Fracture strength of three-unit fixed partial
denture in lithium disilicate, press versus
milled, in-vitro study
NOOR KHAZAL
HOGIR ISMAIL AHMAD
Supervisor:
Christel Larsson
Odontologiska Fakulteten, Malmö
Thesis in Odontology (30 ECTS)
Malmö University
Dentistry Program
Faculty of Odontology
Frakturstyrkan hos 3-leds broar i
litiumdisilikat, press jämfört med fräs, in-
vitro studie
NOOR KHAZAL
HOGIR ISMAIL AHMAD
Handledare:
Christel Larsson
Odontologiska Fakulteten, Malmö
Examensarbete (30 hp)
Malmö Universitet
Tandläkarprogrammet
Odontologiska fakulteten
ABSTRACT
Aim: The aim of this study was to compare fracture load and fracture mode of three-unit fixed partial dentures, made in lithium disilicate when the FDPs are made with pressing technique versus milled with a CAD/CAM system.
Hypothesis: Pressing technique is better suited with regards to fracture load since milling of lithium disilicate blocks can result in defects and tension build up in the material, leaving the material more prone to chipping/micro-abrasions on the surface that could propagate and thus affecting the fracture load. P-value set to p ≤0.05.
Material and methods: 40 FDPs where manufactured with pressing technique versus milled with a CAD/CAM system in each group. Furthermore, each group where subdivided depending on the anatomy. The FDPs thereafter underwent an artificial ageing process consisting of thermocycling and preloading. After the artificial aging process the FDPs were subjected to load to fracture, where the statistical data was collected and analyzed. Also, the fracture mode was observed and analyzed.
Results: There was no significant difference regarding the fracture strength between the full anatomy groups. There was also no significant difference regarding the fracture strength between the core-design groups. The hypothesis was therefore rejected.
Conclusion: There is no significant difference with regards to how much load is required to fracture FDPs made through pressing technique compared to FDPs made through the use of CAD/CAM technique. There is a clear pattern regarding the fracture patterns, however a conclusion can’t be drawn considering the sample size.
SAMMANFATTNING
Syfte: Syftet med denna studie är att jämföra fraktur styrkan och frakturmönster hos tre-leds broar utförda i litiumdisilikat när broarna tillverkas genom pressteknik jämfört med frästa tre-leds broar genom CAD/CAM system.
Hypotes: Pressteknik är bättre lämpad med avseende till fraktur resistens då fräsning av litiumdisilikat block kan resultera i defekter och spänning i materialet, detta gör materialet mer benäget till chipping/mikroabrasioner på ytan som skulle kunna propagera och på så sätt påverka fraktur resistensen. P-värde sattes till p ≤0.05.
Material och metod: 40 3-leds broar tillverkades med pressteknik jämfört med fräst teknik med CAD/CAM system i grupper. Dessa delades in i undergrupper baserat på anatomin. Broarna genomgick en artificiell åldringsprocess som utgjordes av termocykling och
förbelastning. Efter den artificiella åldringsprocessen utsattes broarna för belastning fram till fraktur. Den statistiska datan samlades in och analyserades. Även fraktur mönstret
analyserades.
Resultat: Där fanns ingen signifikant skillnad gällande fraktur styrkan mellan de full anatomiska grupperna. Där fanns inte heller någon signifikant skillnad gällande fraktur styrkan mellan underkonstruktion grupperna. Hypotesen falsifieras därför.
Slutsats: Där fanns ingen signifikant skillnad gällande hur mycket belastning det krävs för att frakturera broarna som tillverkats genom pressteknik jämfört med broarna tillverkade med hjälp av CAD/CAM teknik. Där finns ett tydligt mönster gällande fraktur mönstret men en slutsats kan inte dras med tanke på antalet broar som använts.
TABLE OF CONTENTS
ABSTRACT 2
SAMMANFATTNING 3
INTRODUCTION 6
Material properties and design 6
Classification of Dental Ceramics 7
Ceramic Manufacturing Process 7
Lithium disilicate 8
In-vitro study 8
AIM 9
RESEARCH QUESTION 9
HYPOTHESIS 9
MATERIALS AND METHODS 9
Fixed dental prosthesis (FDP) 9
Tooth analogues 10
CAD/CAM manufacturing process 11
Pressing technique 11 Artificial aging 12 Thermocycling 12 Cementation 12 Storage 12 Cyclic preload 13 Load to fracture 13 Statistical analysis 14 RESULT 14 Fracture strength 14 Fracture mode 14 DISCUSSION 16 Discussion of result 17
How can this study benefit clinicians and labs? 17
CONCLUSION 19
CONFLICT OF INTEREST 19
ACKNOWLEDGMENT 19
INTRODUCTION
Modern prosthetic treatment aims to compensate for possible consequences of missing teeth. Dental function comprises in a wider perspective aspects of inherent aesthetic qualities and promotion of social well-being, in addition to its role as a promoter of chewing efficiency, facilitator of speech and by its inherent ability to maintain dental arch stability amongst other aspects (1).
