The importance of
evaluating before
selecting appropriate
activities as
interventions in
psychiatry
MAIN FIELD: Occupational Therapy
AUTHORS: Dagnäs, Maja & Fredriksson, Julia SUPERVISOR:Edström, Eva
JÖNKÖPING: 2020
A qualitative study conducted as a Minor Field Study at a
psychiatric clinic in Vietnam.
Summary
Aim: The purpose of this study is to describe the intervention process at a psychiatric clinic in Vietnam,
from evaluation to goal setting, and how the staff choose occupation-based intervention for their patients. Method: This study is a qualitative study with inductive approach where the data collection is based on a semi-structured interview with the health care staff at a psychiatric clinic in Vietnam. The respondents consisted of a total of ten participants and were required by a purposive sample. Content analysis according to Kristensson (2014) was used to examine the data. Result: The findings from the result revealed that the clinic work without a standard procedure where the staff evaluates and assess their patient from their own experience. They also interview and observe the patients without an aim. The result also showed that the clinic offers different occupation-based interventions where the doctor decides occupation-training but not in consultation with the patient. It was revealed that the purpose of the occupation is to make the patients independent. The last finding was that the staff has a lack of individual goal setting and the general goal is for patients to get healthy. To see if the patients achieve improvement, observations are made without aim. Conclusion: The study concludes that the health care staff at the clinic has found their strategies using their own experience, for evaluating and assessing their patients.
Keywords: Assessment, Goal setting, Mental illness, Occupation-based interventions, Occupational
Sammanfattning
Betydelsen av att utreda innan man väljer lämpliga aktiviteter som interventioner inom psykiatrin
En kvalitativ studie utförd som en mindre fältstudie vid en psykiatrisk klinik i Vietnam
Syfte:
Syftet med studien var att beskriva arbetsprocessen på en psykiatriklinik i Vietnam, från utredning till målsättning och hur vårdpersonalen väljer aktivitetsbaserade interventioner för sina patienter. Metod: Studien är kvalitativ med en induktiv ansats där datainsamlingen bygger på en semistrukturerad intervju med vårdpersonal på en psykiatriklinik i Vietnam. Studien bestod av tio deltagare och rekryterades genom ett målmedvetet urval. Innehållsanalys enligt Kristensson (2014) användes för att analysera datainsamlingen. Resultat: Resultatet visade att kliniken arbetarutan att följa en standardprocedur. Vårdpersonalen utreder och bedömer sina patienter utifrån egen erfarenhet. De intervjuar och observerar patienterna utan något specifikt syfte. Resultatet visade också att kliniken erbjuder olika aktivitetsbaserade interventioner där läkaren bestämmer patientens aktivitetsträning men detta sker inte i samråd med patienten. Det framkom att syftet med aktiviteterna är att göra patienterna självständiga. Det konstaterandes också att vårdpersonalen har brist på kunskap om individuell målsättning och deras generella mål är att patienterna ska bli friska igen. För att se om
patienterna uppnår förbättring genomförs observationer utan grund.
Slutsats: Vårdpersonalen på kliniken har hittat strategier med hjälp av sin egen erfarenhet för att
utreda och bedöma sina patienter.
Nyckelord: Aktivitetsbaserade interventioner, Arbetsterapi, Bedömning, Målsättning, Psykisk ohälsa, Vietnam
Table of content
1.
Statement of the topic and need for the study ... 1
2.
Background ... 2
2.1 Mental illness in Asia ... 2
2.2
Occupational Therapy ... 2
2.3
Intervention Process Model ... 3
3.
Purpose of research ... 5
4.
Methodology ... 6
4.1 Preunderstanding ... 6
4.2 Participants ... 6
4.3
Data collection... 6
4.4 Data Analysis... 6
4.5 Principles of Ethics ... 8
5.
Resultat ... 9
5.1 Work without standard procedures ... 9
5.1.1 Evaluation and assessment from the staffs own experience ... 9
5.1.2 Interview and observation without aim ... 10
5.2 Different activities as interventions offered at the clinic ... 10
5.2.1 Activity training decided by the doctor and not in consultation with the patient
... 10
5.2.2 The purpose of the activity is to make the patient independent ... 10
5.3 Lack of individual goal setting... 11
5.3.1 Setting goals without knowing what the patient wants to achieve ... 11
5.3.2 Knowing when the patient achieves improvement by observation ... 11
6.
Discussion of the findings ... 12
6.1 Discussion of the methodology ... 12
6.1.2 Participants and requirement... 12
6.1.3 Interview guide ... 12
6.1.4 Data collection ... 12
6.1.5 Data analysis ... 13
6.2 Discussion of the Results ... 13
6.2.1 Individual treatment using a client-centered perspective ... 13
6.2.2 Evidence-based evaluation and assessment of the patients ... 14
6.2.3 Goal-setting ... 15
6.2.4 How occupational therapy practices can benefit to the clinic in Vietnam ... 15
6.2.5 Recommendations for further research ... 15
7. Conclusion ... 16
9.
Appendix ... 0
1. Information Letter ... 0
2. Consent Form ... 0
1
1. Statement of the topic and need for the study
The population of Vietnam is about 84 million people and is the second most populated country in South-East Asia (Bhugra, 2016). It is estimated that 12 million people in Vietnam may be in some need of mental health services and the most common issues regarding mental illness are alcohol abuse, depression, and anxiety (Vuong et al, 2011). Mental health care in Vietnam is characterized by a low priority to mental health services. There are 24 mental health units, 25 psychiatric departments in the hospitals, and 33 psychiatric hospitals in Vietnam. The largest challenge for mental health care in Vietnam is to attract mental health workers. The education of psychiatric primary care staff is complicated and limited and there is a lack of psychiatric health topics and psychiatric textbooks in Vietnamese. To promote mental health should be the aim in the country, and to provide a person-focused service that is cost-effective and available. Mental health services capacity and human resource development need to be increased and continuous research and learning should be pursued (Bhugra, 2016). According to Hayashi (2010), there is a lack of educational institutions or schools in occupational therapy [OT] in Vietnam. In some third world countries the ratio between patient and OTs is poor and assessments are often neglected (Crouch & Alers, 2014). Occupational therapists play an important role in the rehabilitation of mental health care. The process in OT is based on repeated and initial assessments and there are several strategies to use (Taylor & Kielhofner, 2017). An effective occupational assessment is necessary to understand the patient and their needs (Taylor & Kielhofner, 2017). Without a good assessment, qualitative and evidence treatment cannot be provided (Crouch & Alers, 2014). The assessment should be done as early as possible and there is a lot of research and experience that underline the importance of getting started early with evaluation, assessment, and efforts. An early assessment is fundamental to effective and successful rehabilitation (Ekberg et. al, 2015).
