Effects of COPD self-care management education at a nurse-led
primary health care clinic
Eva O
¨ sterlund Efraimsson
RN, MSc (Doctoral Student),Charlotte Hillervik
PhD (Assistant Professor) andAnna Ehrenberg
RN, PhD (Associate Professor and Post-Doctoral Fellow)Department of Health and Social Sciences, Ho¨gskolan Dalarna, Falun, Sweden
Scand J Caring Sci; 2008; 22; 178–185
Effects of COPD self-care management education at a nurse-led primary health care clinic
Chronic obstructive pulmonary disease (COPD) is disabling, with symptoms such as chronic cough, phlegm, wheezing, shortness of breath and increased infections of the respir-atory passage. The aim was to examine the effects of a structured educational intervention programme at a nurse-led primary health care clinic (PHCC) on quality of life (QoL), knowledge about COPD and smoking cessation in patients with COPD. This study had an experimental design in which 52 patients with COPD from a Swedish primary care setting were randomized into two groups (intervention or control). Both groups received standard care but patients in the intervention group were also offered two visits to a nurse specialized in COPD care. The purpose of the visits was to increase the patients’ self-care ability and their knowledge about COPD. The study was approved by the local Research Ethics Committee. Data were collected using two questionnaires, one pertaining to knowledge about COPD and smoking habits and St. George’s Respiratory
Questionnaire, addressing how QoL was affected by the patients’ respiratory symptoms. The intervention and con-trol groups answered both questionnaires on their first and last visits to the PHCC. A statistically significant increase was noted in the intervention group on QoL, the number of patients who stopped smoking and patients’ knowledge about COPD at the follow-up, 3–5 months after interven-tion. However, a confounding factor may have been that one of the researchers (Eva O¨ sterlund Efraimsson), as a nurse in the PHCC, performed the intervention. This im-plies that patients were in a dependent relationship which may have affected the responses in a favourable direction. Our findings show that conventional care alone did not have an effect on patients’ QoL and smoking habits. In-stead, the evidence suggests that a structured programme with self-care education is needed to motivate patients for life-style changes.
Keywords: experimental design, quantitative approaches, district nursing, patient teaching, primary care.
Submitted 31 August 2006, Accepted 26 March 2007
Introduction
Chronic obstructive pulmonary disease (COPD) is a pro-gressive inflammatory pulmonary disease characterized by chronic obstruction in the peripheral bronchus and pul-monary emphysema. The disease is disabling, with symp-toms such as chronic cough, phlegm, wheezing, shortness of breath and increased infections of the respiratory pas-sage. In addition, severely ill patients with COPD often have other symptoms, including congestive heart failure, brittleness of the bones, muscular weakness, malnutrition,
weight loss, cognitive dysfunction, fatigue and depression (1, 2).
COPD, now the fourth leading cause of death in the world, continues to increase in the developing countries. The World Health Organization (WHO) expects COPD to be the third most common cause of death in the world by 2020 (3). The mortality varies in different countries, where it is related to the prevalence of smoking in the population. Mortality is high in China, Mongolia, Eastern and Central Europe, the United Kingdom, Ireland, Australia and New Zealand (4). In Sweden, it is estimated that 8% of the population over 50 years of age suffer from COPD and 25– 30% of the smokers develop the disease, with increased risk in higher ages. About 50% of smokers above 75 years of age are affected by COPD (5). The disease costs the Swedish society more than 1.1 billion USD per year (6).
Because smoking is the greatest risk factor for COPD, smoking cessation treatment is a prioritized intervention.
Correspondence to:
Eva O¨ sterlund Efraimsson, Department of Health and Social
Sciences, Ho¨gskolan Dalarna, SE-791 88 Falun, Sweden. E-mail: eoe@du.se
Early smoking cessation improves the prognosis and leads to less severe symptoms (1, 2). Professional counselling has proven to have a positive affect on smoking habits, as well as counselling with repeated visits (1, 2, 7). Such psycho-social interventions for smoking cessation have shown significantly better outcomes when combined with phar-macological treatment as compared with only psycho-so-cial interventions or no intervention (8).