In the case of tooth loss, most Scandinavian patients react spontaneously with a strong desire to have the tooth replaced immediately, in this case a fixed dental prosthesis (FDP) is a convenient and well-tried solution (1). Conventional prosthetic treatment has been shown to improve the quality of life, satisfaction and masticatory function. It has also been noted that the improvement was more significant if treated with fixed prosthesis which favours well for discomfort following tooth loss and will usually be compatible with maintenance of dental and oral health, if properly designed (1-3)
Via the masticatory muscle forces, the term oral biomechanics is formed, these forces put a direct force concentrated on teeth, restorations and temporomandibular joints. The form and function of the natural structures, i.e. teeth and periodontium, are therefore constructed in a way that resist these masticatory forces as long as they stay healthy and undamaged. It is thus important to design oral artificial structures in a way that resist the same forces.
Both dynamic and static strength, as well as several other mechanical properties, are required for prostheses to withstand necessary transmission of forces under different long-lasting conditions in the oral environment (1).
The force of mastication is the main source which produce stress in both teeth and prostheses, thus the magnitude of the stress varies considerably depending on the oral position. In young adults there can be maximal occlusal biting forces up to 900 N in the molar region, while the average chewing forces range between 100 N in the anterior region and up to 300 N in the posterior region. This implies that the construction should withstand more than a 1000 N occlusal force in a static fracture resistance test. It must also be taken into consideration that occlusal stress may be applied to teeth and prosthesis thousands of times per day, a prosthesis must therefore be able to withstand cyclic loading for a long period of time, nevertheless load with high magnitude (1,4).
Material properties and design
There are three main classes of materials used in prosthetic dentistry, these are divided into: metals, ceramics and polymers. With difference in physical and handling properties different materials are used in different applications (1,5)
Since the design and size radius of the gingival embrasure is crucial for the load-bearing capacity, an increase of the fracture resistance of FDPs can be achieved by broadening the curvature radius of the gingival embrasure of the interproximal connector (5,6).
During the two past decades numerous types of ceramics and processing methods have been introduced with a very promising future because of the increased demand for tooth-colored restorations. Thus, the science and technology of dental ceramics represent the fastest growing areas of dental material research and development (5).
Ceramics can be used to create tooth-like aesthetic restorations that are long lasting. The chemical stability and biocompatibility together with the optical properties are better than other available dental materials (1,5,7)
Dental ceramics are inorganic materials that are stiff and brittle, the composition consists of metallic- or half-metallic atoms and non-metallic atoms, usually oxygen atoms. By chemically bonding, sharing electrons or covalent bonds, each of these atoms gives rise to molecules which are bonded by electrostatic attraction, ionic bonds. This in turn gives rise to a strong and solid material with different grid structures. They can be either crystalline, non-crystalline (amorphous) or a mixture of both. A well-organized crystalline grid-structure is stronger and more stable than both an irregular and a more random, amorphous crystalline grid structure. Despite this, dental ceramics is favoured by both types of grid structures, in the sense that both types of structure exhibit different types of properties favoured by dental ceramics. The mixture gives rise to the characteristics of ceramic materials which include good corrosion resistance, good heat resistance, low thermal expansion coefficient, good wear resistance and optical properties. The material becomes more resistant to compression, but less resistant to tensile strength (1,6,7)
Classification of Dental Ceramics
There have been tremendous advances in the last few decades regarding the mechanical properties and methods of fabrication of ceramic materials (8). Dental ceramics are usually divided into three groups: porcelain, oxide- and glass ceramics. Oxide ceramics are stronger since they do not contain glass, however it’s the glass that gives the glass ceramics their good optical properties. Compared to leucite-based ceramics, lithium disilicate is a bit more opaque but has a stronger core. The flexural strength is more than double that of leucite-based glass ceramics (1,5)
The processing of glass-ceramics is very technique sensitive as the sintering range is very narrow. Veneered prostheses have been reported to be susceptible to chipping however the core ceramic fracture resistance is moderately high(1)
Ceramic Manufacturing Process
Dental ceramics are manufactured through a combination of different techniques. Using both additive and subtractive techniques and in some cases both, the CAM techniques that are used are mainly dependent on the stage of pressing or sintering stage the moulding is done (9). All ceramic restorations, i.e. lithium disilicate restoration can be fabricated using heat-pressing technique, which is based on the lost-wax principle. Ceramic ingots of lithium disilicate, that are prefabricated, are then heated and pressed in into a mould within a ceramic press furnace to obtain the desired shape after the wax burn-out (10,11)
Digital manufacturing procedures (CAM) can be divided into two major groups: additive- or subtractive techniques. Additive technique uses material built either from grains or molecules, whereas using the subtractive technique, material blocks are milled. These methods can be used for both metal-ceramics, ceramics and polymer materials (9).
To minimize defects and tension in the material, the blocks that are used in the subtractive technique are industrially processed under optimal circumstances. The complexity of the form/design is limited by the milling equipment used, more axis movement means more complex design. Often the additive techniques result in complex forms and designs, usually better than the subtractive techniques, but they can also produce tensions and defects in the material while processed (9).