Research on previous studies has been searched for in both literature and articles on how OTs evaluate and assess patients with mental illness, both in the world and specifically in Vietnam. Articles about goal setting and occupation-based interventions have also been searched for. Despite extensive background about evaluation and assessment, not much research has been found about the chosen problem topic. Therefore, it is of great importance that new research and knowledge in this area is studied and can be of benefit to staff and patients.
This study is part of a scholarship project called Minor Field Studies which is financed by the Board of International Development Cooperation [SIDA]. This board allows students to go to a developing country and write their bachelor's degree for eight weeks. The purpose of the project is to provide students with increased knowledge about development issues and motivate why the study is needed (SIDA, 2017). This study is in relation to the 17 Global Goals which the world leader’s year 2015 agreed to (United Nations, n.d.). The ambition of these goals is to develop and achieve a sustainable future since the world today is facing a lot of challenges like climate change, health-related problems, and poverty. The world must work together to build a better future for everyone. The specific goal of this research is related to the third Global Goal which is “Good health and wellbeing” (United Nations, n.d.).
The study was conducted at a psychiatric clinic in Vietnam. The clinic offers open and closed care and treats both adults and children. Those who work there are doctors, nurses, psychologists, physical therapists, and assistant nurses. There are about 50 male patients at a time who is treated with closed care. The most common diseases among the patients are depression, alcohol and drug problems, schizophrenia, ADHD, autism, and epilepsy. The health care staff offers different activites for the patient as a part of the treatment.
2
2. Background
2.1 Mental illness in Asia
According to World Health Organization [WHO] one of four people in the world is affected by mental illness. The term mental illness is defined as a mental imbalance (The Public Health Agency of Sweden, 2017). Mental illness is a range of problems with different symptoms. They are in general characterized by some combination of abnormal emotions, behavior, thoughts, and relationships with others. Examples of common mental disorders are depression, anxiety, eating disorders, ADHD, intellectual disabilities, schizophrenia, and disorders due to drug and alcohol abuse (World Health Organization, n.d.).
The biggest problem of mental health care in Asia is the lack of financial and personal resources and mental health professionals are mostly located in the bigger cities (Lauber & Rössler, 2007). About 73% of the population in Vietnam lives in rural areas (Bhugra, 2016). This creates a barrier for people to seek help and this contributes to the stigmatization of the mentally ill (Lauber & Rössler, 2007). Stigmatization of people with mental illness is a frequent problem that affects participation in society and prevents their recovery. The stigmatization can over the long-term lead to a smaller group of friends, discriminations in daily life, and difficulties at work (Gaebel et al., 2011). In Asia there is a wide tendency to discriminate and stigmatize people with mental illness which can increase the social distance (Lauber & Rössler, 2007).
People suffering from a mental illness diagnosis such as depression can experience social exclusion due to their mental disability. Occupations and community-services can be a big part to help these people participate in activities (Lipskaya-Velikovsky et al., 2016).
Participating in an occupation is to be engaged in the occupation like work, occupations in daily life, spare time activities, or activities that are necessary for a social-cultural context for mental and social wellbeing. Examples of this could be having a job, going to school, voluntary work, or being with friends (Taylor & Kielhofner, 2017).
2.2 Occupational Therapy
An occupational therapist supports patients to be able to participate in daily activities. Occupational therapists achieve this result by supporting patients to improve their abilities and be able to participate in the activities they need. Occupational therapists provide support in occupational training and, suggestions for adapting the everyday environment and helps the patients design strategies that make everyday life work (World Federation of Occupational Therapists [WFOT], 2020).
The role of the occupational therapist in psychiatry is to focus on the consequences of mental disabilities rather than the cause of them (Ottosson & Ottosson, 2007). It's about supporting the patient to find a way to make their everyday life work (Ottosson & Ottosson, 2007). The purpose of the treatment is to enable the patient to recover in social integration and rehabilitation (Finlay, 2004). The occupational therapist works together with the patient with a focus on individual and environmental abilities related to activities in the person's daily life (WFOT, 2020). Occupational therapists have the skills, knowledge, and education to offer interventions for adults living with mental disabilities. Evidence-based interventions can enable individuals to participate in meaningful activities as well as help and participate in community life (Lannigan & Noyes, 2019).
According to Taylor & Kielhofner (2017) the Model of Human Occupation [MOHO], which is a theoretical model in occupational therapy, there are three important components: volition, habituation, and performance capacity. These factors in conjunction with the environment affect motivation, pattern, and execution when performing in occupation (Taylor & Kielhofner, 2017). The environment has a major impact on all activities, both social environment and physical environment. The social environment includes other people how to influence the patient’s occupation, like the patient's social partners. The physical environment includes for example tools and digital devices (Fisher & Marterella, 2019). An occupation that is performed, is motivated by will-determined thoughts and feelings, values, and self-interest. Volition is referred to as motivation for occupation and is regulated by our thoughts and feelings. Volition is an ongoing process, which means that our experience, interpretation, anticipation, and choice is an open process and arises about things we have done, experienced, or are going to do. This means that the individual chooses activities and occupation that motivate them (Taylor & Kielhofner, 2017).
3
Habits are defined as patterns of thoughts, occupation, and speech that are unconscious for how to act and react in familiar situations and environments. Occupational therapy involves restoring a functioning new habit that allows people to integrate feelings, occupation, and thoughts. It also contributes to people's reorganization and recapturing old habits and help to develop new ones (Mårtensson & Archenholtz, 2017). Habits and routines influence our everyday behavior, what we do, when we do it, and how we do it. This gives life structure and predictability. Performance capacity is the ability to perform occupation based on the status of the objective physical and mental factors as well as the subjective experience. The objective and subjective aspects affect each other and go hand in hand and contribute to an performance. They together create the ability to perform an occupation (Taylor & Kielhofner, 2017).
The word structure is explained as “establishing clear expectations of performance by offering people alternatives, setting limits, or establishing ground rules” (Taylor & Kielhofner, 2017, p. 198). Using structure creates demands on the patient to maintain habits and roles. The structure allows the patient to have a feeling of control. External expectations increase the willpower of the patients, which means that the patient has an easier time motivating themselves to do things when others expect something (Taylor & Kielhofner, 2017). Structure in everyday life is important for all people, it provides security and stability in their life. People with mental illness need to have structure as they often have problems creating and maintaining external and internal structures (Eklund et al., 2010).
2.3 Intervention Process Model
According to Fisher & Marterella (2019), there is an intervention process model when evaluating a patient. The first step is to gather initial information about the patient and to identify strengths and problems. The OT also needs to find out what occupational performance the patient wants to prioritize. The next step is to observe the patient’s quality when performing occupation and gather the patient’s perspective of the performance and also to rate the patient’s quality of occupational performance. When this is done, an occupation-focused goal is determined together with the patient. The next phase is to select an appropriate intervention model and to implement this. There are four different types of models to use when choosing an intervention.
