1 Örebro University
School of Medical Sciences Degree project, 15 ECTS January 2020
Are Individuals with Attention-Deficit /Hyperactivity
Disorder at Increased Risk for Type 2 Diabetes Mellitus?
- A systematic literature review
Author: Nour Alden Jojeh Supervisors: Lin Li (Doctoral student)
Henrik Larsson (professor) Örebro, Sweden
2
Abstract
Background: Attention-deficit/hyperactivity disorder (ADHD) is a neuropsychiatric disease that
affects school-aged children and adults. The overall worldwide prevalence of ADHD is estimated to be about 2- 7% in children and 2- 5% in adults. Little is known about its
associations to various metabolic disorders such as type 2 diabetes mellitus (T2DM). Emerging research suggests a positive association between T2DM and ADHD, but the results are
inconclusive. Moreover, the underlying mechanisms behind this possible association are still largely unknown.
Aim: To explore whether there is a link between ADHD and T2DM and the potential
mechanisms.
Methods: We searched PubMed and Cochrane Library up to 20 November 2020 without any
restrictions on language or date of publication. We included all case-control studies, cohort studies, epidemiologic studies, observational studies, longitudinal studies, and follow-up studies on ADHD subjects of any age, sex or setting who were diagnosed with T2DM during the study or prior to the study. The author then used the Newcastle-Ottawa Scale to assess the quality of the chosen studies.
Results: We identified 28 articles and three of them were considered relevant and were therefore
included. The included studies reported a positive association of ADHD and T2DM, the prevalence of T2DM in ADHD diagnosed subjects ranged from 0.8% to 3.9% and remained higher when compared to the prevalence of T2DM in the non-ADHD group (control group) with a prevalence ranging from 0.2 to 1.62%. Multiple mechanisms were discussed in the included studies, including proinflammatory cytokine oversecretion combined with an immunologic dysregulation and reduced blood flow to the parietal and frontal lobes in T2DM patients.
Conclusion: Due to the limited number of relevant studies, there is no clear evidence for a
causal link between ADHD and T2DM. More researches are needed to elucidate the exact underlying genetic and biochemical mechanisms behind this possible association.
3
Abbreviations:
ADHD: Attention-deficit/hyperactivity disorder T2DM: Type 2 Diabetes Mellitus
T1DM: Type 1 Diabetes Mellitus IL: Interleukin
TNF: Tumor necrosis factor IFN: Interferon
NOS: Newcastle Ottawa Scale
PRISMA: Preferred Reporting Items for Systematic Reviews PICO: Population, Intervention, Control, Outcome
DRD4: Dopamine Receptor D4
4
Content
Abstract ... 2 Content ... 4 1. Introduction ... 5 2. Aim ... 63. Material and Methods ... 6
Search strategy ... 6
Data extraction ... 7
Ethical Consideration ... 7
Risk of bias (quality) assessment ... 7
4. Results ... 7
5. Discussion ... 12
Overall summary ... 12
Potential mechanisms ... 12
Biological pathways mentioned in the previous studies ... 12
Potential causal link mediated by obesity ... 12
Causal link mediated by smoking... 13
Association biased by confounders ... 14
6. Strengths and Limitations ... 15
7. Clinical Implication ... 15
8. Conclusion ... 15
5
1. Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a neuropsychiatric disorder characterized by persistent inattention and/or hyperactivity-impulsivity that are inappropriate for one’s
developmental stage [1]. The DSM-V (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition) describes three types of ADHD, predominantly inattentive, predominantly
hyperactive-impulsive and combined type [2]. ADHD is considered to be one of the most
common neurodevelopmental disorders in children [3]. Males are approximately four times more likely to be affected by ADHD compared to females [4]. The worldwide prevalence of ADHD was estimated to be around 2- 7% in children [5]. ADHD persists into adulthood in a high proportion of cases; the worldwide prevalence of ADHD in adults was estimated to be about 2- 5% [6]. The etiology of ADHD is multifactorial and is a combination of both genetic and environmental factors such as: viral infections, fetal exposure to alcohol, maternal smoking during pregnancy and various thyroid disorders [7]. The pathophysiology of ADHD is not fully-understood, dysfunctionalities in the cortico-subcortical pathways combined with abnormalities in the dopaminergic and noradrenergic systems have been implicated through neuroimaging studies [8]. ADHD patients suffer from adverse psychiatric and somatic comorbidities. The prevalence of psychiatric comorbidities have been estimated to be about 62.5% among children [9] and 53.5% among adults [10] including oppositional defiant disorder, conduct disorder and anxiety which complicate the otherwise straightforward treatment of ADHD and pose
considerable clinical and public health challenges [11]. However, limited evidence has been found on the association between ADHD and somatic diseases among both children and adults, such as the metabolic syndrome [12] [13].
