over
-pressed
ABSTRACT
Loss of teeth can affect a person’s self-esteem, social life, appearance and oral function. Reconstruction of a missing tooth has scientifically been shown to increase self-esteem and quality of life and to maintain oral function. For many patients a fixed dental prostheses (FDP) is preferred, either tooth- or implant-supported. Improvement and development of all-ceramic materials have made them preferable to other alternatives. However, despite properties of dental ceramics’ well known biocompatibility, good chemical and mechanical, the materials have their weaknesses, such as brittleness and some difficulties with the layering porcelain. Many all-ceramic materials cannot withstand minor flexure; more than 0.1 - 0.3 %, will lead to fracture. Oxide-ceramic, specifically yttria stabilized tetragonal zirconia polycrystals (Y-TZP) has become the most commonly used all-ceramic material. This material has the potential to be used for larger restorations. In addition, one of many challenges is to ensure durable zirconia-based restorations in the oral cavity.
In the clinical situation, crowns and bridges are supported by a combination of different structures with differing properties, i.e. bone, dentine and enamel. The complexity of the supporting tissues in the oral cavity creates stress patterns in the prosthetic material, which need to be considered when designing a dental restoration.
The durability of all-ceramic FDPs is dependent on knowledge of the material and design of the FDPs. In particular the design, shape of the connector and the radius of curvature at the gingival embrasure play a significant role in the load-bearing capacity of FDPs.
The overall aim of this thesis is to evaluate design of zirconia-based restorations in relation to achieving increased fracture resistance. Another aim is related to how the choice of material used for supporting tooth analogues in the test set-up and how this influences test results relating to fracture strength of all-ceramic FDPs.
Study I evaluates different radii (0.60 and 0.90 mm) of curvature in the embrasure of the connector area and different connector dimensions (2 x 2, 3 x 2 and 3 x 3 mm) and their effects on the
fracture resistance of 3-unit all-ceramic FPDs made of Y-TZP. The results show that by increasing the radius of the gingival embrasure from 0.6 to 0.9 mm, the fracture strength for a Y-TZP FPD with connector dimension 3 x 3 mm will increase by 20%.
Study II investigated how the choice of material (aluminium, polymer and DuraLay) used for supporting tooth analogues and support complexity influence test results concerning the fracture strength of FDPs made of a brittle material Y-TZP. The outcome of the study demonstrated that Y-TZP FDPs cemented on tooth analogues made of aluminium, with high E-modulus showed a significantly higher load at fracture and a different fracture mode than shown in clinical situations.
Study III evaluates how factors as different default settings for connector design of two different CAD/CAM systems and different radii of curvature in the embrasure area of the connector will affect the fracture strength and the fracture mode of 3-unit, i.e. 4-unit all-ceramic FDPs made from Y-TZP and further to investigate how the number of pontics affect the fracture strength of Y-TZP. The results showed that the most crucial factor for the load-bearing capacity is the design of the radius of the gingival embrasures. Increasing the number of pontics from three to four decreases the load-bearing capacity nearly twice.
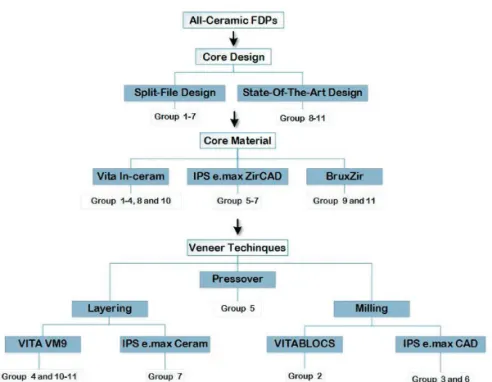
Study IV investigate and compare the fracture strength and fracture mode in 11 groups of the currently most used multilayer all-ceramic systems for Y-TZP FDPs, with respect to the choice of core material, veneering material area, manufacturing technique (split-file, over-press, built-up porcelains and glass-ceramics), design of connectors and radius of curvature of FDP cores. The results show that the design of a framework is a crucial factor for the load bearing capacity of an all-ceramic FDP. The state-of-the-art designs are preferable, since the split-file designed cores call for a cross-sectional connector area, at least 42% larger, to have the same load bearing capacity as the state-of-the-art designed cores. Analyses of the fracture patterns demonstrated differences between the milled veneers and over-pressed or built-up veneers, where the milled ones showed numerically more veneer cracks whereas the other groups only showed complete connector fractures. All veneering materials/techniques tested were found, with great safety margin to be sufficient for clinical use both anteriorly and posteriorly.
POPULÄRVETENSKAPLIG
SAMMANFATTNING
Förlust av tänder kan påverka en persons självkänsla, sociala liv, utseende och orala funktion. Rekonstruktion av en saknad tand har vetenskapligt visat en ökning av självkänsla, livskvalitet och upprätthållande av orala funktioner. För många patienter är en fastsittande konstruktion förstahandsvalet; alternativen är antingen en tandburen eller en implantatstödd tandprotes. Utveckling av helkeramiska material har medfört att protetiska konstruktioner av helkeramisk typ har allt mer blivit tandvårdsteamets förstahandsval. Dentala keramer har, utöver de estetiska fördelarna, flera kemiska och mekaniska egenskaper som talar till deras fördel, men materialen är spröda. Många helkeramiska material är mycket känsliga för böjning; en påkänning större än 0.1 - 0.3%, leder till fraktur. Oxidkeramer, såsom yttriumdioxid-stabiliserad tetragonal polykristallin zirkoniumdioxid (Y-TZP) har ökat i användning och är det vanligaste helkeramiska materialet. Detta material har potential att användas för större tandersättningskonstruktioner. En av många utmaningar är att framställa hållbara, zirconiabaserade tandersättningskonstruktioner. I den kliniska situationen stöds tandersättningskonstruktioner, såsom kronor och broar, av en kombination av olika vävnadstrukturer; käkben, dentin och emalj, med olika mekaniska egenskaper. Komplexiteten hos de stödjande vävnaderna i munhålan skapar spänningsmönster i de dentala materialen, vilket måste beaktas när man designar dentala rekonstruktioner. Hållfastheten hos helkeramiska rekonstruktioner
avgörs av dess utformning. Vid design av en brokonstruktion bör särskild vikt läggas vid utformningen av de sammanfogandes balkarna (connectorområdena) och dess krökningsradie vid balkövergångarna, vilken har en avgörande roll för brokonstruktionens bärande förmåga.
Det övergripande målet med föreliggande avhandlingsarbete var att utvärdera hur zirkoniumdioxidbaserade brokonstruktioner bör designas för ökad hållfasthet. Därutöver var syftet att undersöka hur valet av tandanalogsmaterial som används vid laboratorietest och deras utformning, påverkar resultaten avseende hållfasthetvärden och frakturmönster vid mekaniska test av keramiska brokonstruktioner. Delarbete I utvärderade hur brotthållfastheten hos helkeramiska 3-leds broar, utförda i zirkoniumdioxid påverkas av förändringar i connectorns gingivala radie (0,60 respektive 0,90 mm) samt connectorns dimension (2 x 2, 3 x 2 och 3 x 3 mm). Resultaten visar att genom att öka radien på den gingivala övergången från 0,6 till 0,9 mm, ökar brotthållfastheten med 20 % för 3-leds broar i Y-TZP där connectordimenisonen var 3 x 3 mm.
Delarbete II utvärderade hur valet av material för, och utform-ningen, av tandanaloger avsedda för laboratorietest påverkar resul-tatet avseende hållfasthetvärden och frakturmönster vid mekaniska test av brokonstruktioner i Y-TZP. Resultatet av studien visar att brokonstruktioner cementerade på tandanaloger av material med hög E-modul visade en signifikant högre hållfasthetsvärde, samt att frakturmönstret är av en annan typ än det som erhålls vid kliniska frakturer.