Many types of ceramic materials can be milled by this technique; porcelain, leucite-based glass ceramics, and lithium disilicate glass ceramic. The milling procedure of ceramics are often time consuming and, in some cases, costly with regards to wear on the milling
equipment, which is related to the hardness, as well as sensitivity of the ceramics to grinding defects during the procedure. To minimize this effect there are material that are milled in a recrystallized stage, that is more easily processed. This in turn requires heat treatment to cause the material to obtain material properties including strength and hardness (9).
There are mainly two types of glass ceramics that are used in subtractive technique in
Scandinavia; Leucite-based and lithium disilicate-based glass ceramics. The simplicity in the processing method has allowed many technician labs to adapt to this technique. Usually they are processed monolithic through milling of material blocks that keeps its color throughout the procedure, which in this case limits the esthetical demands and opportunities with the material (9).
For the manufacturing of IPS.eMax one can choose between press and computer aided design and manufacturing (CAD/CAM) options, because lithium disilicate can be pressed from an ingot form or milled from a block form. With the CAD/CAM option the technician can digitally design the restoration rather than perform a full wax-up and invest/press (12). Lithium disilicate
Lithium disilicate, Li2SiO5, are glass ceramics that have a flexural strength ranging between 350 MPa and 450 MPa. In 1988 the first lithium disilicate-reinforced glass-ceramic was introduced in the dental market (IPS Empress 2 (E2), Ivoclar Vivadent, Liechtenstein) for the use as a heat-pressed core material (13). E2 was recommended for the use of a 3-unit FDPs with strength and fracture toughness values ranging from 340 to 400 MPa and 2 - 33 MPa½, respectively. (14)
In 2006 a new restorative material, lithium disilicate CAD/CAM ceramic IPS e.max CAD (Ivoclar Vivadent), was introduced in the market. These where provided as blocks
manufactured in a process based on a so-called “pressure-casting procedure” used in the glass industry. These blocks are supplied in a pre-crystallized state, so called “blue state” (14) In the blue state the ceramic contains metasilicate and lithium disilicate nuclei, and therefore can easily be milled due to its low flexural strength of 130 ± 30 MPa. After the milling process the restoration is recrystallized in a vacuum ceramic oven at a temperature of 850℃ for 20-25 min. This heat treatment dissolves the metasilicate nuclei and at the same time crystallizes the lithium disilicate which also changes the blue state to the chosen shade and translucency. After the crystallized state the ceramic contains 70% of crystals approximately 1,5 mm in size with a flexural strength of between 360 - 400 MPa. With the material
refracting light very naturally gives more indications for the use while also having strength and aesthetics (12,14).
Currently, there are few clinical studies on e.max (IPS e.max CAD, Ivoclar Vivadent) available, however short-term clinical trials on single crowns has shown a survival rate after two years to be between 97,4% and 100%.
In-vitro study
In order to evaluate the clinical potential of dental materials/restoration in-vitro studies are often used in order to prevent material/restoration failure. In-vitro study enables researchers to perform single-variable experiments under conditions that are controlled (15,16).
In order to stimulate the oral environment and conditions with regard to the mechanical properties extracted natural teeth can be used as abutment. This is however difficult, since a great number of teeth is essential to achieve statistical value. Furthermore, the variation of the
conditions and shape of the teeth has to be taken into consideration. Since the total specimens suited would be limited in total, the conclusions drawn would not be significant. Therefore, many in-vitro studies use artificial teeth as substitutes for natural teeth. Different types of materials can be used as abutment i.e. metal alloys or resin abutment. Resin abutment are often used since they are inexpensive and have properties similar to those of natural teeth (15,16). Previous studies have shown that the abutment material has an influence on the fracture load. Three-unit Zirconia FDPs cemented on metal alloys abutment has shown higher fracture load result then FDPs cemented on polymeric abutments (16-18).
According to the manufacturer lithium disilicate(IPS E.max) has an average biaxial strength of over 500 MPa, regardless of being processed via press or milling. It is further mentioned to have a flexural strength of minimum 360 Mpa (19). It is therefore of interest to study if there is any difference between lithium disilicate, being made with pressing technique versus milled. Furthermore, it is also of interest to evaluate if a clinical optimal design of 3-unit FDPs can withstand the oral environment.
AIM
The aim of this study was to compare fracture load and fracture mode of three-unit fixed partial dentures, made in lithium disilicate when the FDPs are made with pressing technique versus milled with a CAD/CAM system.
RESEARCH QUESTION
Is there any difference regarding the fracture load and fracture pattern of lithium disilicate if it’s milled or pressed?
HYPOTHESIS
It is hypothesised that pressing technique is better suited with regards to fracture load since milling of lithium disilicate blocks can result in defects and tension build up in the material, leaving the material more prone to chipping/micro-abrasions on the surface that could propagate and thus affecting the fracture load. P-value set to p ≤0.05.