The models are the compensatory model, educational and teaching model, acquisitional model for occupational skills training, and the restorative model for enhancing body functions and other patient elements.
The compensatory model focuses on to compensate for decreased occupational skills. This includes the adaption of the environment and technical aids to facilitate occupation performance. This method teaches new compensatory or alternative strategies.
The educational and teaching model is about the planning and implementation of educational programs that focus on the performance of daily life tasks. The purpose is to share knowledge related to occupational experience and occupational performance.
The acquisitional model for occupational skills training is used when a patient needs to restore occupation skills or when a patient needs to develop or maintain occupational skills. Using this model combined with an occupational centered perspective can contribute to an appropriated intervention method.
The restorative model for enhancing body functions and other patient elements is focused on developing, restoring, maintaining, and preventing loss of personal factors such as habits and routines. It also focuses on restoring and maintaining lost body functions.
The last step of the intervention process model is to reevaluate and ascertain outcomes. The OT and the patient will determine if any changes have occurred and if the patient’s goals have been reached or if new goals need to be identified (Fisher & Marterella, 2019).
The occupational therapist works together with the patient to develop treatment goals that are both long-term and short-term goals where the long-term goal is achieved with the help of several short-term goals (Eklund, et al, 2010). The treatment goals are developed by getting to know the patient and identifying the patient's situation and environmental changes that can support the patient's participation in the occupation. To measure whether the patient has achieved his or her goals, a measurement will be executed both before and after an intervention. The results will then be compared to understand how the patient has changed through the process. Occupational therapists help their patients achieve their goals by giving advice, coaching, and encouraging them during the process (Taylor & Kielhofner, 2017).
4
To participate in goal planning is productive and creative for the patient to be able to recover. It has been shown to result in greater satisfaction with rehabilitation when a patient is involved with the goal planning (Doig et al., 2015).
The term occupation includes many different types of genres including work, eating, leisure, rest, pleasure, and recreation. The word doing refers to occupation or occupation and can be described with words such as performing, acting, fixing, getting something done, occupation, caring out, preparing, organizing, and making executing (Wilcock & Hocking, 2015). Activities in daily life include personal activities such as showering and eating and leisure activities such as communication, life skills training, education, travel, cooking, and household chores.The occupational therapy intervention focuses on enabling a good everyday life with meaningful and functioning activities for everyone despite residual functional impairment (Erlandsson & Persson, 2020).
The goal of occupational therapists is to get the patient as independent as possible in both daily lives and society and to feel involved (Malcus-Johnson et al., 2005). Occupational therapists contribute interventions plans by using occupation-based interventions (Creek & Lougher, 2008). Using occupation-based training, the occupational therapist collects information from the patient that makes it possible to understand the patient from the patient's perspective. It is important to understand what the patient does, why and how the patient does it, and how these factors support or limit the patient's ability to work. Occupational therapist evaluates their patients in the context of occupational performance and then they use occupational as a primary form of their therapy. When occupational therapists are using occupational based methods as an intervention, they are engaging the patient in occupation. Occupational based intervention refers to the patient being engaged in an actual task performance (Fisher & Marterella, 2019).
According to Taylor & Kielhofner (2017) an effective assessment is necessary to understand the patient and their occupational needs. To not use assessment and seeking important information about our patients can result in poor outcomes. There are several strategies to use when evaluating a patient, where the first step may be an interview. In addition to this, different measuring instruments and observations in different environments can be used for evaluating and assessing a patient's performance abilities. These types of assessment can provide information about the patient's performance in the past and present, their ability to perform an occupation, their thoughts on their ability and their motivation and planning for the future. Using assessment tools during treatment is a strategy to gather information about the patient and understand the needs that exist. To be able to make a good assessment, a knowledge of the patient's entire situation is required, with a description of his or her physical, mental, and social resources and limitations. Knowledge must be gathered about the patient's own experience of his or her ability (Taylor & Kielhofner, 2017).
The findings and the results of an assessment are the basis of the treatment plan. The plan should include short and long-term goals and should be relevant to the person's roles, habits, lifestyle preferences, and the environment. The intervention are designed to facilitate the performance of everyday occupation and adaptation of the person's work and social life. This can also include teaching of new techniques and providing equipment that can help the patient be more independent (WFOT, 2020).
5
3. Purpose of research
The aim is to describe the intervention process at a psychiatric clinic in Vietnam, from evaluation to goal setting, and how the staff choose activities as interventions for their patients.
6
4. Methodology
This study is a qualitative study with inductive approach. The data collection is based on interviews with the health care staff at the psychiatric clinic. Using a qualitative study is meant to describe and interpret people's experiences in a mapping and systematic way. When not being an experienced researcher, a qualitative study is a good way to collect data (Kristensson, 2014). The focus is to find differences and similarities in the collected material. A semi-structured interview guide was used so the respondent could answer the questions freely and be able to ask follow up questions if needed (Kristensson, 2014). The interview guide was based from the theoretical parts from Powerful practice: A model for authentic occupational therapy (Fisher & Marterella, 2019).
4.1 Preunderstanding
According to Kristensson (2014), preunderstanding is about the author's own images, expectations, prejudices, or conceptions of a phenomenon to be interpreted. The authors' preunderstanding was that this specific clinic do not use any evaluation or assessment instrument. This preunderstanding come from reading another study (Causey & Björn, 2019) that was conducted at the same clinic.
4.2 Participants
The participants of this study are health care staff working at the psychiatric clinic and they were gathered through a purposive sampling where the participants were recruited by the interpreter. The inclusion criteria to participate in the study were to be over the age of 18 and for the participants to have different professions. The exclusion criteria to participate in the study were people under the age of 18, working as an assistant nurse and staff working with children in the clinic. Due to the circumstances of the Corona-virus, assistant nurses had to be interviewd even though this was an exclusion criteria. This will be explained under ‘6.1.2 Participants and requirement’. The participants had different professions and experiences, and this is according to Kristensson (2014), to get a varied sample of the representatives.
4.3 Data collection
The data for the study were collected at a psychiatric clinic in Vietnam. During the interview, an interpreter helped with the language to translate the questions and the answers. The interpreter was working as a doctor at the clinic and is familiar with the staff and the situation with the patient. The interpretation of the answers may be based on the interpreter’s experience. Together with the interpreter the interviews were held in a room close to the patient’s yard. The interviews were held with one participant at a time and the interview hade a time frame of approximately 10-20 minutes. The interviews were based on an interview guide and the interviews were recorded and notes were taken. Using a tape recorder was an effective way to record the dialog. Notes were taken as a complement to easier search for relevant information during the data analysis. It was important to make sure that the information was well collected so it could be correctly used when analyzing the data (Kristensson, 2014).