Type 2 diabetes mellitus (T2DM) on the other hand is a common metabolic disorder that stems from a defective insulin resistance, insulin secretion or both resulting in a dysregulated
carbohydrates, protein and lipid metabolism [14]. T2DM is a major public health burden
affecting 462 million individuals (approximately 6.28% of the whole population), 4.4% of those are in the 15- 49 age group, moreover, over 1 million deaths per year can be linked to diabetes, making it one of the major causes of mortality [15]. Early-onset DM has also been associated with poorer academic achievement, motor speed and eye-hand coordination [16]. Current evidence on the co-occurrence of ADHD and T2DM is inconclusive [17] and knowledge of the possible pathophysiological mechanisms that underline these two common diseases is limited. Furthermore, managing diabetes can be adversely affected by ADHD symptoms because they
6 require constant vigilance; therefore, understanding the concurrence of these traits is necessary to ensure that patients receive prompt and appropriate treatment.
2. Aim
The aim of this systematic literature review is to explore whether there is a link between ADHD and T2DM and the potential mechanisms.
3. Material and Methods
Search strategy
PubMed and Cochrane Library were searched up to the 20th of November 2020. The following search terms with filters ‘human’ and ‘English’ for both databases were used: 1) Mesh terms: Diabetes Mellitus, Type 2, Glucose Intolerance, Insulin Resistance, Hyperglycemia,
Hypoglycemia and Attention Deficit Disorder with Hyperactivity. 2) Other terms: impaired glucose tolerance, IGT, diabetes mellitus, diabetes, glucose, insulin, Type 2 Diabetes Mellitus, type 2 diabetes, T2DM, attention deficit hyperactivity disorder, ADHD, hyperkinetic disorder, hyperactiv* and inattenti*. References of the selected papers were hand searched to retrieve any possible additional pertinent publication that could have been missed with the electronic search.
Selection criteria
Published studies were included according to the following inclusion criteria: 1) Case-Control studies, cohort studies (prospective, retrospective and population based studies), epidemiologic studies, observational studies, longitudinal studies, and follow-up studies. 2) Participants from clinical or general population. 3) Studies including ADHD and T2DM diagnosed participants. 4) Studies assessing the prevalence of T2DM in ADHD patients. Exclusions were made according to the following exclusion criteria: 1) Animal studies. 2) Non-empirical studies. 3) Studies based on DSM-I and DSM-II which were not based on empirical data. 4) Studies without a definition of ADHD or studies examining the association between other psychiatric disorders and
T2DM/T1DM. 5) Studies lacking statistical data analyses. A more detailed description of the search process, inclusion/exclusion criteria, PICO, data extraction and quality assessment is available as supplementary data; see the second attached file.
7 Data extraction
The following data were extracted from each study retained for the qualitative synthesis: name of the first author, publication year, study location, study design, data sources, number of
participants, mean age of the participants, covariates and how they were handled, adjusted effect size (Odds ratio (OR), Risk ratio (RR), Hazard ratio (HR), Prevalence ratio (PR)) with 95% confidence interval (CI) and conclusion.
Ethical Consideration
This study is a systematic literature review of previously published material; therefore, ethical problems with the implementation of this study are not applicable. However, it has not been taken into consideration if the chosen articles have been reviewed by an ethics review board or not. In this systematic literature review all the results that emerged after the search process have been presented, both those that support and do not support the author’s aim. No data was deliberately excluded or distorted and objectivity was maintained throughout the whole process for instance including all relevant articles despite their results.
Risk of bias (quality) assessment
The author used the Newcastle-Ottawa Scale (NOS) to assess the quality of the found papers. Nine stars is the maximum that can be given for case-control/cohort studies (ten stars is the maximum for cross-sectional studies) based on selection, comparability and exposure/outcome criteria. Studies that are considered low- rated will not be discarded but be examined to see their overall impact on the study.