MATERIALS AND METHODS
Fixed dental prosthesis (FDP)
We were provided with CAD data for tooth analogues and matching FDPs in two different designs, full anatomy respectively core-design. These designs have been used in previous studies and the method detailing how they were created are detailed in the article (“Influence of core design, production technique, and material selection on fracture behavior of yttria-stabilized tetragonal zirconia polycrystal fixed dental prostheses produced using different multilayer techniques: split-file, over-pressing, and manually built-up veneers”).
A master cast of the upper jaw with teeth 21 and 23 serving as supporting teeth with 22 missing. 21 and 23 had a 15° convergence angle and a cervical preparation design with a 120°
chamfer, the preparation was performed by the same operator. This model was then scanned with a mechanical scanner, the Procera® Forte (Nobel Biocare), the design of the bridges was formed with CAD-software (Procera PCMS, version 1.5, build 75 software).
In total 40 bridges were manufactured. The 40 bridges were split into 2 groups (see fig.1), group A and group B. Group A consist of 20 bridges that were milled using CAD/CAM technique, group B were manufactured with the help of a dental technician using pressing technique. The 2 groups were further divided into each 2 sub-groups of 10 bridges each, based on the FDPs design. Groups A.1 and B.1 designed in full anatomy, groups A.2 and B.2 were designed as core (see fig. 2).
Fig 1. Showing how the groups are divided
Fig 2. Upper model shows the Mono design (full anatomy), lower model show the State
design(core design). These models were created using CAD data provided from a previous study (17).
Tooth analogues
The tooth supporting analogues were produced using additive manufactured technique, via 3D (Formlabs 2, Formlabs, MA, USA)) printing from a polymer material (Formlabs Black Resin GPBK02, Somerville, MA, USA). The supporting analogues were made from the CAD file used to manufacture the FDPs frameworks.
CAD/CAM manufacturing process
Using CAD software, the FDPs were designed to be optimal with regards to ideal
measurements, gingival embrasure, connector design, material thickness. From the software the CAD data was sent to a milling machine. The machine was loaded with two lithium disilicate blocks (Ivoclar Vivadent - IPS e.max CAD LT, A2) were milled according to recommended settings by the software. After the milling process, the FDPs remained
connected to the blocks, this required further milling (by a dental technician) to separate and finish the glaze treatment of the FDPs.
Pressing technique
With the help of CAD/CAM 20 FDPs where milled from wax discs to resemble the wax-up stage, fig 3. 10 FDPs wax-up were designed in full anatomy, and 10 were designed as core build up.
Fig 3. Milled wax material of full anatomy design.
The waxed-up FDPs was separated from the wax disk and luted onto an investment ring base with strings of wax connected onto the FDPs. The position of the wax-up was controlled using a sprue guard. Each of the FDPs wax-up was connected to one investment ring base. The investment material used (IPS® PressVest Premium - Ivoclar Vivadent) where mixed with a vacuum mixing device according to manufacturer's description.
A silicone ring was positioned onto the investment ring base. The investment material was applied carefully with the help of a brush onto the occlusal surface of the waxed up FDPs to prevent air bubbles from being trapped. The investment ring was then filled with investment material up to the marking at the silicone ring. The investment material was then pressed with a silicone ring cap allowing excess material to be escape through the opening of the cap. The investment ring was then left to solidify and was thereafter separated from the investment ring.
Investment went through a pre-heat treatment in a heat furnace before being placed in a press furnace (Ivoclar vivadent Programat® EP 5000 G2, Software: Press HT 100g) . Before the investment was places in the press furnace 3 cold ingot (Ivoclar Vivadent - IPS e.max press LT, A2) where placed in each investment ring followed by a plunger (Ivoclar vivadent - IPS. e.max Alox plunger).
After the press furniture the investment was set in room temperature, allowed to cool down. The investment was separated with a separating disk and thereafter sand blasting until all investment material was eliminated.
The attachment points were separated, reworked and polished. The FDPs where then cleaned from contamination, polished and glazed with an even coat (Ivoclar Vivadent - IPS Ivocolor).
Artificial aging
The FDPs where put through an artificial aging process that would simulate the environment of the oral cavity. To achieve these two techniques where used, these included:
Thermocycling and preloading and are described below
Thermocycling
For the thermocycling (Thermocycler THE-1100, SD Mechatronik GmbH) process the FDPs where placed in a container separating each group. The container submerged into a two separate water baths at a temperature of +5°C and +55°C, respectively. The FDPs where submerged during a period of 20 seconds in each bath, with 10 transformation time between the separate baths. The container alternated between these two baths for a total of 5,000 cycles.
Fig 4. FDPs in the container, separated by group, mid-transfer from one bath to the other.
Cementation
The FDPs were luted onto the tooth analogues with Multilink Automix luting cement (Ivoclar Vivadent Bluephase, Scaan, Liechtenstein.) using Multilink Primer A+B with a ratio of 1:1 and light curing lamp. The FDPs were filled with cement, and placed onto the tooth analogues which then were placed under a load of 15 N in the insertion direction. For a optimal
polymerization light curing was performed for both supporting teeth individually for a curing time of 20 seconds for each surface (buccal, mesial, distal and palatinal). The cementation process was performed according to the manufacturer’s recommendations.