Research indicates that physiological, psychological and social aspects of quality of life (QoL) are affected in patients with COPD (1, 2). For instance, physical exercise, brea-thing and coughing technique, relaxation and pelvic muscle exercise are all known to improve activity toler-ance and thus improve the individual’s QoL (9). Moreover, increased physical activity is conducive to good fitness and can compensate for reduced pulmonary function in pa-tients with moderate COPD (1, 2). Papa-tients can be sup-ported to live a life that is more health promoting by helping them survey and structure their daily activities. Such rehabilitation programmes have been found to im-prove physical performance, decrease dyspnoea and greatly enhance QoL (10).
Dietary counselling can counteract weight loss as well as promote well-being and reduce dyspnoea (1, 2). This is important in that weight loss is known to affect the pro-gression of the disease (11, 12). A qualitative study of COPD patients’ experiences of eating showed that dietary issues cannot be considered only as a physiological matter but also as a complex psycho-social problem (13). There-fore, it is vital that health care personnel have skills in the areas of nutrition and eating in order to support patients with COPD that suffer from weight loss (13).
The role of the Swedish primary health care system is to detect, diagnose, treat and evaluate COPD, all of which is done to prevent deterioration of the disease. The aim is to decrease symptoms, improve QoL and increase physical and social activity in the daily life of these individuals. Primary health care should also provide smoking cessation programmes (1, 2). Patient education is an important ele-ment in clinical guidelines for COPD care (1, 2, 14). In this direction special nurse-led COPD clinics have developed within Swedish primary health care during recent years, with a primary focus on support for self-care and smoking cessation. Approximately 50% of primary health care units in mid-Sweden have developed such clinics (15). In con-ventional care patients with COPD see their physician (general practitioner) for health examinations and deteri-oration of the disease. In contrast to visits to the nurse, physician visits are for the most part limited in time and scope, where focus is often restricted to pharmacological treatment of the disease. According to clinical experience and research, compliance in patients with chronic diseases is improved by structured treatment, patient education, regular check-ups (11, 16, 17) and specially educated health care professionals (18). Accordingly, nurse-led
clinics for COPD are tested and recommended in Swedish health care, but have not yet been the subject to rand-omized controlled trials (2).
The aim of this study was to examine the effects of a structured educational intervention at a nurse-led primary health care clinic (PHCC) on QoL, knowledge about COPD and smoking cessation in patients with COPD. The study had an experimental design, i.e. a comparison of conven-tional treatment (control group) and an educaconven-tional intervention (intervention group) to support patients’ self-care ability at a nurse-led COPD clinic.
Materials and methods
The study population consisted of all patients with sus-pected COPD (n = 110) that were referred to the COPD nurse at a PHCC in a mid-Swedish municipality during the period January to October 2004. Data collection was per-formed during a 10-month period in which patients were included consecutively upon referral. The inclusion criteria were patients diagnosed with mild, moderate, severe or very severe COPD based on spirometry, lung capacity after bronchodilator use, based on the GOLD criteria (1). Pa-tients with diagnosed severe mental disorders such as schizophrenia, dementia or alcohol or drug abuse were excluded. Patients with anxiety and depression were not excluded.