4.4 Data Analysis
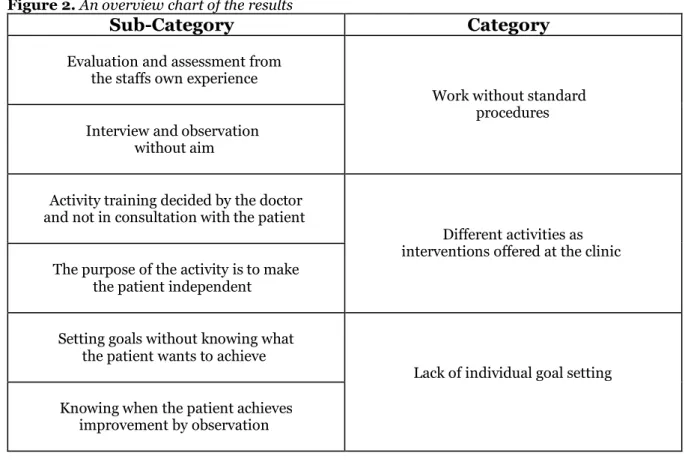
The collected data material was transcribed during the stay in Vietnam and resulted in about 12 pages. Content analysis according to Kristensson (2014) was used to examine the data. The method of a qualitative content analysis focuses on the subject and context, and underline differences and similarities between codes and categories (Graneheim & Lundman, 2004). The data was read thoroughly several times and was discussed to get a sense of the whole picture. The units of meaning were identified in the text and is related to the purpose of the study. The units that are not relevant to the study were deleted. The meaning units were condensed to make the text shorter and easier to work with. Then the coding of the condensed meaning units was performed, which means that the meaning units are labeled with a shorter description of the content. The codes was read through to find similarities and differences between the codes. The codes that belong together form a category (Kristensson, 2014). A category is content that shares a commonality and the 10 interviews resulted in three categories. To find a subcategory the text, categories, and codes were read through (Graneheim & Lundman, 2004). An interpretation of the underlying condensed meaning in the text then became a subcategory (Kristensson, 2014). The analysis is illustrated in a chart (Figure 1).
7
Figure 1. Chart describing an example analyzation of the data Unit of Meaning Condensed unit
of Meaning Code Sub-Category Category
“We don’t have a standard procedure to investigate the
patient, we just work on [from] our experience. […]
They don’t have the standard
procedure
Work from own experience Evaluation and assessment from the staffs own experience Work without standard procedures
“There’s [are] two ways to investigate a patient. The
first way I will ask the patient, I will interview the patient. And the second way
is to observe the patient in the department”
Talk with and
interview the patient. Observe the
patient in the department Evaluation of the patients Interview and observation without aim
“It depends on the activity and the interest of the
patient. “[…] what the present situation [is] of the patient, so that I can choose
the [a] suitable activity for them”
The staff chooses activity depending on the
activity and the patients' interests Activity decided by the patient's diagnosis and daily status Activity training decided by the doctor and not in consultation with the patient activities as Different interventions offered at the clinic
“[…] watch and observe the patient washing the dish so
with this activity the purpose is when the patient
get home it can do the chores. […] make sure they
have the personal hygiene. Like have them to brush their teeth, [and] take
a shower”
The staff watch and observe the patient in different activities
to make sure that they can manage it
by themselves Purpose of the activity training The purpose of the activity is to make the patient
independent
“I have two ways [to set goals]. The first is I will see the records and the second I
will observe the patient. Like for example if a patient
[is] dirty when they get into the department, and
then in a few days they become more clean
[cleaner]”
The staff will set goals based on the
records and observation. Goal setting without consultation with the patient
Setting goals without knowing
what the patient wants to achieve
Lack of individual goal setting “We need to observe the
patient. Like the body hygiene, we observe every day. If the patient
can make themselves clean or not. If the patient cannot we have to
teach the patient step by step”
Observe the patient every day to see if the patient is getting
better Observe the patient to set goal Knowing when the patient achieves improvement by observation
8
4.5 Principles of Ethics
In terms of ethical aspects, the authors of this study have related to the four central principles that Kristensson (2014) describes as important aspects of a research project. These are the principle of autonomy, the utility principle, not to harm principle, and the principle of justice. The principles mean that all participants must be voluntary, that the researcher must consider the risk of injury, and generally use safe methods and that participants are treated on equal terms.
To protect the participants in the study, the research ethical rules were taken into account (Kristensson, 2014). These include information requirements, the project manager's name, and institution on the information letter and consent form. The purpose and context of the study were explained to the participants and they were also informed about the voluntary of the study and the right to cancel whenever they want. It was explained that the results of the study are only for research purposes and the data in the study will be treated confidentially, with no transparency of others, no individual can be identified and duty of confidentiality for ethically sensitive tasks (Kristensson, 2014). Before every interview, the participants were provided with informed consent and an information letter which was translated into Vietnamese by the interpreter. This consent form had to be signed by the participants (Appendix 2). As described in the information letter the participants were assured that their participation in the study was voluntary and could be canceled at any time. The integrity and confidentiality of the participants were respected. Completed anonymity could not be guaranteed. Only the participants' profession was noted.
There are some ethical and reliability aspects to consider when using an interpreter. By using an interpreter, the full meaning of the spoken language must be accurately captured. The translation will likely lose or significantly change the meaning of the data. Using an interpreter could lead to an impact on the trustworthiness of the qualitative data (Al-Amer et al., 2016). Before the interviews, the interpreter signed an approval form regarding confidentiality (Appendix 2) (Kristensson, 2014). According to Kvale and Brinkmann (2009) an interview project needs to be submitted to an ethical review board. This was submitted before the trip to Vietnam since the standards of Jönköping university require that this needs to be accepted before the data collection
9
5. Resultat
The participants were a total of ten health care staff; doctors, nurses, physiotherapists, and assistant nurses. The respondents were in both genders and between the age of 18-45 years. They were all working close to the patients who were temporarily living at the clinic.
Figure 2. An overview chart of the results
Sub-Category
Category
Evaluation and assessment from the staffs own experience
Work without standard
procedures
Interview and observation without aim
Activity training decided by the doctor and not in consultation with the patient
Different activities as
interventions offered at the clinic
The purpose of the activity is to make the patient independent
Setting goals without knowing what the patient wants to achieve
Lack of individual goal setting
Knowing when the patient achieves improvement by observation
5.1 Work without standard procedures
According to the respondents, it turned out that the staff has a lack of structure regarding evaluation, goal setting, and assessment and it emerged that they do not use any standard procedure. This means that the clinic does not have a structured way of evaluating and assessing their patients. According to the respondents, they work from their own experience and they usually start the first meeting with a new patient by small talking and asking basic questions. It all depends on the patients' diagnoses and daily status.