Delarbete III utvärderade hur grundinställningarna avseende connectordesign i två olika CAD/CAM-system påverkar hållfastheten, samt hur en ökad längd på brobalken (dvs. antalet pontics) påverkar brotthållfastheten hos helkeramiska brokonstruktioner tillverkade av Y-TZP. Resultaten visar att den mest avgörande faktorn för brohållfasthet är utformningen av, och radien på, connectorns gingival övergång. En ökning av antalet led (pontics) från tre till fyra minskar brotthållfasthetens med nära hälften.
Delarbete IV utvärderade och jämförde brotthållfastheten hos 3-leds broar med Y-TZP som kärnmaterial. 11 grupper med design och ytkeramer av de vanligast förekommande typerna testades avseende betydelsen av faktorer som connectordesign och gingival radie hos
broskelettet samt val av ytkeram och framställningsteknik (fräst, över-pressad, handupplagt porslin). Resultat visade att designen av en brokonstruktion är en avgörande faktor för brotthållfastheten hos en helkeramisk bro. State-of-the-art design är att föredra framför split-file design, som behöver en 42% större connectorarea för att likvärdig brotthållfasthet som state-of-the-art designen uppvisar ska erhållas. Analysen av frakturmönster visar skillnader mellan fräst ytkeram och pressad eller handupplagd ytkeram. Grupperna med frästa ytkeramer uppvisade frakturer i ytkeramen, medan övriga grupper bara uppvisade totalfrakturer. Alla ytkeramiska material/ metoder som testades visade stor säkerhetsmarginal som är tillräcklig för den kliniska användet i den orala miljön.
ABBREVIATIONS AND DEFINITIONS
Alumina Aluminum oxide
CAD Computer-aided design
CAM Computer-aided manufacturing
CIP Cold isostatic pressing
E-modulus Elastic modulus
FDP Fixed dental prostheses
HIP Hot isostatic pressing
LTD Low temperature degradation
MDP 10-Methacryloyloxydecyl dihydrogen phosphate
MPa Mega Pascal
N Newton
POM-C Polyoxymethylene-copolymer
(m) Stable monoclinic-phase
TC Thermocycling
(t) Tetragonal-phase
Y-TZP Yttria stabilized tetragonal zirconia polycrystals
Yttria Yttrium oxide
INTRODUCTION
Loss of teeth can affect a person’s self-esteem, social life, appearance and oral function. According to the WHO’s criteria (2001), tooth loss is a physical impairment because it constitutes loss of important parts of the body (1). Reconstruction of a missing tooth has been scientifically shown to increase self-esteem and quality of life and to maintain oral function (2). The dental team has many options concerning restoration production technique and materials in order to fulfil the patient’s need for aesthetic, functional, long-lasting, and biocompatible restorations. Many patients prefer fixed dental prostheses (FDPs), either tooth- or implant-supported (3).
Treatment planning (Clinical application of dental ceramics)
In recent years all-ceramic restorations have increased in popularity because ceramic is an aesthetic and biocompatible material. There is a growing tendency toward replacing metal-based restorations in the posterior and anterior region with all-ceramic materials. Development and improvement of high-strength ceramics and new manufacturing processes have led dental teams to prefer all-ceramic materials for FDP treatment. The success of restorations not only depends on the material selected but also involves personal preferences and prevailing clinical conditions such as tooth preparation, caries, endodontic problems, and the choice of cementation technique (4-6). To avoid stress concentrations, the tooth preparation and the restoration should have smooth, rounded contours. However, the cement-space required between the tooth substance and the FDP material can affect the functionality and quality of the remaining tooth substance.The durability of all-ceramic FDPs depends on clinicians and dental technicians knowledge of the material and design of the FDPs (7). In particular, the design, the shape of the connector, and the radius of the curvature at the gingival embrasure play a significant role in the load-bearing capacity of FDPs (8-11). In clinical situations, crowns and bridges receive support from a combination of different structures with differing E-modulus properties such as bone, dentin, and enamel. The complexity of the supporting tissues in the oral cavity leads to stress patterns that the design of the test setup for an
in-vitro study should take into consideration (11, 12).
Dental Ceramics
All-ceramic materials have strong covalent and ionic interatomic bonds. They are well-known for their high E-modulus, wear resistance, hardness, and melting temperature, as well as their low thermal expansion coefficient and electrical conductivity. Furthermore, some studies have demonstrated that all-ceramic materials accumulate less plaque than acrylic materials (13-15). All-ceramic materials are more tooth-like than metal-based restorations and have optical properties similar to that of enamel and dentin.
Despite dental ceramic’s well-known biocompatibility and good chemical and mechanical properties, the materials have their weaknesses, such as brittleness. Many all-ceramic materials cannot withstand flexure; more than 0.1–0.3% will lead to fracture. Furthermore, the materials are strong when compressed but weak under tension (16, 17). Another disadvantage of ceramic materials is their vulnerability to flaws or defects in manufacturing related to mechanical, chemical, or thermal processing. Under load, the flaws and the defects can act as a starting point for fracture; a localized concentration of stress will break the atomic bonds and propagate a crack that, if not hindered, will affect the strength of the construction and may cause a complete fracture (18-22).
Ceramic classification
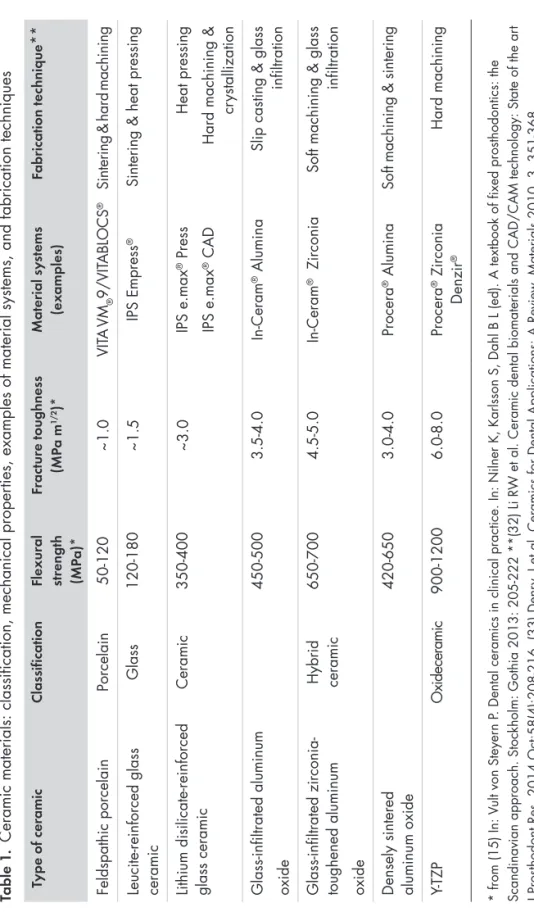
In recent years many types of ceramic systems have been introduced in dentistry for all kinds of restoration. Dental ceramics may
be classified in a variety of ways based on their intended use, chemical composition, processing method, sintering temperature, microstructure, translucency, fracture resistance, and abrasiveness (23-25). Additionally, the International Organization for Standardization (ISO), ISO 6872:2008 Dentistry – Ceramic Materials (26), lists other classifications: ceramic products that are provided from powder (Type I), and all other forms of ceramic products (Type II) (27). This thesis classifies dental ceramics according to their chemical composition and their intended use (Table 1).
Dental glass-based/porcelain systems
Dental glass-based and porcelain systems consist mainly of silicon dioxide (silica or quartz) and varying amounts of alumina (or aluminum oxide). These systems also employ feldspars that are mainly made of aluminosilicates found in nature. They contain various amounts of potassium and sodium. Their main application is for aesthetically important areas, monolithic restorations (veneers), or as veneering with strong optical properties (16). They have disadvantages, such as limited strength, but their strength can be increased significantly by etching and use of a resin bonding (28).