After excluding 48 patients not diagnosed with COPD (none excluded by exclusion criteria), 62 patients were invited to join the study with 52 accepting to participate. Patients were matched based on gender and the severity of COPD and then randomized into the intervention or control group when a matched pair was identified (Table 1). The randomization was performed when two patients with the same variables agreed to participate in the study by assigning each individual an identity number. An independent person drew lots for allocation to either
Table 1 Distribution of patients (n = 52) in the intervention and control groups as a function of gender and severity of chronic obstructive pulmonary disease (COPD)
Patient characteristics Intervention group Control group Total
Women (n = 13) (n = 13) (n = 26)
Mild COPD 2 3 5
Moderate COPD 3 3 6
Severe COPD 3 2 5
Very severe COPD 5 5 10
Total 13 13 26
Men (n = 13) (n = 13) (n = 26)
Mild COPD 3 2 5
Moderate COPD 6 6 12
Severe COPD 3 3 6
Very severe COPD 1 2 3
intervention or control group. The sample included 26 women and 26 men, with a mean age of 68 (SD = 9.7) and 66 years (SD = 11.4) for women and men, respectively. The mean age for the control group was 67 years (SD = 10.4) and for the intervention group 66 years (SD = 9.4). Co-morbidity was similar in the two groups, including diseases such as cancer, diabetes and heart dis-ease.
The drop-out rate was 10 patients (five women and five men), with a mean age of 66 years (SD = 5.6). Of these 10 patients, three were smokers (two women and one man) and seven were ex-smokers. The severity of the illness was evenly distributed between men and women: three wo-men and three wo-men had moderate COPD, one woman and one man had severe COPD and one woman and one man had very severe COPD. The drop-out group did not differ from the sample in any of these aspects.
Instruments
Two questionnaires were used for data collection: St. George’s Respiratory Questionnaire (SGRQ) and a ques-tionnaire specifically developed for this study.
SGRQ, which has been used in several studies, is a dis-ease-specific instrument designed to measure impact of respiratory symptoms on overall health, daily life and perceived well-being. The instrument has shown good validity and reliability, with Cronbach’s alpha scores >80 (19). The questionnaire is divided into two sections. Section one includes frequency and severity of symptoms and part two covers activities that cause or are limited by breath-lessness and impact on social functioning and psychological disturbances resulting from airway disease. Responses in the first section are given on a 5-point Likert scale and in the second section as dichotomous variables (yes/no). Re-sults are reported in four sections: symptoms, activities limited by breathlessness, psycho-social impact and com-prehensive impact as a basis for the assessment of QoL. Each section is presented as a weighted score. Scores range from 0 to 100, with higher scores indicating poor health.
The second questionnaire contained questions on pa-tient characteristics, such as gender, age, marital status, education, knowledge about COPD and smoking habits. Patients’ knowledge was measured by a simple question: ‘How do you rate your knowledge about COPD?’ and responded to on an ordinal scale, ranging from very good to none. Data on smoking was collected by the question ‘Do you smoke?’ with dichotomous response alternatives (yes/no).
Procedure
Permission was given by the manager and physician in charge at the PHCC. The study was approved by the local Research Ethics Committee.
After referral to the nurse-led COPD clinic, patients were assessed by spirometry. Patients who were diagnosed as having COPD and fulfilled the inclusion criteria were invited by the nurse to participate in the study. Patients were provided with written information about the study. Further, they were informed about the voluntary nature of their participation and that they could withdraw from the study at any time. Informed consent was obtained from all patients.
All patients were scheduled for two visits to the COPD clinic, with a 3–5-month interval between the first and last visits. In addition, the patients in the intervention group had two visits for self-care education during these 3– 5 months. Each visit lasted for about 1 hour and the same nurse (Eva O¨ sterlund Efraimsson) was responsible for all consultations. At the first and last visits, all patients responded to the two questionnaires, which were com-pleted by each participant in an undisturbed area. The nurse in charge was available to answer questions and to check that the patients responded to all the items. The control group was given conventional care that included a first visit to the nurse, spirometry and a follow-up visit to a physician. After the termination of the data collection phase of the study, patients in the control group were invited to self-care educational visits to the COPD nurse.
Intervention
Patients in the intervention group received education with an emphasis on self-care ability and how to support the individual based on his or her unique requirements and abilities to cope with disease and treatment (2, 10, 11). The educational visits were based on motivational dialogue, tailored for each patient based on severity of illness, age, intellectual capacity and life style, with the following main components:
- Description of the anatomy and physiology of the air-ways and the effects of COPD.
- Measurement of respiratory function (spirometry) and explanation of the outcome to the patient.