Storage
To create a moist environment similar to the oral cavity the FDPs were placed in 4 plastic containers separating each group. Inside the containers wetted papers were placed using distilled water to create a moisture environment. The containers were then stored in room temperature. The FDPs were kept in these containers until put into the load-to-fracture machine.
Cyclic preload
A specially built loading machine was used to preload the FDPs during 10,000 cycles, in a wet environment, between forces of 30 N and 300 N at a rate of 1 Hz sine wave. The force was applied centrally on the incisal edge of the lateral incisor pontic, with a stainless-steel indenter, 2.5mm in diameter. To avoid sliding during cyclic preload, the specimens were mounted relative to the vertical plane at a 10° inclination. After cyclic preload the FDPs where moved directly and monitored on to the fracturing machine.
Fig 5. Custom software provided by Malmo University showing the settings and data after
one group of FDPs were done.
Fig 6. Illustrate the mounting of the specimen and the insertion of the preloading and load-to
fracture machine: a) Brass foundation, b) Supporting tooth analog c) The pontic (20).
Load to fracture
To measure the fracture pattern and necessary load precisely, a load to fracture machine Instron 4465 (Instron Co. Ltd, Norwood, MA, USA) was used. The specimens were mounted in the pre-loading machine using special containers, these were moved to the Instron 4465 and placed at a 10° inclination in a similar manner to the cyclic preload, fig 6. The load was
2.5 mm in diameter. The crosshead speed was 0.255 mm/min. The machine registered data for: load required for fracture (measured in Newton), flexure distance (measured in mm) to be analysed and compared in the results section.
Statistical analysis
To analyse the data we used means of the Student’s t-test to determine the differences in fracture strength between the groups at level of significance set to P ≤ 0,05.
RESULT
Fracture strength
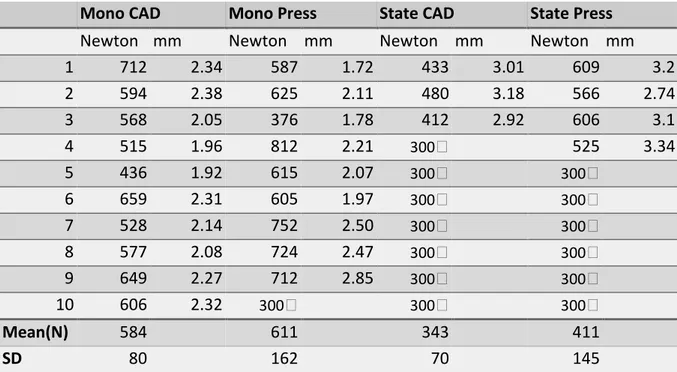
There was no significant difference regarding the fracture strength between the full anatomy groups (p > 0,05), State CAD and State Press. Therefore, the hypothesis that there would be a significance could be rejected.
There was no significant difference regarding the fracture strength between the
unreconstructed groups (p > 0,05), Mono CAD and Mono Press. The hypothesis could be rejected here too.
Table 1. Data from the load to fracture process.
Mono CAD Mono Press State CAD State Press
Newton mm Newton mm Newton mm Newton mm
1 712 2.34 587 1.72 433 3.01 609 3.2 2 594 2.38 625 2.11 480 3.18 566 2.74 3 568 2.05 376 1.78 412 2.92 606 3.1 4 515 1.96 812 2.21 300🔼 525 3.34 5 436 1.92 615 2.07 300🔼 300🔼 6 659 2.31 605 1.97 300🔼 300🔼 7 528 2.14 752 2.50 300🔼 300🔼 8 577 2.08 724 2.47 300🔼 300🔼 9 649 2.27 712 2.85 300🔼 300🔼 10 606 2.32 300🔼 300🔼 300🔼 Mean(N) 584 611 343 411 SD 80 162 70 145
🔼FDPs that fractured during cyclic mechanical preload 30-300 N, SD; standard deviation.
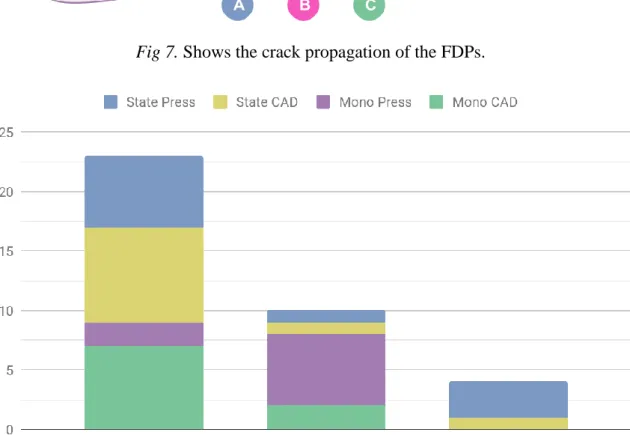
Fracture mode
Observation of the fracture mode of the 40 FDPs studied showed a visible fracture in the area of the connector and pontic. In 11 out of the 14 FDPs that fractured during the cyclic
preloading fracture occurred and the pattern was registered. The abutments fractured in 2 FDPs during cyclic preload and 1 FDPs had no visible fracture.