Glass ceramics
The composition of glass ceramics is similar to that of the porcelain category above. The difference is in the modification process in which varying amounts of different types of crystals are either added or grown in the glass matrix. The primary crystal types available today are leucite, lithium disilicate, and fluorapatite. Dental porcelain and ceramics with high glass content include veneers for monolithic all-ceramic and metal frameworks. They can be used as anterior veneer restorations (e.g., as laminate veneers), in crowns, and in the rest of the mouth as onlays and inlays. Glass ceramic made from fluorapatite and litthium disilicate have been subject of several improvements; from layering glass ceramics to molded pressable ceramics and from the lost wax method to machine-milled ceramics. Those materials are used in full monolithic restorations in any region of the mouth, such as crown, inlays, onlays, veneers and FDPs up to premolar region (29-31).
Table 1
.
Ceramic materials: classification, mechanical proper
ties, examples of material systems, and fabrication techniques
T ype of cer amic Classif ication Flexur al str engt h (MP a)* Fr actur e t oughness (MP a m 1/2 )* Material sy stems (ex am ples) Fabrication tec hniq ue ** Feldspathic porcelain Porcelain 50-120 ~1.0 VIT A VM ® 9/VIT ABLOCS ®
Sintering & hard machining
Leucite-reinforced glass ceramic
Glass
120-180
~1.5
IPS Empress
®
Sintering & heat pressing
Lithium disilicate-reinforced glass ceramic
Ceramic 350-400 ~3.0 IPS e.max ® Press IPS e.max ® CAD Heat pressing
Hard machining &
cr
ystallization
Glass-infiltrated aluminum oxide
450-500
3.5-4.0
In-Ceram
® Alumina
Slip casting & glass
infiltration
Glass-infiltrated zirconia- toughened aluminum oxide Hybrid ceramic
650-700
4.5-5.0
In-Ceram
® Zirconia
Soft machining & glass
infiltration
Densely sintered aluminum oxide
420-650
3.0-4.0
Procera
® Alumina
Soft machining & sintering
Y-TZP O xi de ce ra m ic 900-1200 6.0-8.0 Procera ® Zirconia Denzir ® Hard machining * from (15) In: V
ult von Steyer
n P
. Dental ceramics in clinical practice. In: Nilner K, Karlsson S, Dahl B L (ed). A textbook of fixed prosthodontics: the
Scandinavian approach. Stockholm: Gothia 2013: 205-222 **(32) Li R
W et al. Ceramic dental biomaterials and CAD/CAM technology: State of the ar
t
J Prosthodont Res. 2014 Oct;58(4):208-216. (33) Denr
y, I et al. Ceramics for Dental Applications: A Review
Glass-infiltrated oxide-ceramics (hybride-ceramics)
Interpenetrating phase ceramics were introduced in the early 1990s. This system consists of partly-sintered alumina or zirconia cores, reinforced by a glass infiltration technique and subsequently veneered with specially developed porcelain to give the restoration the desired aesthetic properties. Its main use is for single crowns and three-unit FDPs (34, 35). Because this technique is sensitive and its manufacturing time consuming, use of this group of ceramics has decreased while use of lithium disilicate glass ceramic and oxide ceramics has increased (36).
Oxide ceramics
Polycrystalline ceramics, also known as high-strength oxide ceramics, have no glass phase and are acid resistant. The two main oxide ceramics in dentistry are densely sintered aluminum oxide and yttria-stabilized tetragonal zirconia polycrystals (Y-TZP), sometimes described as “ceramic steel”. Due to their outstanding biocompatibility, mechanical properties, and relative translucency, these materials have become more commonly used (37, 38). It could be said that Y-TZP has replaced aluminum oxide as the dominant all-ceramic core material for FDPs. As a substructure material, Y-TZP is used with a veneer material consisting of porcelain or glass ceramics that can be produced using layering or pressable ceramics, or by computer-aided design and computer-aided manufacturing (CAD/CAM). Their range of use is wide: orthodontic brackets, endodontic posts/dowels, veneers, crowns, FDPs, and implant abutments (36, 39-41). New research on stabilized zirconia has developed more translucent forms of the material to achieve more aesthetic monolithic restorations (42, 43).
Stabilized Zirconium Dioxide
Y-TZP was introduced into dentistry in the 1990s. Pure
zirconium-dioxide (ZrO2, zirconia), is a metal oxide that was first identified
in 1789 (44). In nature, zirconia is polymorphic, meaning that it displays a different equilibrium (stable) crystal structure at different temperatures with no change in chemistry. It exists in three crystalline phases: above 2370 °C, zirconia forms a cubic solid solution; at intermediate temperatures between 2370 °C and
1170 °C, the material transforms into a solid solution of tetragonal microstructure; and below 1170°C, it changes to a monoclinic structure. During cooling, this material undergoes a change in crystal structure; it transforms from a tetragonal to a monoclinic structure. This results in a volume increase in the range of 3–5%. The volume increase induces stress within the material and may initiate crack formation. This makes pure zirconia unsuitable at room temperature for structural or mechanical use. Spontaneous crack formation can occur within the material (32, 44).
It is possible to decrease or eliminate these crystal-structure changes by adding one of several oxides that dissolve within the crystal
structure of zirconia. Such oxides include yttrium oxide (Y2O3),
cerium oxide (Ce2O3), calcium oxide (CaO), or magnesium oxide
(MgO), known as stabilizers. These oxides dissolve within the crystal structure of zirconia and make it possible to densify the material in the tetragonal-phase-range to yield a fine-grained microstructure consisting almost completely of tetragonal grains that is metastable at room temperature (stabilized zirconia) (45-47). The transformation of tetragonal-stabilized zirconia into a monoclinic structure is influenced by temperature, vapor, particle size, the micro- and macrostructure of the material, and the concentration of stabilizing oxides. The most common zirconium dioxide in dentistry is stabilized with 3 mol% yttrium oxide (3Y-TZP). With its mechanical properties such as flexural strength (between 900 and 1200 MPa) and fracture toughness (6–10 MPa/m1/2) it is the dental ceramic considered to have the best mechanical properties (Table 1) (44, 48).
Microcracks, flaws, and defects that inherently grow during the thermal and mechanical processes of manufacturing may significantly influence the fracture resistance of dental ceramics (49). Flaws and defects embedded in the material have the potential to crack under local stress. When a crack occurs, each tetragonal grain has the potential to transform into a monoclinic phase. This causes a local increase in crystal volume of about 3–5%, which inhibits or delays further crack propagation (50, 51). This mechanism is known as transformation toughening; it is a one-way progression that gives the material great potential for stress-bearing and wear-resistant applications (25, 52).
The strength and structural stability of Y-TZP can also be affected by exposure to fluids such as saliva, water, and steam sterilization, or via microcracks caused by mechanical treatments such as grinding or airborne-particle abrasion. Metastasized zirconia ceramics may spontaneously transform from tetragonal to monoclinic phase, which is known as low temperature degradation (LTD) (53-55). Fluids such as saliva may penetrate the surface into the material, breaking the bonds between the atoms and leading to an increase in volume that stresses the particles and results in subcritical crack growth (56). Several factors influence the LTD behaviour of stabilized-zirconia ceramics, including grain size distribution; phase composition; stabilizer distribution; and sintering conditions such as sintering time, temperature, and atmosphere (55, 57, 58). Compared with other dental ceramic materials, Y-TZP is more opaque. To achieve a more aesthetic Y-TZP restoration, the core material is covered with veneering porcelain. The most significant sources that hinder the translucency of Y-TZP are the grain boundaries and pores (43). Changes in the amount and size of the crystals and pores, as well as in the sintering process, have made the material increasingly translucent (59-61). Translucent Y-TZP is currently designed for use as full anatomical constructions. These monolithic constructions are characterized by painted stains on the surface, or used with different degrees of cut-back in the labial/buccal areas that are then layered with porcelain to achieve better aesthetics.