- Optimization of pharmacological treatment and control of the inhalation technique. Explanation to patients of when, how and why they should take their medications. - Instructions on the coughing technique to prevent infections and exacerbations.
- Motivational dialogue on smoking cessation based on Prochaska and DiClementes’ transtheoretical model of the stages of change (20). The model is based on open ques-tions to help patients reflect on their smoking habits and empower patients to quit smoking.
- Instructions on how patients should deal with acute exacerbations.
- Measurement of oxygen saturation (pulsoximetry) be-fore and after exertion.
- Assessment and instruction of breathing technique and relaxation. Patients were instructed how to cope with respiratory problems, especially during exertion. In order to visualize the correlation between breathing technique and oxygen saturation training of the breathing technique during and after exertion was given with simultaneous pulsoximetry.
- Dialogue on physical activity and exercise.
- Dietary counselling was intensified in patients with very severe COPD. Patients received information on nutritional supplements and were referred to a dietician.
- Psycho-social counselling and support. - Counselling on infection prevention.
- Individual treatment plan in collaboration with the pa-tient, including how patients should adjust medication on exacerbation and when to consult the physician.
The intervention programme was accomplished in col-laboration among patients, the COPD nurse and the phy-sician. When needed, a dietician, a medical social worker, a physical therapist and an occupational therapist were consulted. In the intervention group there were 16 pa-tients who had their medication changed. Three papa-tients had an extra visit to the physician, two were referred to a medical social worker, two to a dietician, physical therapist and occupational therapist, respectively. In the control group, no patients had their medication changed. One patient had an emergency visit to the PHCC, one had a telephone consultation and one had a planned visit to the physician.
Analysis
Hypothesis testing of effects on QoL was performed by the Mann-Whitney U-test. Effects on smoking cessation and patients’ knowledge about COPD were computed by Fisher’s exact test. Significance levels at p < 0.05 were accepted, and clinical relevance was accepted if there was a difference of the means within and between groups of four weighted units, which is in accordance with the SGRQ manual (21).
Results Quality of life
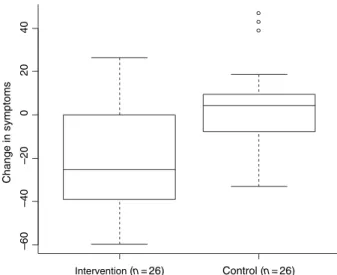
As depicted in Fig. 1, patients in the intervention group perceived a reduction in symptoms of cough, phlegm, dyspnoea and wheezing with an average value of 25.2 units (from 53.4) and no change was observed in the control group. The difference between the intervention and control groups was clinically relevant according to the SGRQ manual and statistically significant (p = 0.00035).
Patients in the intervention group reported increased activities (e.g. managing hygiene, clearing away snow and performing physical exercise) that reduced their dyspnoea.
The average value of this change was 5.6 units (from 42) (Fig. 2). The patients in the control group did not report any improvement. The difference between the groups was significant (p = 0.0267) and clinically relevant.
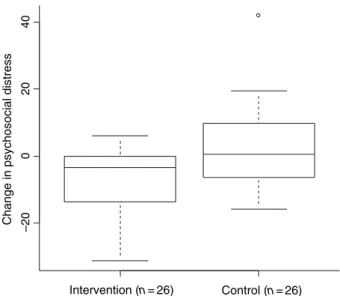
A decreased impact of COPD on psycho-social health (based on median value) by an average value of 3.4 units (from 19) was noted among patients in the intervention group (Fig. 3). There was no change for patients in the control group. The difference between the groups was clinically relevant and statistically significant (p = 0.0161). QoL was improved by an average value of 8.2 units (from 30.6) in the intervention group, whereas no change was noted in the control group. The difference between the groups was significant (p = 0.00030) and clinically relevant (Fig. 4). Intervention (n = 26) –60 – 40 –20 0 2 0 4 0 Control (n = 26) Change in symptoms
Figure 1 Patients’ perceived symptoms before and after intervention.