“We don’t have the standard procedure.” - Interview 6
5.1.1 Evaluation and assessment from the staffs own experience
The evaluation and assessment of the patient are not done by any structured procedures. The health care staff use their own experience and ask different questions to the patient and these are adopted by the patient's diagnosis and status. The staff has a team meeting together to discuss patients, and then the doctor will have the final say about the patient and what treatment and activity the patient should have. The nurse will advise the doctor about interventions and which activity that's fits well but it's the doctor that will decide.
“We just talk with the patients and see the records,
10
5.1.2 Interview and observation without aim
According to the respondents, they do not use any structured questions or questionnaires when interviewing the patient for the first time. Primarily, the staff wants to build up a relationship with the patient before they start the therapy. The staff always look at the patient's records before the meeting, they want to know about the diagnoses and the specific symptoms of the patients and the cognitive status of the patient so the staff can give suitable questions. The most common questions at the interview are about how the patient's everyday life looks like, personal information like name, age, and their job, and why the patient comes to the clinic.
“[…]the first meeting, first I will introduce myself and […] asking about the history and ask the problem associated with the patient and then I will call the doctor to see the patient and then I will
arrange the room for the patient. The important factor is that we have to have the [a] good relationship with the patient “- Interview 6
The questions that are asked depends on which profession meets the patient and the questions are never the same. It is most common that the patients come from a rehabilitation department, but others come here for the first time on their own or that their relatives no longer can take care of them. The staff observes the patients in different activities to see how they perform and identify their process skills. But the staff does not look for any special skills, only if the patients seem to look happy. Through observation, the staff sees if the patients are feeling well and if the patients are on the way to
achieve the staff’s goals (managing hygiene for example) and can be discharged
.
5.2 Different activities as interventions offered at
the clinic
The clinic offers different kinds of activities, like workout at the gym, go to the supermarket, cook dinner, clean the beach, etc. A finding from the interviews was that the clinic only offers group therapy/activities and no individual therapy/activity.
“We don’t offer individual therapy.
We just have the group therapy. […]” - Interview 1
5.2.1 Activity training decided by the doctor and not in consultation with the
patient
The health care staff do not use any evaluation or assessment instruments and the findings from the interviews resulted in that the staff only choose activities based on the patient's diagnosis, daily status, interests, and previous job. The staff has a team meeting where they discuss the patients but, in the end, it is the doctor who decides which activities each patient should do. This is not in consultation with the patient. The staff only know the patient's interest, but they do not actually know what activity the patient prefers to do.
“I will choose activity depends on the patient characteristics, if the patient can cooperate with the staff or not and the ability of the patient if they can work with the activity. It also depends on the
previous job of the patient, to see the ability of the patient.” - Interview 5
5.2.2 The purpose of the activity is to make the patient independent
Each activity does have a specific purpose, but it’s not connected to what each patient need. The staff explains that they choose activity depending on if a patient is active or not. If a patient is lazy and lays on the bed a lot, they will make the patient clean the ground or help in the garden. During the group sessions they talk and discuss the patient's diseases. The staff wants the patients to have insight about their disease and help them understand and accept it.
11
The staff wants to stimulate the patient's behavior so that the patient can understand the importance of activity. There are activities available in the yard for those with different interests such as basketball, badminton, books, soccer games, and board games. The staff regularly works to educate patients about health and to help the patient understand how important it is to take care of themselves, such as managing their personal hygiene. The staff also work a lot with the patients to make them understand how they can cope independently with activities in daily life. The staff work with helping and motivating the patient's in different ways, like increasing their activity level and helping patients feel more confident. The patient will start with an easy activity and move on to a more difficult activity when the staff notices an improvement in the patient process skills.
“[...]Because some patient do not know how to take care of themself and so the nurse will take care of them and make sure they have the personal hygiene." - Interview 2
5.3 Lack of individual goal setting
According to the respondents they do not set individual goals in consultation with the patient. They observe the patient in general without the patient's knowledge and they usually focus on the patient’s personal hygiene.
5.3.1 Setting goals without knowing what the patient wants to achieve
The general goal for the patients is to make them happy and have them live a normal life which for them means good health and being able to work. How the staff set goals on the patient depends on the patient's daily status. The staff focuses on making the patients healthy again, not on the patient's abilities and weaknesses. The staff does not have any specific goal for each patient, and they do not form goals in consultation with the patient. According to the respondents, the priority goal is focused on the patient's hygiene and if they can take their medication by themselves.
“We don’t have specific goals in general”– Interview 1
5.3.2 Knowing when the patient achieves improvement by observation
A lot of the respondents did not know what a goal is and how to use it in the rehabilitation process. As written under “Lack of individual goal setting” the main goal for the patient is to make them happy again and have them live a normal life. According to the respondents they see improvement by observing the patient in different tasks, but mostly to see if the patient can manage their hygiene and interact with other patients. To see if a patient achieves any improvement, the staff sees if the patient looks happy and is being social and engaged in the activities. They also let the patient do different tasks, starting with easy tasks to more difficult tasks and this is how they see improvement.
“We need to observe the patient. Like the body hygiene, we observe every day. If the patient can make themselves clean or not. If the patient cannot we have to teach the patient step by step”
12
6. Discussion of the findings
6.1 Discussion of the methodology
6.1.2 Participants and requirement
The inclusion criteria to participate in the study were set before the trip to Vietnam. One inclusion criterion was for the participants to be of different professions and this is according to Kristensson (2014), to get a varied sample of the representatives. The collection of participants was supposed to be a purposive sampling where the participants were consciously recruited. Since the Corona Virus Disease- 19 [COVID-19] arose when this study was conducted, it is of relevance to explain it since it affected the requirement of the participants. Due to the current situation that arose, time became scarce and participants from the exclusion criteria needed to be interviewed to conduct 10 interviews. This led to the interpreter selected participants based on who was available and hade time to be interviewed, and therefore assistant nurses had to be interviewed.
6.1.3 Interview guide
Before the trip to Vietnam, an interview guide was designed with questions related to the purpose of the study. When arriving in Vietnam, other questions arose that were more interesting to ask about and that fit better into the purpose of the study. There were now questions that were no longer relevant and instead other questions that suited the situation better. Some of the follow-up questions in the interview guide were not developed to give detailed answers, so there were many short answers. Although many answers were short or in some cases absent, some answers could be linked to the study's purpose which were of interest. The interview questions could have been better prepared by having other questions that provided more elaborate answers that do not require any follow-up questions. This could have been done by searching for relevant articles or studies that have been done in the past to be more prepared for the scenario. Some questions were difficult to understand for the participants, and this led to other questions could not be answered correctly since they did not understand the question.