Manufacturing Procedure
The same set of manufacturers produce almost all zirconia raw materials, but quality varies depending on the type of powder granulometry and the compaction production process used for the discs and blocks. These will determine the final microstructure. There are three ways to compress zirconia powder to increase the density of a ceramic body: uniaxial pressing, cold isostatic pressing (CIP), and hot isostatic pressing (HIP). When using the uniaxial press technique, the powder is pressed in one direction, yielding a green body with low density that is most likely to contain inherent stresses (60, 62, 63). The isostatic methods of compression involve pressure from all directions through a liquid or gaseous medium surrounding the compacted part, yielding a more homogenously packed material with higher density and fewer pores and voids. CIP is conducted at room
temperature by one of two techniques: wet bag or dry bag. In the wet bag method, the mold is enclosed with powder, placed in a container filled with liquid, and put under pressure. In the dry bag method, the mold is an integral part of the container and compression uses very little liquid. HIP combines pressing and sintering at increased
temperature (1400–1500oC) under high pressure in a gas atmosphere,
yielding a dense material of up to 99% density. The diffusion process improves densification, healing voids and pores (63). Previous studies also report that zirconia produced by HIP is less sensitive to LTD (64). The first step of the fabrication process is the manufacture of a block or blanks, which can be made from a huge number of ceramics, using one of these methods (32).
CAD/CAM
It is possible to produce blanks and blocks made from stabilized zirconia using a subtractive technique in a CAD/CAM system, either by soft or hard machining. Soft machining includes two different blanks: green stage which is pressed only, or white stage where the powder is pressed and partially sintered. The presintered blanks are easy to shape. The restoration is milled out in a framework enlarged by approximately 20-25%. To achieve the final dimensions and maximal strength, the restoration must be sintered after milling (32, 65, 66). Hard machining involves the milling out of fully sintered blanks that are pressed and completely sintered before milling. Its high hardness requires long milling times and causes rapid wear of the machining tools. Surfaces of dental ceramics machined by hard or soft machining and adjustment grinding show extensive formation of deep defects, microcracking with grain refinement, and deep machining grooves. These factors will decrease the strength of the material (67, 68).
Several CAD/CAM systems are available on the market. The majority use presintered blocks or blanks. The introduction and development of CAD/CAM systems has influenced the production of prosthetic reconstructions, and today this technique is dominant. The introduction of CAD/CAM has made it possible to produce all-ceramic FPDs not only with a higher degree of purity and better aesthetics, but also with a high degree of accuracy (32, 65, 66). In each system, the design is more or less dependent on the design
limitations of the CAD software and the milling properties of the CAM system. Many of the design parameters can be individually adjusted to fit each case, while other systems have fixed default settings determined by the manufacturers before milling (69).
Effects of the design of all-ceramic dental restorations
and in-vitro test setup
FDP core design
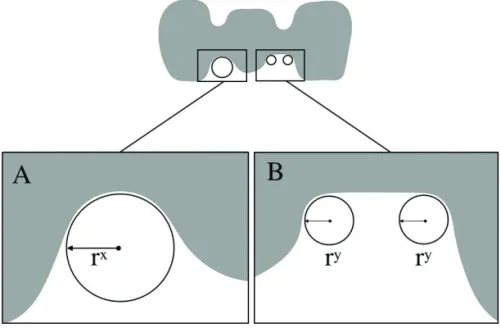
The design of crowns and bridges has a great impact on the clinical performance of all-ceramic restorations. Complete fracture through both veneer and core can occur. The design possibilities for an FDP may be limited because of the default settings of CAD/CAM systems and may depend on limitations in the CAD software. In-vitro tests and finite element analyses (FEA) have shown that concentrations of stress occur in the connector of all-ceramic FDPs (46, 70, 71). The dimensions of FDP connectors must be large enough to counteract the concentrations of stress that develop in the framework at the intersection of the pontics. The most important factor seems to be connector diameter, but the radius of curvature at their intersection may also be important (Figure 1) (72, 73). In the CAD software, connector dimensions can be set as either occlusal-gingival height
(mm) × buccal-lingual width (mm) or as a cross-section (mm2). In
this thesis, all frameworks were designed with connector dimensions set as height × width. Longer spans with several pontics have shown decreasing fracture strength in all-ceramic FDPs (74, 75). Veneer thickness can influence the concentration of stress in an FDP, leading to veneer fractures. To reduce the incidence of veneer fracture or chipping, FDP cores should incorporate anatomical designs, making an even veneer thickness possible (16, 76, 77). In-vitro studies have investigated the fracture strength and fracture mode of stabilized-zirconia FDPs using different shapes and sizes of connectors. A small radius with a design of its own, connected with a straight beam, has been shown to reduce the strength of all-ceramic FDPs (78, 79). However, in-vitro studies have used different testing methods, which affects comparability (80-82).
Several studies have explored the optimal design for all-ceramic stabilized zirconia FDP cores. They have suggested that the app-ropriate shape and dimensions for FDPs should include the following:
a minimum core thickness of 0.7 mm (36, 83); an overall smooth, rounded, and anatomically shaped core that allows and supports an even layer of veneering material 0.8–2.0 mm thick (16, 84, 85); connector dimensions of at least 3 mm × 3 mm; and U-shaped gingival embrasure areas, preferably with a radius of at least 0.90 mm (11, 86, 87). This design is widely accepted and is currently considered to be the state-of-the-art design for Y-TZP FDPs.
Figure 1 (a and b). Two connector designs of the gingival embrasure, where
rx and ry represent the radius of the curvature of the gingival embrasure:
(a) The gingival embrasure has a smooth, round, large radius; (b) The curvature of the width of the gingival embrasure has a smaller radius.
In-vitro test setup for all-ceramic FDPs
New materials on the commercial market need to be tested before clinical use to ensure patient safety. An in-vitro test setup can be made in many different ways and the purpose of in-vitro tests is often to determine the specific properties of a material (88). When testing ceramic materials, the test methods must take into account the range and distribution of forces with consideration for the brittle nature of the material (22, 89). Because tensile strength and fracture toughness can be tested in various ways, several test methods are available
depending on the material to be tested. Mechanical tests can be performed with various samples of test specimens including beams, discs, or norm crowns, for example (90-92). When evaluating the material and design of dental reconstructions, their geometry must be considered (82, 93-95). This requires extra effort in designing the framework in an in-vitro study to reproduce the complexity of the supporting systems in the oral cavity that create stress patterns in the FDP (94, 96). In-vitro studies should mimic patient-related factors such as supporting bone, periodontal ligament, abutment teeth with varying root anatomies, and dentin cores of different shapes and quality as nearly as possible (96, 97). Furthermore, in-vitro studies should also consider environmental factors such as moisture, repeated loads, support, and temperature changes, particularly for a complex construction like an FDP (98-100). In-vitro testing can use tooth analogues as abutments. Several tooth analogues have been used in various publications. Examples include cast metals, prefabricated analogues (CAD/CAM), and various kinds of resins (37, 79, 101-103). Extracted human or bovine teeth have also been used (81, 104, 105). The choice of tooth analogues can affect the fracture strength of all-ceramic FDPs. Using rigidly supported tooth analogues may hinder the movement of the abutment teeth. In this case, the load-bearing capacity of the FDPs tested will probably increase and consequently affect the result, giving unrealistic fracture data (96, 97, 106). By comparison, a study design that takes into consideration the supporting tissues, dentin cores, periodontal ligament, and cortical bone may produce decreased load-at-fracture values (96, 97, 105, 107).
Follow up and maintenance of dental ceramic restorations
Correct diagnosis and prognosis of the intraoral situation is very important to the clinical outcome of ceramic supraconstructions. Despite the advantages of stabilized zirconia, there are weaknesses associated with the material that need to be improved, especially for their FDP application. Several clinical studies report that fractures occur in the connector of Y-TZP-based FDPs. The most commonly reported problem with Y-TZP FDPs covered by hand-layered veneer is chipping of the veneer (108-112). To overcome these complications associated with chip-off fractures, improvements in the mechanicalproperties of Y-TZP veneers have achieved comparable mechanical properties to veneers used for metal-ceramic FDPs (86, 113). Several other solutions have been developed, such as the overpressing technique and milling out of the veneer using CAD/CAM technology (97, 114, 115). In the case of chipping failure, this can be repaired using bonding techniques and polishing the surface. Major chipping or connector fractures may require complete replacement of the FDP.