Intervention (n = 26) –30 –20 –10 0 1 0 2 0 3 0
Change in activities restricted by dyspnoea
Control (n = 26) Figure 2 Patients’ perceived restrictions in daily activities because of dyspnoea before and after intervention.
Smoking
In the intervention group (n = 26) 6 of the 16 (or 37.5%) patients who were smokers had stopped smoking during the intervention phase. In the control group (n = 26) none of the 14 smokers stopped smoking. The difference be-tween the groups was significant (p = 0.0185).
Knowledge about COPD
Patients in the intervention group reported an increase in knowledge about COPD, whereas no such increase was observed in the control group (Table 2). At baseline, no
difference between the groups regarding knowledge of COPD was noted, but there was a significant difference post intervention (p < 0.001).
Discussion
The findings of this study show significant effects of the educational intervention on patients’ perceived QoL, smoking cessation and knowledge about their disease. Patients in the intervention group reported a reduction in respiratory distress symptoms, increased physical activity and improved psycho-social health. In the intervention group, 6 of 16 patient smokers stopped smoking during the intervention whereas none in the control group stopped smoking. Furthermore, patients reported improved knowledge about COPD after the intervention programme. Patients in the intervention group reported decreased breathing problems (from 53 to 25 units) as measured by the SGRQ. The patients’ ability to influence and cope with dyspnoea, cough and phlegm by using medications and coughing and breathing techniques is crucial for their perceived QoL. Research has shown that patients with COPD may benefit considerably from knowledge on how to handle pharmacological treatment, dyspnoea and ex-acerbations [14]. Seemungal et al. (22) found that only 50% of exacerbations in patients with COPD were reported to their physician, which supports the notion that patients need knowledge to enhance their awareness on when to seek medical care (22).
We presume that an explanation for patients’ improved QoL in our study is the combined self-care education based on a structured programme and the individual written treatment plan (1, 2, 10). This connection has also been shown in previous studies, as for example by Worth and Dhein, who showed a significant improvement in inhala-tion technique, self-care and decreased exacerbainhala-tions after structured educational intervention (23). In another study, in which conventional care was compared with group education and individual consultations by nurses and physiotherapists, improved health and reduced health care costs for the intervention group were reported (14). In a
Intervention (n = 26) –20 0 2 0 4 0 Control (n = 26)
Change in psychosocial distress
Figure 3 Patients’ perceptions of the impact of respiratory problems
on psycho-social activities before and after intervention.
Intervention (n = 26) –30 –20 –10 0 1 0 2 0 3 0 Control (n = 26)
Change in the impact on quality of life
Figure 4 Patients’ perceptions of quality of life as based on the
weighted total change of symptoms, activities and psycho-social function.
Table 2 Patients’ (n = 52) reported knowledge on chronic obstructive
pulmonary disease (COPD) before and after the educational intervention
Perceived knowledge about COPD
Intervention group Control group
Before (n = 26) After (n = 26) Before (n = 26) After (n = 26) No knowledge 8 0 10 8 Limited knowledge 14 7 13 13 Good knowledge 4 17 2 4
Very good knowledge 0 2 1 1
third study individual self-care education, in combination with a written individual treatment plan, resulted in de-creased hospital re-admissions, unplanned physician visits, sick leaves and nocturnal symptoms in patients with COPD (24).
Another contributing factor to account for the positive outcome may be the trusting relationship that was estab-lished between the nurse and the patients. Problems with patients lacking adherence to treatment regimen is well known in patients with chronic diseases. To improve pa-tient compliance health care personnel need to show re-spect for the patients’ opinions and keep an open dialogue (25). Self-care education of patients improves patient compliance and responsibility to manage their disease (18).