A. In 23 FDPs the fracture began in the distal connector between the pontic and connector and extended through the pontic.
B. In 4 FDPs the fracture began in the distal and mesial connector between the pontic and connector and extended through the pontic.
C. In 10 FDPs the fracture began in the mesial connector between the pontic and connector and extended through the pontic.
Fig 7. Shows the crack propagation of the FDPs.
DISCUSSION
The aim of this study was to investigate and compare the fracture strength and fracture behavior of 3-unit FDPs made in lithium disilicate when the FPD where made with press technique versus milled with CAD/CAM manufacturing system. The fracture mode was also analysed and registered after the FDPs had been fractured by observing if any fracture was visible in the FDPs.
In this present study a total amount of 40 specimens were examined. The 40 specimens were subdivided into four subgroups depending on the anatomy of the FDPs and manufacturing process, conventional wax-up technique vs CAD/CAM manufacturing system. Therefore, the sample size consisted of 10 specimens in each subgroup. Previous studies have shown this amount of specimens to be sufficient to show if there is an significant difference, hence the sample size (18,20).
It is important to understand the mastication function and bite forces for the evaluation of the clinical effects on dental restorations. There is a variation in the biting force in different region of the oral cavity. The greatest biting forces can be achieved the more posteriorly a transducer i placed since greater forces can be more tolerated due the periodontal ligaments around molars and also a larger area on the occlusal surfaces of the teeth (21). There are also several factors which influence the measurements of the biting forces. Factors that may influence the biting force may be related to anatomical and physiologic factors, such as craniofacial morphology, age, gender, periodontal support of teeth, temporomandibular disorders and pain, and dental status (22,23).
Since an in vitro study cannot replicate the oral environment, forces of mastication and the clinical situation, the purpose of an in vitro study is to investigate the material under similar controlled conditions. It is therefore of importance when determining the setup of an in vitro study.
The setup used in this study resembles the one used in previous studies used to determine fracture strength and fracture mode (24,25). The method used in this study was similar to the ones used in previous studies by Mahmood et al (17,26). The different FDPs designs were full anatomy and as core build up, also used in previous studies by Mahmood et al (17,26).
The artificial ageing process used to mimic the oral environment consisted of thermocycling and cycling preload. These methods were used to expose the material to fatigue and to stimulate ageing of the specimens.
The specimen where exposed to fatigue through a thermocycling process, which would stimulate the ageing process of the specimens. The process involved an abrupt change in the temperature when the FDPs where submerged in two different baths causing temperature changes, which results in stresses build up between the surface and the bulk material in the specimens (27).
To obtain a reasonable thermal cycles the value in this study was set to 10,000 cycles, which is believed to correspond a year of clinical function. The amount of cycles in previous studies has varied considerably with a mean value between 10,000 cycles (31). To obtain maximum bonding strength the Multilink Automix adhesive luting cement (Ivoclar Vivadent Bluephase, Scaan, Liechtenstein.), a universal self-curing luting composite, was used according to the manufacturer's recommendation. Also the cementation process was performed according to the manufacturer’s recommendations. Previous study has demonstrated that the use of
adhesive luting cement significantly increased the tensile bond strength in comparison of luting cement without adhesive or self-adhesive luting cement (32).
During cyclic preload the specimens were submerged in water to mimic an aqueous
environment as in the oral cavity, which in turn would resemble aging of the specimen during function in the mouth. Since the force of mastication while chewing range from 100 to 300 N, the cyclic preload had a force applied varying between 30 to 300 N. Most studies suggest that the mean value in the posterior region vary around 300 N, independent of age group, and around 100 N in anterior region (21,23,28,29). Therefor, the most optimal choice for this study would be to preset the cyclic preload machine for up to a maximum of 100 N, since the manufacturer only recommend a maximum of 3-unit FDPs to be placed in the anterior region. But since the manufacturer claims that flexural strength is over 500 MPa and due to lack of previous studies, the decision was made to place a maximum of 300 N to be able to compare with previous studies (30). The amount of load and frequencies of the cycles was chosen according to previous studies, thus allowing comparisons (17,20,25,26). To be able to compare the study with previous studies, using similar method was important and for that reason a 10° inclination was chosen. This process result in periods of tension and compression build-up which occur at the crack tip as result of load cycles (20).The damage is increased in the presence water, since stress corrosion enhance crack growth (27,31).
Discussion of result
The hypothesis was that pressing technique is better suited than milling in terms of fracture resistance however the statistical analysis showed no significant results. This is beneficial for dental practitioners, labs and dentists. In terms of labs, they can choose what is better suited for them in terms of equipment, production time and economical aspects.
Since the manufacturer can digitally design the restoration, rather than performing a full wax-up and invest/press the CAD/CAM options, could be more time beneficial, since the milling machine can work during night time.
How can this study benefit clinicians and labs?