What do we know today? Final remarks
The use of stabilized zirconia restorations has increased, but many improvements are still needed. To achieve acceptable long-term clinical survival of stabilized zirconia restorations, we need more knowledge about design and how to increase fracture resistance. Furthermore, there is still no consensus regarding the design and diameter of the connector, nor enough information concerning how different veneering techniques affect fracture strength. Hence, further studies are needed to improve the fracture strength over time of FDPs made from stabilized zirconia.
AIMS
The overall aim of this thesis is to evaluate how to improve the design of Y-TZP fixed dental prostheses to increase fracture resistance. The thesis also seeks to evaluate the effect of tooth analogues on fracture strength of Y-TZP.
Specific aims
• To investigate how the fracture strength of 3-unit all-ceramic FDPs made of Y-TZP is dependent on different connector dimensions.
• To evaluate how various radii of curvature in the embrasure area of the connector affect the fracture strength of three-unit all-ceramic FDPs made of Y-TZP.
• To investigate how the choice of material used for supporting tooth analogues and support complexity influences test results relating to fracture strength of FDPs made of the brittle mate-rial Y-TZP.
• To investigate how default settings of two CAD/CAM systems affect the fracture strength and the fracture mode of three-unit and four-unit all-ceramic FDPs made from Y-TZP by compa-ring the radii of curvature in the embrasure area of the con-nector.
• To investigate how FDP length (i.e., number of pontics) affects the fracture strength of Y-TZP.
• To investigate and compare the fracture strength and fracture mode in 11 groups of multilayer three-unit all-ceramic Y-TZP FDPs of the kind currently most common with respect to the choice of core material, veneering material, manufacturing technique, design of connectors, and the radius of curvature of FDP cores.
MATERIALS AND METHODS
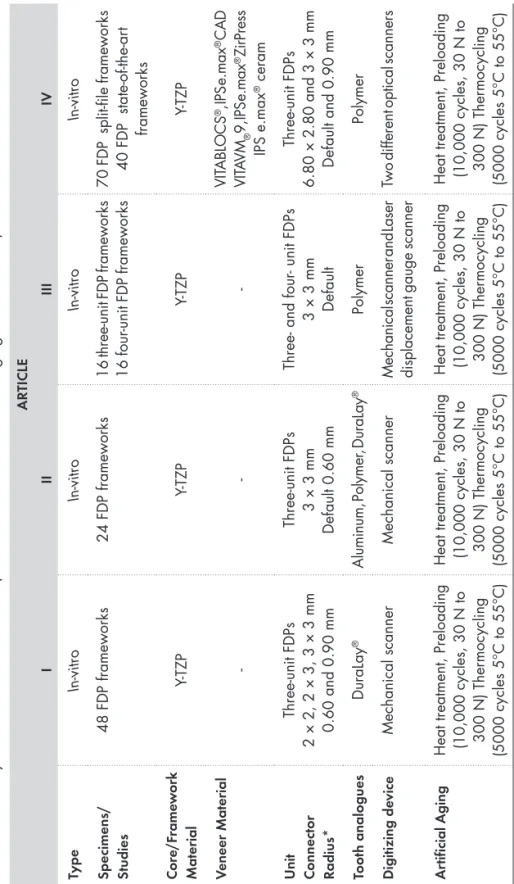
This thesis comprises four in-vitro studies. Table 2 (Table 2.) summarizes the various materials and methods explained in this section. For further details, see the “Materials and Methods” sections of each individual study.
Laboratory Procedures
Study I
Specimen preparation
A master model resembling an upper jaw, with teeth 21 and 23 serving as abutments and tooth 22 missing was made in die stone. Abutments 21 and 23 had a 15° angle of convergence and a cervical preparation design with a 120° chamfer. After scanning this master
model with a mechanical scanner, the Procera® Forte (Nobel Biocare,
Gothenburg, Sweden), design of the various connector dimensions and the radii of the curvatures of the gingival embrasures were made and divided into groups, (Table 3.) using the scanned data from the CAD software (Procera PCMS, version 1.5, build 75 software). The Procera Production Centre (Nobel Biocare, Stockholm, Sweden) then produced
a total of 48 anterior all-ceramic FDPs from Procera® Zirconia bridge
material following regular production procedures. The FDPs were supported by end abutments and with one pontic, divided into six groups of eight FDPs each according to their connector dimension and design.
Table 2.
Summar
y of materials and methods (*Radius of the cur
vature of the gingival embrasure).
ARTICLE I II III IV Type In-vitro In-vitro In-vitro In-vitro Specimens/ Studies 48 FDP frameworks 24 FDP frameworks
16 three-unit FDP frameworks 16 four
-unit FDP frameworks
70 FDP split-file frameworks 40 FDP state-of-the-ar
t frameworks Cor e/F rame w ork Material Y-TZP Y-TZP Y-TZP Y-TZP V eneer Material -VIT ABLOCS ®, IPS e.max ® CAD VIT AVM ® 9, IPS e.max ® ZirPress IPS e.max ® ceram U nit Connect or Radius* Three-unit FDPs 2 × 2, 2 × 3, 3 × 3 mm 0.60 and 0.90 mm Three-unit FDPs 3 × 3 mm Default 0.60 mm
Three- and four
- unit FDPs
3 × 3 mm Default
Three-unit FDPs
6.80 × 2.80 and 3 × 3 mm Default and 0.90 mm
Toot h analogues DuraLay ® Aluminum, Polymer , DuraLay ® Polymer Polymer Digitizing de vice Mechanical scanner Mechanical scanner
Mechanical scanner and Laser displacement gauge scanner
Two different optical scanners
Ar
tif
icial Aging
Heat treatment, Preloading (10,000 cycles, 30 N to 300 N) Ther
mocycling
(5000 cycles 5°C to 55°C)
Heat treatment, Preloading (10,000 cycles, 30 N to 300 N) Ther
mocycling
(5000 cycles 5°C to 55°C)
Heat treatment, Preloading (10,000 cycles, 30 N to 300 N) Ther
mocycling
(5000 cycles 5°C to 55°C)
Heat treatment, Preloading (10,000 cycles, 30 N to 300 N) Ther
mocycling
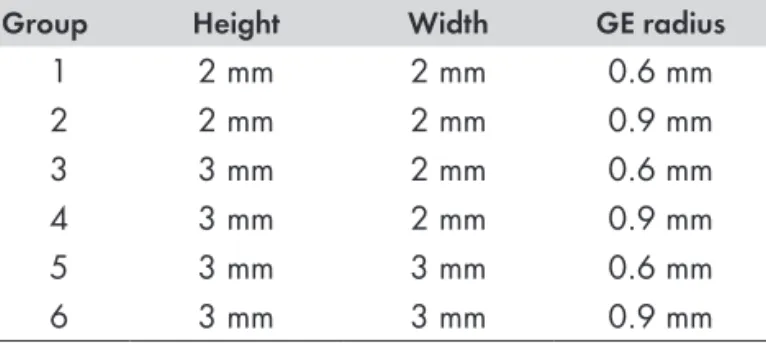
Table 3. Study I: Connector diameter and radius of the curvature of the gingival embrasure (GE radius).
Group Height Width GE radius
1 2 mm 2 mm 0.6 mm 2 2 mm 2 mm 0.9 mm 3 3 mm 2 mm 0.6 mm 4 3 mm 2 mm 0.9 mm 5 3 mm 3 mm 0.6 mm 6 3 mm 3 mm 0.9 mm
Heat treatment
All FDP cores underwent heat treatment in a calibrated porcelain furnace (Multimat Touch & Press; Degudent, Dreieich, Germany) to simulate the firing cycles of the veneering porcelain (Nobel Rondo™ Zirconia, Nobel Biocare) manufacture recommended veneering porcelains for the core material used. Heat treatment comprised four firing programs: Liner, Dentin 1, Dentin 2, and Glaze, all according to the manufacturer’s instructions.