The findings of our study indicate that using spirometry was an effective educational device for smoking cessation. By motivational dialogue and information on the impact of smoking on pulmonary tissue, about one-third of the smoking patients in the intervention group were able to quit smoking. The spirometry displayed the patients’ de-creased pulmonary capacity, which probably enforced and helped to explain their perceptions regarding shortness of breath. This conclusion is confirmed by DeJong (26), who showed that nurse-led screening with spirometry and patient education helped patients to stop smoking or seri-ously considering stopping. Patient information has pre-viously shown positive effects on smoking cessation (1, 2). Convincing effects of nurse-led clinics in patients with chronic diseases have mostly been attributed to the effects of patient education and responsibility for their own care (11, 16, 17). As indicated in our study, these studies show an improvement in the ability of patients to cope with their disease and daily life activities when supported by struc-tured self-care programmes. In our study the nurse-led clinic involved collaboration between the patient, the nurse and the physician. Other health care professionals (e.g. dietician, medical social worker, physiotherapist and occupational therapist) also contributed to the care of the patients when needed. This multi-professional teamwork was available for patients with specific needs and might have had an impact on the outcomes for patients suffering from severe or very severe COPD.
In a review of studies on nurse-led COPD clinics there were no significant differences in comparison with con-ventional care. Among the reviewed studies were those on hospital care, out-patient clinics and community-based homecare led by nurses, and the variables studied included health-related quality of life (HRQoL), mental health, disability, respiratory function and number of hospital admissions. One of the studies with a more structured programme found decreased hospital admissions in pa-tients in the intervention group. However, there were no data on patient satisfaction, self-care ability or compliance (27). Because of scant descriptions of the interventions, it
is possible that the outcomes are attributed to a lack of structure of the intervention programme. In another re-view, self-care education in COPD patients was compared with conventional medical care at an out-patient clinic. Patients in the intervention group increased their inhala-tion and antibiotics medicainhala-tion and their acute medical needs were reduced, indicating that patients who receive self-care education become more aware and observant of their symptoms. However, there were no effects on fre-quency of hospital re-admissions, emergency care visits, sick leave and respiratory function (28).
Limitations
There are several important limitations of the data and alternative interpretations of our findings. For instance, concerning patient characteristics, no differences were observed between the intervention and control groups. However, in the patients who declined participation there were fewer patients who were smokers (3 by 10 in the drop-out group compared with 30 by 52 in the sample) and more patients with moderate COPD as compared with the participants (6 by 10 compared with 19 by 52). It is reasonable to believe that patients who already had quit smoking considered that they had done what was required to stop the progress of the disease. Further, patients with moderate COPD may have had few symptoms of the dis-ease and, therefore, lacked motivation to join the study. A confounding factor may have been that one of the researchers (Eva O¨ sterlund Efraimsson), as a nurse in the PHCC, performed the intervention. This implies that pa-tients were in a dependent relationship which may have induced social desirability and thus affected the responses in a favourable direction. Moreover, patients may have been affected by the ‘Hawthorne’ effect in the sense that they were given an individualized treatment programme and felt acknowledged in their disease state. The researchers are aware that a follow-up time close to the intervention might show better results than a longer fol-low-up time. Some of the patients that were randomized into the control group were disappointed, possibly affect-ing their responses in a negative direction.
Most patients were recruited from the PHCC where the intervention was carried out, a fact that may have entailed selection bias of patients. Because of the close collaboration between the COPD nurse and physicians, more patients were referred to the nurse-led clinic by the physicians at this PHCC. It can be assumed that physicians were more inclined to observe symptoms of COPD and, therefore, referred patients to the nurse-led clinic more often. It seems as though the intervention did encourage increased attention and early diagnosis of these patients. However, because of the relatively small sample and the possible selection bias, generalization of the findings must be treated with caution.
Conclusion
Our findings show that conventional care alone did not have an effect on patients’ QoL and smoking habits. In-stead, the evidence suggests that a structured programme with self-care education is needed to motivate patients for life-style changes, which supports previous findings and recommendations in clinical guidelines (1, 11, 14). From our findings, we believe that nurse-led COPD clinics in primary health care are cost-effective, which has previ-ously been demonstrated for asthma clinics (14). Studies have shown that patients were significantly more satisfied with nurse consultations compared with physician con-sultations in primary health care (29), and that patients’ participation in care planning increases their satisfaction (30).