However, this could have been avoided by preparing two different interview guides, one with the project's thematic research questions and one with the questions to be posted.
This is because the research question is often written in a theoretical language and the interview questions should, therefore, be formulated in the everyday language of the interviewees (Kvale & Brinkmann, 2009). By using this strategy, any misunderstandings could have been avoided.
6.1.4 Data collection
A lot of unexpected things happened that affected the data collection. The room where the interviews where held, were located in the building where the patients resided. This turned out to be a poor location since it was very noisy outside the room and sometimes other health care staff walked in during the interviews. According to Kristensson (2014) it should be the respondents who decide the location of the study, preferably in a secluded room with no interruptions. Even though it was the respondents who picked the location, a quieter room would be preferable. Due to Covid-19, everyone in the clinic had to wear a face mask and because of this, the facial expression could not be seen during the interviews. It was difficult to see how the respondents reacted to the questions.
An interpreter was present during the interviews and helped translate the questions and the answers. One thing that needs to be considered is that the interpreter works as a pediatric doctor at the clinic and is familiar with the clinic and the staff. This can lead to the interpreter translating the answer based on his own experiences and interpretations. Sometimes the interpreter did not quite understand the questions and therefore the translation to the participants became wrong and this led to that the answers were not quite correct either. Some questions had to be explained by an example for both the interpreter and the respondent during the interview. The interviews were recorded but notes were also taken, and this turned out to be a wise choice since a lot of the answers were hard to hear on the recorder because of the noise outside. This made the transcription a little complicated, but the notes were very helpful during this phase. Due to the avoidable circumstances and things that needed to be rearranged, data was collected and could be used in the study.
13
6.1.5 Data analysis
Since there was a preunderstanding from a previous study, the result may have been affected. This was tried to be avoided by using triangulation which according to Kristensson (2014), means that two or more are analyzing the data together.
To increase the verifiability and reliability, the interviews were read through individually but then discussed to get a common impression and context of the material.
To not miss information during the data analysis that is of importance to the study, it is significant to stick to the study’s purpose and contain the relevant information. To increase the study's confirmability, quotes from the interviews are used to reinforce the results (Kristensson, 2014).
In some cases, the answers were not valuable as they did not have the proper intention towards the interview questions, for example the question of which assessment instrument is being used when investigating their patients. The fact that these answers are not useful may be due to differences in health care in Sweden and Vietnam. There are unavoidable differences between the participants' responses and the interpreter's summary of the participant's responses when conducting the interviews. Participants' responses were very long and were broadly discussed between the interpreter and the participant, while the interpreter's summary was very brief and concise. Interpretation may involve rephrasing or clarification of an answer that can lead to a misunderstanding and this could lead to a deceptive result (Kvale & Brinkmann, 2009).
Using an interpreter could have affected the results since the participants answers may not have been presented correctly and meaningful sentences may have been sorted out by the interpreter.
6.2 Discussion of the Results
The revealing of the results showed that the health care staff at the clinic do not use any standard procedures when evaluating and assessing their patients. But, the staff has found their own structure and strategies and are working from their own experience. They do have interviews and ask questions to the patient depending on the patient's diagnosis and daily status. Observations are made to see if a patient is getting better.
Along with this they only focus a little on the patient as an individual since they do not offer any individual treatment, only group interventions. To decide what occupation treatment a patient should have they have a team meeting but in the end it's the doctor who decides what treatment each patient should have. The discussion of the results will be focused on the findings regarding the evaluation and assessment of the patient and how to work client-centered.
6.2.1 Individual treatment using a client-centered perspective
The clinic offers a lot of group therapy interventions such as workout at the gym, gardening, cook dinner, clean the beach, and go to the supermarket. Several studies have shown that group therapy has many positive outcomes for individuals suffering from mental illness. A study by Fieldhouse (2003) showed that the participants valued group therapy in the natural environment, such as being outdoors in a green environment, which provided a sense of peacefulness by being away from ordinary stressors. According to (Eklund et al., 2010) being part of social interaction is a fundamental aspect of everyday life and contributes to being a part of society. Group therapy is a common intervention for occupational therapists and focuses on a specific occupation. By using group therapy as an intervention, different types of social contexts can be practiced. It also provides an opportunity for the participants to share their experiences with others (Eklund et al., 2010).
As mentioned in the result, under “5.2 Different occupation-based interventions offered at the clinic”, the clinic does not offer any individual therapy. This can be a disadvantage for the patients. Individual contact may be necessary at the beginning of therapy if the patient is not matured enough to join a group with other participants. Individual contact is individualized, and the treatment can focus directly on the patient's needs. It is also an opportunity for the occupational therapist to get to know the person, create a good alliance, or perhaps make a special assessment of the patient during the occupation (Eklund et al., 2010). The staff do have induvial contact with the patient, but it is only in the beginning when the patient arrives to the clinic.
14
Client-centered practice requires that occupational therapists develop a relationship with their patient and then work together with the a respectful way that considers the patient’s values, choices, and own perspective. A therapeutic relationship is built on mutual trust, a non-judgmental perspective, and respect.
Working together with the patient means that the occupational therapist sees the patient as an equal partner who is actively involved in their own occupational therapy process (Fisher & Marterella, 2019). The finding from the result showed that an occupational therapist could contribute to a more individual-based treatment.
6.2.2 Evidence-based evaluation and assessment of the patients
In the result it was clear that the health care staff do not use any evidence-based or structured evaluation or assessment instruments. Although, the staff expressed a great desire to be able to use evaluation instruments to make better assessments on their patients.
The first phase in rehabilitation is an assessment of the patient where the staff collects a baseline from the patient to identify strengths and needs. An assessment is also necessary to be able to evaluate the effectiveness of a specific treatment intervention (Mohammed Alotaibi et al., 2009). Since there is no routine or standard procedure for evaluating and assessing the patients' abilities and disabilities at the clinic today, standardized instruments can be used to promote the work of evidence-based practice (Romli et al., 2019). Evidence-based practice [EBP] has become a priority in modern mental health occupational therapy and is an important driver (Hitch, 2016). EBP is a process that health care uses that is about research and clinical experience applied in clinical contexts (Fristedt et al., 2016). This is to bring out the best care resources and the most effective interventions for the patients. It may prove unethical to not offer patients the latest and most appropriate research (Fristedt et al., 2016). Several strategies can be used when assessing a patient to gather information about the patient. The first stage of the assessment is an interview, the other strategies include instruments, questionnaires, and observations. These assessments provide information about the patient's past and present capacity, their ability to perform a task, their thoughts on their abilities, and motivation.
The staff at the clinic do perform interviews and observation, but using different instrument could be used to get a broader picture of the patients’ abilities and disability, and their current situation.