Supporting tooth analogues
The fabrication of supporting tooth analogues was created by reproducing the abutments of the master cast, first and third incisor, were reproduced using A-silicon impression material (President, Coltene AG, Altstätten, Switzerland), to make two tooth-like end abutments on which the FDPs could be cemented and fixated in acrylic blocks. Impressions were taken of the central incisor and canine abutments using A-silicon impression material (President, Coltene AG) then poured in die stone (Vell-mix, Kerr, Romulus, MI, USA) with a metal dowel pin centred in each abutment to stabilise the following build-up of a wax-up. Grooves were made on the dowel pins to facilitate retention of the wax. The above-mentioned reproduction abutments were to be used only to create the shape for the final test model and were not to be used in the test. They were copied in a second step using an A-silicone impression (President, Coltene
AG) and subsequently poured with inlay pattern resin (DuraLay®,
Reliance Dental MFG Co., Worth, Illinois, USA) which was weighed and measured according the manufacture recommendation, creating the final model for the experiment (Figure 2). A total of 48 tooth analogues, 96 copies, 48 incisors and 48 canines were made.
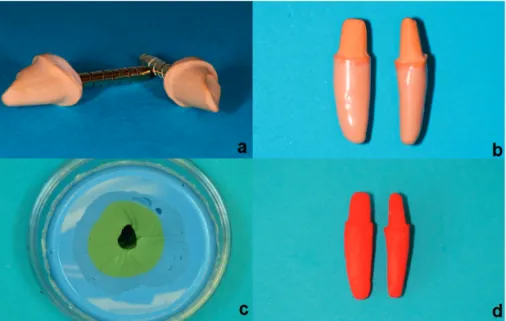
Figure 2 (a-d). Fabrication of supporting tooth analogues: (a) First and third incisor reproduced from master impression poured in die stone, (b) Wax-up of rots, (c) Mold for duplicating wax-up, (d) Incisor and canine in DuraLay®.
Cementation
The DuraLay® tooth-supporting analogues were cleaned and treated
with ED primer II A and B (Kuraray Medical INC.) which was applied to the cementation surfaces according to manufacturer’s instructions.
The FDPs of all groups were luted onto the reproduction abutments with Panavia F 2.0 luting cement (Kuraray Medical INC.) using both Oxyguard II (Kuraray Medical INC.) and light curing lamp (Ivoclar-Vivadent Bluephase, Scaan, Liechtenstein). Polymerization light inten-sity was 1100 mW/cm2 and curing time was 20 seconds in each of four directions, 90° apart, and then 60 seconds in one direction with the seating load removed, according to the manufacturer’s recommendations. During setting of the cement, all FDPs were loaded in the direction of insertion with a force of 15 N for a period of 60 seconds. The cemented FDPs were fixated in holes in acrylic blocks with die stone (Vell-mix, Kerr, Romulus, MI, USA) subsequent to cementation before starting of ageing of the FDPs cores. To create moist environment of the oral cavity, the FDPs were placed in a plastic container, with a sealable lid,
and with distilled water (37±1°C). The FDP cores remained in this moist environment throughout the testing period until load-to-fracture.
Artificial aging - thermocycling and cyclic preload
Artificial aging comprised two steps. The first stage of aging – thermocycling (TC) – put each FPD through 5000 cycles in two water baths at temperatures of +5°C and +55°C, respectively. Each cycle lasted 60 seconds: 20 seconds in each bath and 10 seconds to complete the transfer between baths. In the second stage of aging, all specimens underwent cyclic preloading of 30 N and 300 N in a wet environment and mounted at a 10° inclination relative to the vertical plane. Cyclic preloading comprised 10,000 cycles with a load profile in the form of a sinusoid wave at 1 Hz. A stainless steel indenter, 2.5 mm in diameter, applied the force centrally on the incisal edge of the lateral incisor pontic to avoid sliding during loading (Figure 3).
Figure 3 (a-d). A schematic picture of the jig and the application of the
load during preloading and load-to-fracture: (a) brass foundation, (b) tooth analogue, (c) the pontic, (d) stainless steel indenter.
Load to fracture
The specimens were placed in a testing jig at a 10° inclination and subjected to a load applied by a universal testing machine (Instron
4465, Instron Co. Ltd, Norwood, MA, USA). The crosshead speed was 0.255 mm/min and the load was applied with a stainless steel intender 2.5 mm in diameter, placed centrally on the incisal edge of the lateral incisor pontic. Fracture was defined as a visible fracture through the entire construction.
Statistics
Means of the Student’s t-test determined the differences in fracture
strength between the groups at a level of significance set to p ≤ 0.01.
Study II
Preparation of master casts for three-unit FDPs
For the 3-unit mater cast, plastic model of an upper jaw (KaVo Dental GmbH, Biberach, Germany) was used. Two abutment preparations were made on the 21 incisor and the 23 canine with missing teeth 22. The aim was to design a preparation with a 120° chamfer and an angle of convergence of 15°. Subsequently a full arch A-silicone (Flexitime Mono Phase, Heraeus Kulzer, GmbH, Hanau, Germany)
impression was taken and poured with die stone (Everest® Rock,
Type 4 die stone, KaVo Dental) to produce a master cast (Figure 4).
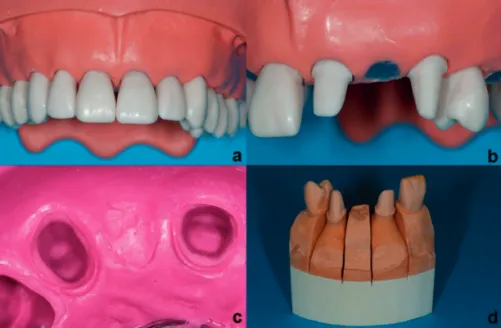
Figure 4 (a-d). Master model production: (a-b) Plastic model with two
abut-ment preparations, (c) Impression of plastic model, (d) Master cast in die stone.
Specimen preparation
The master cast was scanned once with a mechanical scanner,
Procera® Forte (Nobel Biocare, Zurich, Switzerland). The connector
dimensions were set to 3 mm x 3 mm and the minimum thickness of the core was set to 0.7 mm. The radius of the gingival embrasure in the connector areas was 0.6 mm in accordance with both the default settings of the CAD program and the manufacturer’s
recommendations. A total of twenty-four FDPs in Procera® Zirconia
bridges were produced following standard production methods.
Supporting tooth analogues
Study II required three types of tooth analogue (Figure 5). Two of the tooth analogues were milled using the same CAD file as the one
used to produce the FDP cores at the production center (Procera®
Production center, Stockholm, Sweden), and the other, complex tooth analogue was made using the same technique described in Study I. The milled tooth analogues were made from either aluminum or a polymer material (polyoxymethylene-copolymer [POM-C]). The
complex tooth analogues were made of DuraLay® (Reliance Dental
MFG Co., Worth, Illinois, USA). A total of 24 tooth analogues divided in 3 groups were to be made.
Figure 5 (a-c). Tooth analogues: (a) Tooth analogues milled from aluminum,
(b) Tooth analogues milled from polymer material, (c) Complex tooth ana-logues made in DuraLay® cemented to a Y-TZP FDP, fixated in acrylic block
with die stone.
Heat treatment and artificial ageing - TC
All specimens received heat treatment using the same firing program as Study I and in the same manner. Furthermore, all FDP cores underwent TC (LTC Multifunctional Thermocycler; LAM Technologies Electronic Equipment, Firenze, Italy) for 5000 cycles in the same manner as Study I using a small basket controlled by a device driver.