4. Results
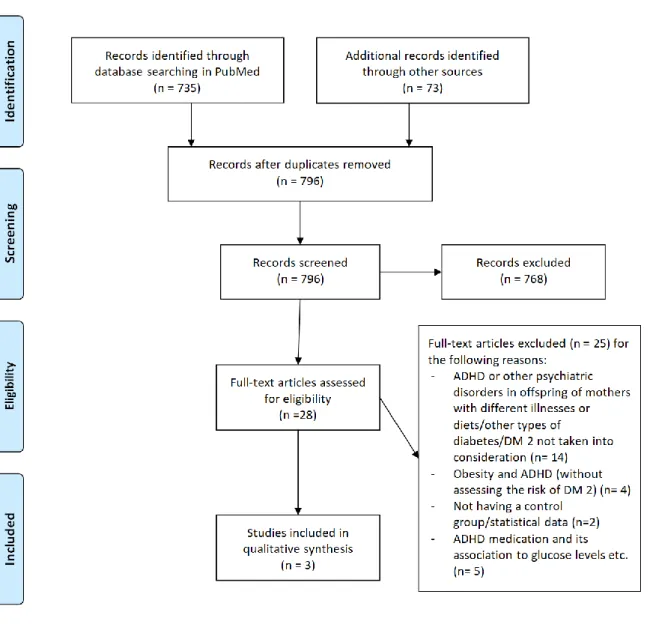
The study selection process is shown in PRISMA (Figure 1) and a list of excluded studies with reasons for exclusion is shown in the supplementary data file. 735 records in PubMed and 73 records in Cochrane Library were identified. After removing duplicate records, 796 records were screened by reviewing titles and abstracts, 768 records were then removed and 28 records were full-text assessed for eligibility of which 25 were removed for various reasons described in the supplementary data file. Ultimately, our qualitative review included three published research studies based on original data.
Table 1 shows the main characteristics of the three included studies. The three included studies
[18] [19] [20] were case-control, cohort and cross-sectional studies respectively and were conducted between 2013 and 2018. Two studies [18] [19] were based on data from the Taiwan
8 National Health Research institute and one [20] was based on a data from the Swedish national registers, thus, a relatively large participant sample was included in all of the studies, the participant sample ranged from 4,302 subjects with ADHD and 21,510 controls to 61,129 ADHD subjects and 5,490,678 controls. The mean age ranged from 8.6 to 40.55 years. The statistical methods and reported results varied across studies. Chen H et al [18] reported that ADHD was significantly correlated with a previous T2DM diagnosis (OR = 2.75, 95%
confidence interval (CI) = 1.82–4.16), Chen M et al [19] reported similar findings; adolescents and young adults with ADHD were at higher risk of developing T2DM (HR = 2.83; 95% CI, 1.96-4.09 in adolescents and HR = 3.28; 95% CI, 1.41-7.63 in young adults), further, Chen Q et al [20] reported a PR of 2.41, 95% CI: 2.27-2.55 indicating that T2DM is more prevalent in ADHD subjects. The selected studies consistently suggested a significant association between ADHD and T2DM, with the prevalence of T2DM in ADHD subjects ranging from 0.8-3.9%. Even though all studies were based on large sample size, they still suffered from some limitations including not being able to measure the severity of ADHD, the inclusion of only those who sought medical assistance and not being able to include those treated in primary care due to limitations with the data-bases.
Table 2 represents the potential confounders that have been assessed in the selected studies.
Age, sex, geographic region, diagnostic criteria for ADHD and T2DM and metabolic /
psychiatric comorbidities were evaluated in most of the studies. The quality assessment of the chosen studies is demonstrated in Table 3. Each study was judged based on selection,
comparability and outcome/exposure by using the Newcastle-Ottawa Scale. Nine stars is the maximum that can be awarded to each study (ten stars is the maximum for cross-sectional studies). The selected studies were awarded a total of nine to ten stars each indicating a high quality.