Instruments that can be applied in practice and collect valuable information about patients in psychiatry can be the instrument Satisfaction with Daily Occupation [SDO] (Wästberg et al., 2016). This is a tool for patient evaluation in mental health care. SDO can help to get a wider picture of the patient and the patient's self-assessment of valuable activities. It can also help to set goals for the patients. Canadian Occupational Performance Measure [COPM] (Law et al., 2016) is used when the patient indicates up to five activities that the patient has problems in everyday life. These are ranked and the patient then estimates them based on two aspects - the quality of the performance and satisfaction with the performance of the occupation (Eklund et al., 2010). Occupational self-assessment [OSA] (Baron et al., 2019) is a person-centered self-assessment tool that allows the person to express their view of their occupation ability and the influence of the environment on their daily activities. In this instrument, they give the patient the opportunity to indicate how important an occupation is and to set a priority order for changes. Another instrument is Occupational Circumstances Assessment Interview and Rating Scale [OCAIRS] (Forsyth et al., 2017). This is an instrument that provides a structure for systematically collecting, assessing, and analyzing information about a patient’s occupation situation and participation in daily life (Taylor & Kielhofner, 2017).
These assessment tools are used to gather information about the ptient's abilities. Using these instruments, the patient's strengths and weaknesses can be mapped, and detailed information about the patient's actual performance. Using structured assessments could contribute to evidence-based therapy (Taylor & Kielhofner, 2017). For an occupational therapist to use the benefits of an assessment, it is important to choose an appropriate assessment matched with the patient's situation. Selecting an appropriate assessment tool can contribute to the patient's treatment plan (Mohammed Alotaibi et al., 2009). According to the findings, an occupational therapist and the knowledge about evidence-based instruments could be of great use at the clinic.
15
6.2.3 Goal-setting
It was discovered in the result that the clinic has a lack of knowledge about goal-setting. When discussing the question about goal-setting, it was difficult for the respondents to understand. In the end, the common answer to the question was that the general goal for the patient is to be able to manage their hygiene. The health care staff also use observations without aim to see if the patients look healthy and happy, and this is how they achieve improvement.
The assessment of the patient is a part of the therapeutic process since it decides the treatment intervention based on the patient's assessed strengths and weaknesses to formulate a specific goal (Mohammed Alotaibi et al., 2009). It was discovered in the result that staff do not use any specific assessment instruments and therefore they have difficulty to formulating individual goals for their patients.
Through collecting information about the patient with help from instruments, the information can be used as a tool to formulate a goal-setting together with the patient (Eklund et al., 2010). To have an evidence-based practice it is essential to document the patient's baseline and goals. Without a baseline and a goal, the occupational therapist cannot document and evaluate the outcomes of occupational therapy interventions. The baseline and the goals must be documented before any occupational therapy interventions are implemented. The components of an occupation-focused goal include how well the patient will be able to perform an occupation and what the patient will be able to do. The occupational therapist needs to collaborate with the patient to establish a goal since most patients do not have experience writing or formulating goals (Fisher & Marterella, 2019). The benefits of goal setting have been shown to increase a person's motivation and changed behavior (Wade, 2009).
The knowledge about goal-setting that an occupational therapist possesses, can be of great benefit to the clinic and their patients since it has a major impact on a patient’s recovery.
6.2.4 How occupational therapy practices can benefit to the clinic in Vietnam
The clinic could be in use of an occupational therapist and take advantage of the knowledge an occupational therapist can provide. An occupational therapist is well known with evidence-based assessments which could contribute to qualitative and evidence-based treatment and interventions. EBP has become a priority in mental health occupational therapy and this gives the opportunity to strengthen the occupational therapist's role and profession (Hitch, 2016, Eklund et al., 2010). Within psychiatry it has for a long time been a focus on medical treatment rather than focusing on the individual as a competent person. Now, the value of occupation in health care is instead noticed and appreciated (Eklund et al., 2010). An occupational therapist has a broad knowledge of occupation-based interventions, and this could be of benefit at the clinic to provide suitable occupation-based interventions for the patients. According to Eklund et al., (2010), patients need meaningful activities that can contribute to their rehabilitation and recovery. The occupational therapist can have an educational role at the clinic and educate the other staff about the findings of the study.
According to the Code of Ethics for Occupational Therapists in Sweden, occupational therapists have a responsibility when it comes to development work and research to disseminate their knowledge and work to the public (Sveriges Arbetsterapeuter, 2018). Ethical dilemmas are a common issue in occupational therapists’ daily work and can sometimes make it difficult to optimize the patient's participation regarding the decision- making. The occupational therapist needs to take into account to acting professionally and respecting the patient’s wishes and integrity (Kassberg & Skär, 2008).
6.2.5 Recommendations for further research
This study is a qualitative study with ten semi-structured interviews with health care staff at a psychiatric clinic in Vietnam. The conclusion of the analyzed data is that it can be determined that further studies are needed in this area and clinic. The study can be developed with a larger number of participants and with a more in-depth method and more detailed answers.
Outside the interviews a presentation about occupational therapy was performed to the staff at the clinic. The staff expressed a wish to learn more about evaluation and assessment and maybe a further study could measure the outcome of a certain assessment instrument that the clinic can try. They wanted an opinion on their work and on their occupation-based interventions and how they can improve the rehabilitation. The staff at the clinic expressed a great desire for continued research at the clinic and collaborations with other universities. They appreciated the work at the clinic and the opportunity to learn about the work process and a client-centered perspective and occupational therapy practice.
16
7. Conclusion
The study concludes that the health care staff at the clinic has found their own structure and strategies by using their own experience, for evaluating and assessing their patients. The result showed that they work without a standard procedure. The interviews and observations of the patients are made without an certain structure. Regarding the goal setting, the staff focuses on setting a general goal for the patients that are not individual. They do not set goals together with the patient to know what the patient wants to achieve and by using observation the staff can conclude of improvement. Although the clinic offers a lot of different based interventions, the choice of the occupation-training is not in consultation with the patient and is mostly decided by the doctor. The common purpose is to make the patient independent. The clinic does not use a client-centered perspective, even though the staff valuates a good relationship with the patient.
17
8. References
Al-Amer, R., Ramjan, L., Glew, P., Darwish, M., & Salamonson, Y. (2016). Language translation
challenges with Arabic speakers participating in qualitative research studies. International Journal of Nursing Studies, 54, 150–157.
Baron, K., Kielhofner, G., Iyenger, A., Goldhammer, V. & Wolenski, J. (2019). Min mening om olika
aktiviteter - självskattning av kompetens och värderingar (OSA-S), (L. Haglund, övers. och bearb.,
version 3.0). Nacka: Sveriges Arbetsterapeuter. (Occupational Self Assessment (OSA), version 2.2/2006).
Bhugra, D. (2016). Routledge handbook of psychiatry in Asia . New York: Routledge.