Intra-oral scanners are becoming more widely available. Intra-oral scanning is useful from several aspects; impressions are sent to labs without the need of postal service thus reducing the cost of transportation and insuring the impressions are not damaged or shrunken. If a dental lab uses CAD/CAM they can shape and mill the FDPs faster, in turn reducing the time between patients visits to the dentist. There are also downsides to consider such as cost of acquiring and maintaining CAD/CAM hardware/software, material spill/waste using milling blocks, how many axes the mill utilizes.
Fractures during preload and connector design
13 of the 14 specimen that fractured during mechanical preloading were in the core-design group. The exact load at which the FDPs fractured during preload is unclear. Since the preloading machine is applying a force between 30 N and 300 N at a rate of 1 Hz during 10,000 cycles, it could not be registered at which period of cycle or exact load the fracture occurred. If the fractures had occurred at a very early stage during the cyclic preload it would have implied that the FDPs could not withstand loads of 300 N and possibly would have affected the statistical analysis and produced a significant difference. However it was concluded (supposed) that the FDPs could withstand forces between 30-300 N at minimum
for 1900 cycles and the load to fracture value was therefore set at 300 N. Previous studies has also encountered this problem and, drawn the same conclusions(18,20,24).
There is however a possible explanation to why it is to be expected that the core-design group would fracture during the cyclic preload. Since the dimension of both of the designs used in this study is initially used in previous studies for 3-unit FDPs in Yttria Tetragonal Zirconia Polycrystals (Y-TZP) it would mean that the dimensions for lithium disilicate in the same design is not to be recommended because of a lower flexural strength then Y-TZP.
Conventional Y-TZP is a material with a flexural strength ranging 900 to 1,200 MPa (1,5). The high flexural strength allows for the material to withstand physiological forces applied in posterior regions in the oral environment (31). This allows the dimensions for the connector to be smaller then for other all-ceramic core materials, e.g. lithium disilicate. It has been shown that a connector dimension for Y-TZP can vary from 2-4 mm in occluso-gingival height and 2-4 mm in bucco-lingual width (18). By increasing the connector dimension to 3 x 3mm, like the one used in the core-design in this study, it has been shown to increase the fracture strength of Y-TZP by 20% (20).
The importance of the design of the connector dimension therefore plays a crucial factor regarding the fracture strength and has shown in previous studies to be of great importance. By broadening the gingival and occlusal curvature radius of the connector, the fracture
resistance can be increased. The connector dimensions that was used in the core-design group were 3x3mm and the full anatomy group had two different dimension, 6.4mm x 3.5mm in the left central incisor and 7.8mm x 3.8mm in the left canine.
Fig 9. Illustrating the connector dimensions in full anatomy design(left) and
core-design(right).
According to the manufacturers recommendation regarding the connector dimension, the cross-sectional area for lithium disilicate FDPs should not decrease below 16mm2, which is the the minimum thickness recommended (30). This in the clinical situation would result in a more clumsy construction that would appear less esthetic or comfortable for the patient. The full anatomy design in this study therefore provide an estimation of the design that would most likely be used in the clinical situation. Hence, the design was chosen since it is more suited in clinical situations and there are previous studies using the same design, therefore allowing comparison with previous studies.
CONCLUSION
Within the limitations of this study, the following conclusions was drawn:
- There is no significant difference with regards to how much load is required to fracture FDPs made from lithium disilicate through pressing technique compared to FDPs made by using CAD/CAM technique.
- There is a clear pattern regarding the fracture patterns, however a conclusion can’t be drawn considering the sample size.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
ACKNOWLEDGMENT
We would like to thank our supervisors Christel Larsson and Deyar Mahmood for making this master's thesis possible. We would also like to thank dental technician Amila Vegar for
helping with the manufacturing of the FDPs. We are also thankful to Teknodont and
department of prosthetic dentistry for allowing us to use their space and machines. Thank you to Ivoclar Vivadent for materials.
REFERENCES
(1) Nilner K, edt, Karlsson S, edt, Dahl BLe. A textbook of fixed prosthodontics : the Scandinavian approach. 2nd ed.: Stockholm : Gothia fortbildning, 2013 (Slovenien); 2013. (2) Jenei Á, Sándor J, Hegedűs C, Bágyi K, Nagy L, Kiss C, et al. Oral health-related quality of life after prosthetic rehabilitation: a longitudinal study with the OHIP questionnaire. Health Qual Life Outcomes 2015 Jul 10,;13:99.
(3) Davis DM, Fiske J, Scott B, Radford DR. Prosthetics: The emotional effects of tooth loss: a preliminary quantitative study. British Dental Journal 2000 -05;188:503-506.
(4) Takaki P, Vieira M, Bommarito S. Maximum Bite Force Analysis in Different Age Groups. Int. Arch. Otorhinolaryngol 2014 Jul;18:272-276.
(5) Phillips RW, Anusavice KJ, Shen C, Rawls HR. Phillips' science of dental materials. 12th ed.: St. Louis, Mo. : Elsevier/Saunders, c2013.; 2013.
(6) Lawn BR, Pajares A, Zhang Y, Deng Y, Polack MA, Lloyd IK, et al. Materials design in the performance of all-ceramic crowns. Biomaterials 2004;25:2885-2892.