Cementation
The tooth analogues made from aluminum received steam cleaning before treatment with a metal adhesive primer (Alloy primer; Kuraray Medical Inc., Okayama, Japan). The tooth analogues made from
polymer and those made from DuraLay® were steam cleaned and
subsequently treated with ED primer II A and B (Kuraray Medical Inc.). The specimens were luted onto the reproduction abutments with Panavia F 2.0 luting cement (Kuraray Medical INC.) using both light and Oxyguard II (Kuraray Medical INC.), all according to the manufacturer’s recommendations. All specimens cemented to the tooth analogues in Study II used the same cementation procedures as in Study I and were stored in the same manner as in Study I, both to create a moist environment like the oral cavity and to prevent desiccation of the luting cement.
Cyclic preload and Load to fracture
All specimens received cyclic preloading of 10,000 cycles and were loaded to fracture in the same manner as Study I.
Statistics
Means of the Student’s t-test determined differences in fracture
strength between the groups with the level of significance set to p ≤
0.001. Fisher’s exact probability test calculated differences in fracture
modes at a level of significance of p ≤ 0.01.
Study III
Preparation of the master cast for three-unit and four-unit FDPs
The master cast of the three-unit was the same master cast used in Study II. The mater cast of the four-unit were made with the same design and material as the 3-unit mater cast. Two abutment preparations were made of the right central incisor and the left canine, the left central incisor and the left lateral incisor were removed (Figure 6).
Figure 6. A plastic model with two abutment preparations, incisor 11 and canine 23, for preparation of the four-unit master cast.
Specimen preparation
Study III used two different scanners to produce the specimens for four groups with two different designs and units of two different lengths. The master casts were scanned with a mechanical scanner,
Procera® Forte (Nobel Biocare, Zurich, Switzerland) and the data was
transferred to a computer equipped with CAD software (Procera CAD Design C3D, version 2.60) where the intended design of the FDPs was established. The connector dimensions were set to 3 mm x 3 mm and the minimum thickness of the core was set to 0.7 mm. The radius of the gingival embrasure in the connector areas was 0.6 mm according to the default settings in the CAD program and according to the manufacturer’s recommendations. To generate data for the last two groups, the master cast was scanned with a laser displacement gauge
scanner, NobelProcera® Scanner (Nobel Biocare, Zurich, Switzerland).
The data was transferred to a computer equipped with CAD software (NobelProcera 3D prosthetic design, version 4.1.10.4.). This software produced the intended design of the FDPs according to the protocol established for the first two groups. A total of 32, all-ceramic Y-TZP FDP cores: 16 three-unit and 16 four-unit cores with differing design were made. These FDPs had either one or two intermediate pontics, supported by end abutments. The FDPs were then divided according to design in four groups, with eight FDPs in each group.
Heat treatment and artificial aging - thermocycling
All specimens received heat treatment and TC for 5000 cycles in the same manner as Study II.
Supporting tooth analogues
The production center (Procera® Production Centre, Stockholm,
Sweden) produced the tooth analogues for the testing procedure at the same time it produced the FDPs from the same CAD file as the one used to produce the Y-TZP FDP cores, as the same manner as in Study II. A total of 32 tooth analogues, 16 three-unit and 16 four-unit inspection blocks, from a polymer material.
Cementation
The tooth analogues received steam cleaning and subsequent treatment with ED primer II A and B (Kuraray Medical Inc.). The specimens were luted onto the reproduction abutments with Panavia F 2.0 luting cement (Kuraray Medical INC.) using both light-cured
with a curing lamp (Heraeus Translux® Power Blue®, Hereaus Kulzer
GmbH, Hanau, Germany) and Oxyguard II (Kuraray Medical INC.), all according to the manufacturer’s recommendations. All specimens cemented to the tooth analogues were cemented and stored in the same manner as Studies I and II, to create a moist environment of the oral cavity and to prevent desiccation of the luting cement.
Cyclic preload and load-to-fracture
All specimens underwent cyclic preloading for 10,000 cycles and load-to-fracture in the same manner as Studies I and II.
Statistics
Means of the Student’s t-test determined differences in fracture strength between the groups with the level of significance set to
p ≤ 0.05.
Study IV
Preparation of the master cast
In this study, the master cast of the three-unit FDP was the same master cast used in Study II and Study III.
Specimen preparation
To prepare the specimens in Study IV, two different optical scanners were used. Data for Groups 1-7 (the split-file core design) were generated using the Sirona InEos Blue (Sirona Dental Systems GmbH, Germany). The master cast was scanned once and the
data was transferred to a computer equipped with CAD software (Sirona inLab, version 3.88) which produced the intended design of the FDP. Data for Groups 8-11 (the state-of-the-art core design) were generated with the 3shape D640 (3Shape A/S, Copenhagen, Denmark). The master cast was scanned once and the data was transferred to a computer equipped with CAD software (Dental-designer 3shape 2013, build 2.8.8.0) which produced the intended design of the FDP. A total of 110 anterior three-unit Y-TZP FDP cores with one intermediate pontic, supported by end abutments, were made (Figure 7), (Table 4.). In addition to the 110 FDPs, we made two extra cores, one of each design for analyzing the connector cross-section areas.
Figure 7. Overview of all-ceramic FDPs, Groups 1–11: core design,
core material, and veneer techniques.
Split-file design cores
The split-file design was made in total of 70 FDP split-file cores, divided into seven groups. In four groups the FDPs were made in
Bad Säckingen, Germany). In three groups the FDPs were made in
IPS e.max® ZirCAD for inLab MO 0 B40 (Ivoclar Vivadent AG,
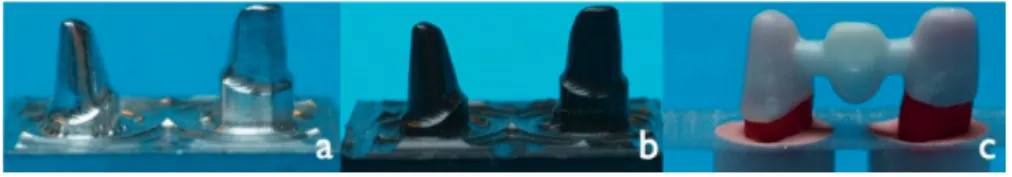
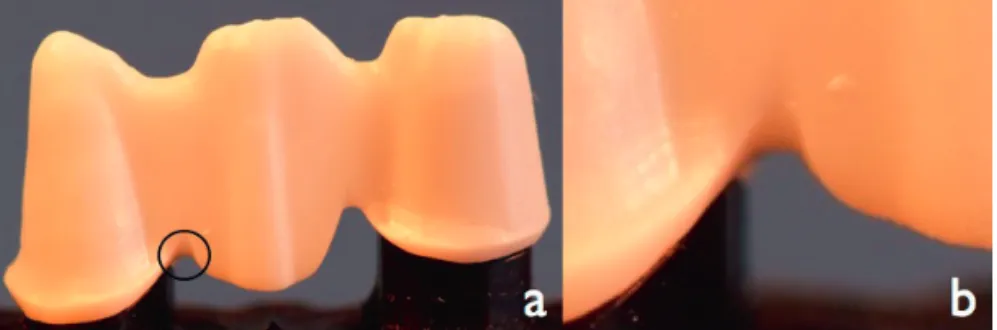
Liechtenstein). The connector dimensions of the Y-TZP cores in the split-file groups were 5.40 mm × 2.50 mm for the left central incisor and 6.80 mm × 2.80 mm for the left canine, with a bar-shaped occlusal design in accordance with the default settings of the CAD program. The core thickness was 0.70 mm. The radius of the curvature of the gingival embrasure in the connector areas was selected according to the default settings of the CAD program and the manufacturer’s recommendations (Figure 8).
Figure 8 (a-b). (a) Split-file core design: Circle shows the radius of the
gingival embrasure; (b): Enlargement of the radius of the curvature of the gingival embrasure.