Primary health care will have a pivotal role in caring for the increasing number of patients with COPD in the fu-ture. It is therefore important to continue research to further our knowledge about the most effective methods for early detection, treatment and care of these patients. We believe that nurse-led clinics are a viable alternative in organizing COPD care in PHCC (14,15). Nurses specialized in COPD care and patient education are needed to meet the specific needs of these patients, as well as to plan and implement care. Studies on the effects of nurse-led clinics in PHCC are scarce (2). Therefore, larger randomized controlled trials of such clinics are called for, with partic-ular focus on the effects of self-care educational pro-grammes on life-style changes, self-care ability, compliance and QoL (11, 27, 28).
Acknowledgement
The authors wish to thank the patients who participated in the study.
Author contributions
O¨ sterlund Efraimsson has been involved in conception, study design, data collection, analysis, drafting of manu-script and revision. Hillervik has been involved in con-ception, study design, analysis, drafting of manuscript, revision and supervision. Ehrenberg has been involved in analysis, drafting of manuscript, revision and supervision.
Funding
This study was funded by the County Council of Dalarna, Sweden.
References
1 Pauwels RA, Buist SA, Calverley PMA. Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the
Diagnosis, Management, and Prevention of Chronic
Obstructive Pulmonary Disease: National Heart, Lung, and Blood Institute and World Health Organization Global Ini-tiative for Chronic Obstructive Lung Disease (GOLD).
Exe-cutive Summary Respire Care 2004; 46: 798–825.
www.goldcopd.com.
2 Svensk Lungmedicinsk Fo¨rening. Nationellt va˚rdprogram fo¨r KOL2003 (National guidelines for COPD). www.slmf.se. 3 Gulsvik A. The global burden and impact of chronic
obstructive pulmonary disease. Monaldi Arch Chest Dis 2001; 56: 261–64.
4 Murray C, Lopez A. Mortality by cause for eight regions of the world: Global Burden of disease study. Lancet 1997; 349: 1269.
5 Lundba¨ck B, Lindberg A, Lindstro¨m M, Ro¨nmark E, Jonsson A-C, Jo¨nsson E, Larsson L-G, Andersson S, Sandstro¨m T, Larsson K. Not 15 but 50% of smokers develop COPD? Re-port from Obstructive Lung Disease in Northern Sweden. Respiratory Med 2003; 97: 115–23.
6 Jansson S-A, Andersson F, Borg S, Ericsson A˚ , Jo¨nsson E,
Lundba¨ck B. Costs of COPD in Sweden according to disease severity. From the OLIN Studies. Chest 2002; 122: 1994–2002. 7 Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Tobacco Addiction Group. Cochrane Library 2005; 3: 1.
8 Meer RM, Wagena EJ, Ostelo RWJG, Jacobs JE, van Schayck CP. Smoking cessation for chronic obstructive pulmonary disease (Cochrane Review). Cochrane Library 2003; 4: 3. 9 Bellone A, Spagnolatti L, Massobrio M, Bellei E, Vinciguerra
R, Barbieri A, Iori E, Bendinelli S, Nava S. Short-term effects of expiration under positive pressure in patients with acute exacerbation of chronic obstructive pulmonary disease and mild acidosis requiring non-invasive positive pressure ven-tilation. Intens Care Med 2002; 28: 581–85.
10 Lacasse Y, Brosseau L, Milne S, Martin S, Wong E, Guyatt GH, Goldstein RS, White J. Pulmonary rehabilitation for chronic obstructive pulmonary disease (Review). Cochrane Library 2003; 1: 1–38.
11 Kara M, Asti T. Effect of education on self-efficacy of Turkish patients with chronic obstructive pulmonary disease. Patient Educ Counsel 2004; 55: 114–20.