(7) Øilo M, Schriwer C. Dentala keramer.
(8) Shenoy A, Shenoy N. Dental ceramics: An update. Journal of Conservative Dentistry 2010 October;13:195.
(9) Vult Von Steyern P, Ekstrand K, Svanborg P, Örtorp A. Modern digital technologies for producing prosthetic constructions: an overview / Framställning av protetiska konstruktioner - med hjälp av moderna digitala teknologier - en översikt. Tandläkartidningen 2014:56.
(10) Subasi G, Ozturk N, Inan O, Bozogullari N. Evaluation of marginal fit of two all-ceramic copings with two finish lines. Eur J Dent 2012 Apr;6:163-168.
(11) Azar B, Eckert S, Kunkela J, Ingr T, Mounajjed R. The marginal fit of lithium disilicate crowns: Press vs. CAD/CAM. Brazilian oral research 2018;32:e001.
(12) Culp L, McLaren EA. Lithium disilicate: the restorative material of multiple options. Compendium of continuing education in dentistry (Jamesburg, N.J. : 1995) 2010;31:725. (13) Guazzato M, Albakry M, Ringer SP, Swain MV. Strength, fracture toughness and microstructure of a selection of all-ceramic materials. Part I. Pressable and alumina glass-infiltrated ceramics. Dent Mater 2004 Jun;20:441-448.
(14) Li RWK, Chow TW, Matinlinna JP. Ceramic dental biomaterials and CAD/CAM technology: state of the art. J Prosthodont Res 2014 Oct;58:208-216.
(15) Wimmer T, Erdelt K, Eichberger M, Roos M, Edelhoff D, Stawarczyk B. Influence of abutment model materials on the fracture loads of three-unit fixed dental prostheses. Dent Mater J 2014;33:717-724.
(16) Faggion CM. Guidelines for reporting pre-clinical in vitro studies on dental materials. J Evid Based Dent Pract 2012 Dec;12:182-189.
(17) Mahmood DJH, Linderoth EH, Wennerberg A, Vult Von Steyern P. Influence of core design, production technique, and material selection on fracture behavior of yttria-stabilized tetragonal zirconia polycrystal fixed dental prostheses produced using different multilayer techniques: split-file, over-pressing, and manually built-up veneers. Clin Cosmet Investig Dent 2016;8:15-27.
(18) Larsson C, Holm L, Lövgren N, Kokubo Y, Vult von Steyern P. Fracture strength of four-unit Y-TZP FPD cores designed with varying connector diameter. An in-vitro study. J Oral Rehabil 2007 Sep;34:702-709.
(19) https://www.makeitemax.com/better-emax (2019-04-30).
(20) Bahat Z, Mahmood DJH, Vult von Steyern P. Fracture strength of three-unit fixed partial denture cores (Y-TZP) with different connector dimension and design. Swed Dent J
2009;33:149-159.
Groups. International Archives of Otorhinolaryngology 2014 Jul;18:272-276.
(22) van der Bilt A, Tekamp A, van der Glas H, Abbink J. Bite force and electromyograpy during maximum unilateral and bilateral clenching. Eur J Oral Sci 2008 Jun;116:217-222. (23) Koc D, Dogan A, Bek B. Bite force and influential factors on bite force measurements: a literature review. European journal of dentistry 2010 Apr;4:223-232.
(24) Mahmood DJH, Linderoth EH, Von Steyern PV, Wennerberg A. Fracture strength of all-ceramic (Y-TZP) three- and four-unit fixed dental prostheses with different connector design and production history. Swed Dent J 2013;37:179-187.
(25) Mahmood DJH, Linderoth EH, Von Steyern PV, Wennerberg A. Fracture strength of all-ceramic (Y-TZP) three- and four-unit fixed dental prostheses with different connector design and production history. Swed Dent J 2013;37:179-187.
(26) Mahmood DJH, Linderoth EH, Vult Von Steyern P. The influence of support properties and complexity on fracture strength and fracture mode of all-ceramic fixed dental prostheses. Acta Odontologica Scandinavica 2011 Jul;69:229-237.
(27) Morresi AL, D'Amario M, Capogreco M, Gatto R, Marzo G, D'Arcangelo C, et al. Thermal cycling for restorative materials: does a standardized protocol exist in laboratory testing? A literature review. J Mech Behav Biomed Mater 2014 Jan;29:295-308.
(28) Bonakdarchian M, Askari N, Askari M. Effect of face form on maximal molar bite force with natural dentition. Arch Oral Biol 2009 Mar;54:201-204.
(29) Lassila V, Holmlund I, Koivumaa KK. Bite force and its correlations in different denture types. Acta Odontol Scand 1985 Jul;43:127-132.
(30) http://www.ivoclarvivadent.com/zoolu-website/media/download/27583/IPS+e-max+Press+Monolithic+Solutions?v=1 (2019-04-30).
(31) Daou EE. The Zirconia Ceramic: Strengths and Weaknesses. The open dentistry journal 2014;8:33-42.