Veneering of the split-file core
The aim was to create a split-file design structure that allowed a veneering material with a thickness of 1.5 mm. The CAD data for the FDPs were sent to a milling machine Sirona inLab MCXL (Sirona Dental Systems GmbH, Germany), which produced the split-file designed FDPs. The design of the veneering materials in the four milling groups followed the manufacturer’s recommendations. In one of the groups, the material used for the milled veneer structures was
prepared from VITABLOCS® (VITA Zahnfabrik) and subsequently
luted onto the substructure with Panavia F 2.0 luting cement (Kuraray Medical Inc.). In two of the groups, the material used for
veneer milling was IPS e.max® CAD (Ivoclar Vivadent AG), which
Connect (Ivoclar Vivadent AG). The veneers for the overpressing
group were milled from combustible acrylic blocks of IPS AcrylCAD®
(Ivoclar Vivadent AG), then mounted onto the cores, and finished
with over-pressing according to the lost-wax method using IPS e.max®
ZirPress (Ivoclar Vivadent AG). All frameworks of the multilayer veneer were attached following the manufacturers’ instructions.
State-of-the-art core design
The state-of-the-art cores comprised four groups, containing a total
of 40 FDPs. Two of the groups were made in VITA In-Ceram®
YZ DISC, Ø 98 x 18 mm (VITA Zahnfabrik). The remaining two
groups were made in BruxZir® HT 2.0, Ø 98 x 15 mm (Glidewell
Laboratories, California, USA). In the CAD program, the design of the connector dimensions of the Y-TZP were set to 3 mm × 3 mm, the minimum thickness of the core to 0.7 mm, and the radius of the gingival embrasures in the connector areas to 0.90 mm. The CAD data for the FDPs were subsequently sent to a milling machine Wieland 4030MN (Wieland Dental, Technik GmbH, Germany), with the software CAM: Zenotec CAM 2.2.017, (Wieland Dental, Technik GmbH, Germany) where they were used for production of the FDPs (Figure 9).
Figure 9. State-of-the-art core design with connector dimensions 3 × 3 mm,
Table
4.
FDP specimens in Study IV
. Connector height and width (H/W), radius of the cur
vature of the gingival embrasure, number
of units, material, a nd c or e de si gn . Gr oup Cor e Y -TZP V eneer H/W α H/W β Radius γ U nit Cor e design 1 VIT A In-Ceram ® CORE* 5.40 × 2.50 mm 6.80 × 2.80 mm default 3-unit Split-file 2 VIT A In-Ceram ® VIT ABLOCS ® 5.40 × 2.50 mm 6.80 × 2.80 mm default 3-unit Split-file 3 VIT A In-Ceram ® IPS e.max ® CAD 5.40 × 2.50 mm 6.80 × 2.80 mm default 3-unit Split-file 4 VIT A In-Ceram ® VIT A VM ® 9 5.40 × 2.50 mm 6.80 × 2.80 mm default 3-unit Split-file 5 IPS e.max ® ZirCAD IPS e.max ® ZirPress 5.40 × 2.50 mm 6.80 × 2.80 mm default 3-unit Split-file 6 IPS e.max ® ZirCAD IPS e.max ® CAD 5.40 × 2.50 mm 6.80 × 2.80 mm default 3-unit Split-file 7 IPS e.max ® ZirCAD IPS e.max ® ceram 5.40 × 2.50 mm 6.80 × 2.80 mm default 3-unit Split-file 8 VIT A In-Ceram ® CORE** 3 × 3 mm 3 × 3 mm 0.90 mm 3-unit State-of-the-ar t 9 BruxZir ® HT 2.0 CORE** 3 × 3 mm 3 × 3 mm 0.90 mm 3-unit State-of-the-ar t 10 VIT A In-Ceram ® VIT A VM ® 9 3 × 3 mm 3 × 3 mm 0.90 mm 3-unit State-of-the-ar t 11 BruxZir ® HT 2.0 VIT A VM ® 9 3 × 3 mm 3 × 3 mm 0.90 mm 3-unit State-of-the-ar t
α Connector dimension in the left central incisor
. β Connector dimension in the left canine. γ Radius of gingival embrasur
. *Core only – tested without veneer material.
Same core design as group 1-7. **Core only – tested without veneer material. Same core design as group 8-1
Manually built-up porcelain
To duplicate the shape of the veneers in the milled veneering groups
one of the completed IPS e.max® CAD-on FDPs was placed on a
tooth analogue and the undercuts were waxed. Then duplicated the shape of the FDP using A-silicon and putty impression material (PRESIDENT, Coltène AG, Altstätten, Switzerland). The performed manual layering of the veneering porcelain was made in four groups, two spilt-file and two with state-of-the-art core design. To separate the layered porcelain from the inner surfaces of the impression, we
used a GI-MASK® universal separator for silicones, Coltène® (Coltène/
Whaldent AG, Switzerland) and thereafter applied LPC Isolating
Liquid (Ivoclar Vivadent AG). The VITAVM®9 (VITA Zahnfabrik,
Germany) porcelain, was used to veneer two groups of state-of-the-art cores and one of the two split-file core groups. The last group
of split-file cores received IPS e.max® Ceram(Ivoclar Vivadent AG,
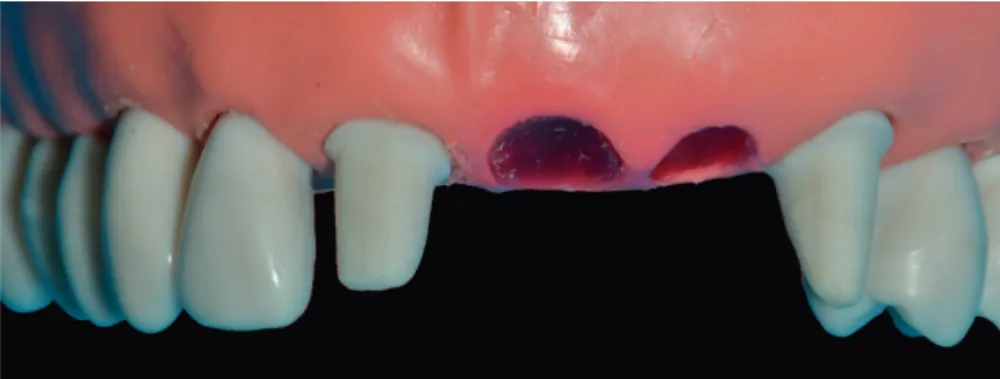
Liechtenstein). Veneering ceramic for dentin was applied on the FDPs frameworks using the impression to achieve standardized shape and size of the FDPs. All the layered FDPs then underwent a first firing. A second layer dentin ceramic was applied to compensate the sintering shrinkage (Figure 10) and finally applied glaze to the FDPs. All porcelain firing proceeded in a calibrated porcelain furnace (Ivoclar P 500; Ivoclar Vivadent AG) according to the firing programs (Table 5-6) recommended by the manufacturer’s instructions.
Heat treatment and artificial aging - thermocycling
Three groups comprised core material only. One group had a split-file
core made of VITA In-Ceram® YZ (VITA Zahnfabrik). The other
two groups had state-of-the-art cores design with one group made of
VITA In-Ceram® YZ (VITA Zahnfabrik) and one of BruxZir® HT 2.0
(Glidewell Laboratories). The FDP cores in the three groups were sub-jected to heat treatment to simulate the firing cycles of the veneering
porcelain VITAVM®9 (VITA Zahnfabrik, Germany) and IPS e.max®
ceram(Ivoclar Vivadent AG, Liechtenstein) according to the
manu-factures recommendations. The group FDPs made of VITABLOCS®
(VITA Zahnfabrik, Germany), which was subsequently luted onto the substructure with Panavia F 2.0 luting cement (Kuraray Medical INC) were excluded from the heat treatment procedure according to the manufacturer’s recommendations. All specimens received thermo-cycling for 5000 cycles in the same manner as Studies II and III.