12 Slinde F, Gro¨nberg AM, Engstro¨m CP, Rossander-Hulthe´n L, Larsson S. Individual dietary intervention in patients with COPD during multi-disciplinary rehabilitations. Respiratory Med 2002; 96: 330–36.
13 Odencrants S, Ehnfors M, Grobe SJ. Living with chronic obstructive pulmonary disease: Part 1. Struggling with meal-related situations: experiences among persons with COPD. Scand J Caring Sci 2005; 19: 230–39.
14 Gallefoss F. The effects of patient education in asthma and COPD: a randomised controlled trial. Lungeforum Scand Res-piratory J 2001; 11 suppl 14: 3.
15 Lisspers K, Sta¨llberg B, Hasselgren M, Johansson G, Sva¨rdsudd K. Organisation of asthma care in primary health care in Mid-Sweden. Primary Care Respiratory J 2005; 14: 147–53.
16 New JP, Mason JM, Freemantle N, Teasdale S, Wong LM, Bruce NJ, Burns JA, Gibson JM. Specialist nurse-led inter-vention to treat and control hypertension and hyperlipidemia
in diabetes (SPLINT): a randomized controlled trial. Diabetes Care 2003; 26: 2250–55.
17 Stro¨mberg A, Ma˚rtensson J, Fridlund B, Levin LA, Karlsson JE, Dahlstro¨m U. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart fail-ure: results from a prospective, randomised trial. Eur Heart J 2003; 24: 1014–23.
18 Gold DT, McClung B. Approaches to patient education: emphasizing the long-term value of compliance and persist-ence. Am J Med 2006; 119: 325–75.
19 Engstro¨m C-P, Persson L-O, Larsson S, Sullivan M. Reliability and validity of a Swedish version of the St George’s Ques-tionnaire. Eur Respiratory J 1998; 11: 61–66.
20 Prochaska JO, DiClemente CC. Stages of process of self-change in smoking: toward an integrative model of self-change. J Consult Clin Psychol 1983; 51: 390–95.
21 Jones PW. Interpreting thresholds for a clinically significant change in Health status in asthma and COPD. Eur Respiratory J 2002; 19: 398–404.
22 Seemungal TA, Donaldsson GC, Bhowmik A, Jeffries DJ, Wedzicha JA. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respiratory Crit Care Med 2000; 161: 1608–13.
23 Worth H, Dhein Y. Does patient education modify behaviour in the management of COPD? Patient Educ Counsel 2004; 52: 267–70.
24 McDonald VM, Gibson PG. Asthma self management edu-cation. Chronic Respiratory Dis 2006; 3: 29–37.
25 Stevenson F, Gerrett D, Rivers P, Wallace G. GPs recognition of, and response to, influences on patients’ medicine taking. The implications for communication. Fam Practitioner 2000; 17: 119–23.
26 DeJong SR, Veltman RH. The effectiveness of a CNS-led community-based COPD screening and intervention pro-gram. Clin Nurse Specialist 2004; 18: 72–79.
27 Taylor SJC, Candy B, Bryar RM, Ramsay J, Vrijhoef HJM, Esmond G, Wedzicha JA, Griffiths CJ. Effectiveness of innovations in nurse-led chronic disease management for patients with chronic obstructive pulmonary disease: sys-tematic review of evidence. Br Med J 2005; 331: 485. 28 Monninkhof EM, van der Valk P, van der Palen J, Van
Herwaarden C, Parridge M, Walters E, Zielhuis G. Self-management education for chronic obstructive pulmonary disease. Cochrane Airways Group. Cochrane Library 2005; 3: 4.
29 Venning P, Durie A, Roland M, Roberts C, Leese B. Rand-omized controlled trial comparing cost effectiveness of gen-eral practitioners and nurse practitioners in primary care. Br Med J 2000; 320: 1048–53.
30 Wiggington Cecil D, Killeen I. Control, compliance, and satisfaction in the family practice encounter. Clin Res Methods 1997; 29: 653–57.