Causey, B., & Björn, L. (2019). ‘Help the patient turn back to happy’: A qualitative study with mental health professionals in Vietnam : A Bachelor of Science Thesis in Occupational Therapy about how mental health staff support their patients back into society, conducted as a Minor Field Studies project (Dissertation).
Creek, J., & Lougher, L. (2008). Occupational therapy and mental health (4. ed.). Edinburgh: Churchill Livingstone.
Crouch, R., & Alers, V. (2014). Occupational therapy in psychiatry and mental health (5. ed.). Chichester: Wiley-Blackwell.
Doig, E., Prescott, S., Fleming, J., Cornwell, P., & Kuipers, P. (2015). Development and construct
validation of the Client-Centredness of Goal Setting (C-COGS) scale. Scandinavian Journal of
Occupational Therapy, 22(4), 302–310. Retrieved from
Ekberg, K., Eklund, M., & Hensing, G. (2015). Återgång i arbete : processer, bedömningar, åtgärder . Studentlitteratur.
Eklund, M., Gunnarsson, B., & Leufstadius, C. (2010). Aktivitet & relation : mål och medel inom
psykosocial rehabilitering (1. uppl.). Studentlitteratur.
Erlandsson, L., & Persson, D. (2020). ValMO-modellen : arbetsterapi för hälsa genom görande (Andra upplagan).
Fieldhouse, J. (2003). The Impact of an Allotment Group on Mental Health Clients’ Health, Wellbeing
and Social Networking. The British Journal of Occupational Therapy, 66(7), 286–296.
Finlay, L. (2004). The practice of psychosocial occupational therapy (3. ed.). Cheltenham: Nelson Thornes.
Fisher, A. G., & Marterella, A. (2019). Powerful practice: A model for authentic occupational therapy.
Fort Collins, CO: Center for Innovative OT Solutions.
Forsyth, K., Deshpande, S., Kielhofner, G., Henriksson, C., Haglund, L., Olson, L., Skinner, S., & Kulkarni, S. (2017). Bedömning av delaktighet i aktivitet (OCAIRS-S), (L. Haglund, övers. och bearb., version 2.2). Nacka: Sveriges Arbetsterapeuter. (The Occupational Circumstance
Assessment-Interview and Rating Scale (OCAIRS), version 4.0 (2005)."
Fristedt, S., Areskoug-Josefsson, K., & Kammerlind, A. (2016). Factors influencing the use of
evidence based practice among physiotherapists and occupational therapists in their clinical work. Internet Journal Of Allied Health Sciences &Amp; Practice, 14(3), 1–13.
Gaebel, W., Zäske, H., Cleveland, H-R., Zielasek, J., Stuart, H., Arboleda-Florez, J., … Sartorius, A. (2011). Measuring the stigma of psychiatry and psychiatrists: Development of a questionnaire.
European Archives of Psychiatry and Clinical Neuroscience. 261 (2). pp 119- 123.
18
Graneheim, U., & Lundman, B. (2004). Qualitative content analysis in nursing research: concepts,
procedures and measures to achieve trustworthiness. Nurse Education Today, 24(2), 105–112.
Hayashi, Y. (2010). Service development to meet the needs for rehabilitation in the community in
Vietnam. World Federation of Occupational Therapists Bulletin. 61 (1). pp 39- 44. DOI:
10.1179/otb.2010.61.1.01
Hitch, P.D. (2016). Attitudes of mental health occupational therapists toward evidence-based practice.
Canadian Journal of Occupational Therapy = Revue Canadienne D’ergothérapie., 83(1), 27–32.
Höglund-Nielsen, B., & Granskär, M. (2017). Tillämpad kvalitativ forskning inom hälso- och
sjukvård (Tredje upplagan). Studentlitteratur.
Kassberg, A., & Skär, L. (2008). Experiences of ethical dilemmas in rehabilitation: Swedish
occupational therapists’ perspectives. Scandinavian Journal of Occupational Therapy, 15(4), 204–
211.
Kristensson, J. (2014). Handbok i uppsatsskrivande och forskningsmetodik för studenter inom hälso-
och vårdvetenskap (1. utg.). Natur & Kultur.
Kvale, S., & Brinkmann, S. (2009). InterViews : learning the craft of qualitative research
interviewing (2. ed.). Los Angeles: Sage Publications.
Lannigan, E., & Noyes, S. (2019). Occupational Therapy Interventions for Adults Living With Serious
Mental Illness.(Evidence Connection). AJOT: American Journal of Occupational Therapy, 73(5),
7305395010p1–7305395010p5.
Lauber, C., & Rössler, W. (2007). Stigma towards people with mental illness in developing countries in
Asia. International Review of Psychiatry, 19(2), 157-178.
Lipskaya-Velikovsky, L. Jarus, T. Easterbrook, A. & Kotler, M. (2016). Participation in daily life of
people with schizophrenia in comparison to the general population. Canadian Journal of Occupational Therapy. 83 (5). DOI: 10.1177/0008417416647158
"Law, M., Baptiste, S., Carswell, A., McColl, M.A., Polatajko, H., & Pollock, N. (2016). Canadian Occupational Performance Measure (COPM), (K. Samuelsson, A. Bergström & A. Carlsson, övers. och bearb., 5:e upplagan). Nacka: Sveriges Arbetsterapeuter. (Originalet: Canadian
Occupational Performance Measure (COPM), 5th ed. (2014).
Malcus-Johnson, P., Carlqvist, C., Sturesson, A., & Eberhardt, K. (2005). Occupational therapy during
the first 10 years of rheumatoid arthritis. Scandinavian Journal of Occupational Therapy, 12, 128–
135.
Mohammed Alotaibi, N., Reed, K., & Shaban Nadar, M. (2009). Assessments Used in Occupational
Therapy Practice: An Exploratory Study. Occupational Therapy In Health Care, 23(4), 302–318.
Mårtensson, L., & Archenholtz, B. (2017). Occupational therapists’ perceptions of habits based on their
professional experiences. Scandinavian Journal of Occupational Therapy, 24(2), 151–159.
https://doi.org/10.1080/11038128.2016.1227368
Ottosson, H., & Ottosson, J. (2007). Psykiatriboken (1. uppl.). Stockholm: Liber.
Romli, M., Wan Yunus, F., & Mackenzie, L. (2019). Overview of reviews of standardised occupation‐
based instruments for use in occupational therapy practice. Australian Occupational Therapy Journal, 66(4), 428–445.
https://doi.org/10.1111/1440-1630.12572
Styrelsen för Internationellt Utvecklingssamarbete [The Swedish
International Development Cooperation Agency [SIDA]. (2017). Sidas stipendier och praktikprogram. https://www.sida.se/Svenska/engagera-dig/sidas-stipendier-och-praktikprogram/