9
Table 1: Characteristics of the studies included in the qualitative synthesis
First author (year) Study design Country/data source (s) Subjects Mean age (SD)/age range (years)
Adjusted estimates (OR, RR, HR ,PR and 95% CI)
Prevalence, % Conclusion Strengths and limitations
Chen H et al. (2013) Case-control study Longitudinal Health Insurance Database (LHID2005) in Taiwan
4,302 patients with ADHD as cases and 21,510 randomly selected subjects as controls
8.6 y (SD = 2.7 y) ADHD was significantly correlated with a previous T2DM diagnosis (OR = 2.75, 95% confidence interval (CI) = 1.82–4.16)
The prevalence of T2DM in subjects with ADHD (N=4,302) is 0.8
The prevalence of T2DM in the controls (N=21,510) is 0.3
A significant correlation between ADHD and a previous T2DM diagnosis
Strength: large sample population (population based database) Limitations: The use of antipsychotic drugs have been suggested to contribute to DM which might have influenced the study
Chen M et al. (2018) Cohort study The Taiwan National Health Insurance Research Database
35,949 subjects with ADHD and 71,898 controls (age and sex matched)
10- 17 (adolescents) and 18 -29 (young adults), the mean age was 12.89 ± 3.33
Adolescent (hazard ratio = 2.83; 95% CI, 1.96-4.09) and young adults (hazard ratio = 3.28; 95% CI, 1.41-7.63) with an ADHD diagnosis had a higher risk of developing T2DM compared to the control group ADHD subjects had a shorter mean ± SD period between admission and commencement of T2DM (3.17 ± 2.33 vs. 4.08 ± 2.11 years, P = .004) during the follow up compared to the control group.
The prevalence of T2DM in adolescents and young adults with ADHD (N=35,949) is 0.83 The prevalence of T2DM in the controls (N=71,898) is 0.21
A higher risk of developing T2DM in adolescents and young adults
Strength: large sample size by using the Taiwan National Health Insurance Research Database Limitations: the study only included patients who sought medical assistance meaning that the incidence of T2DM might have been underestimated
Chen Q et al. (2018) Cross-sectional study The Swedish National Patient Register
5,551,807 subjects (18 to 64 years old) living in Sweden on December 31, 2013 of whom 61,129 had an ADHD diagnosis.
A subgroup of 1,665,938 (50 to 64 years old) adults of whom 4,864 had an ADHD diagnosis were elected to study different comorbidity patterns of adult ADHD in older adults
18 to 64 years (Mean [SD] age: 40.55 [13.49] years)
T2DM is more common in subjects with ADHD than in those without, with the approximated prevalence ratio = 2.41, 95% CI: 2.27-2.55
The prevalence of T2DM in adults with ADHD is 3.9 (95% CI = 3.68-4.13)
The prevalence of T2DM in adults without ADHD is 1.62 (95% CI = 1.61-1.63)
T2DM is more prevalent in ADHD subjects when compared to the non-ADHD group
Strength: large sample size through the linkage of multiple Swedish national Registers
Limitations: subjects who failed to seek medical assistance and those treated in primary care were not included in the national patient register.
10
Table 2: Variables/possible confounders assessed in the above selected studies
variables Chen H et al. 2013 Chen Q et al. 2018 Chen M et al. 2018 Age x x x Sex x x x Geographic region x x Presence of diabetes 1 x Index year (first
diagnosis of ADHD) x
Diagnosis criteria for ADHD (ICD/DSM)
x x x
Diagnosis criteria for T2DM (ICD-9)
x x x
Psychiatric conditions other than ADHD
x x x Metabolic conditions related to T2DM (hypertension and dyslipidemia) x x
Table 3: Quality assessment by using the Newcastle-Ottawa Scale (NOS) [21] [22]
Study Study design
Selection Comparability Outcome Exposure Total
Chen H (2013) Case-control study
****
**
***
9 Chen M (2018) Cohort study****
**
***
9 Chen Q (2018) Cross-sectional study*****
**
***
1011 * Each study was judged on eight items from Newcastle-Ottawa Scale, where stars awarded for each quality item serve as a quick visual assessment. The highest quality studies are awarded up to nine stars.
12
5. Discussion
Overall summary
Previous evidence on the associations between ADHD and T2DM is limited. Only three population-based studies with various study designs were identified and suggested that
individuals with ADHD are at increased risk for T2MD. Further, because of the limited number of studies, it is currently unclear whether the observed associations are due to a causal effect or confounding.
Potential mechanisms
Biological pathways mentioned in the previous studies
Several mechanisms underlying this association have been discussed in the selected studies; a reduced blood flow to the frontal and parietal lobes was suggested to explain the cognitive impairment in patients with T2DM, moreover, proinflammatory cytokine oversecretion combined with an immunologic dysregulation has been suggested to explain the potential association between ADHD and T2DM [23]; IL-2 (interleukin), IL-6, IFN-gamma (interferon), IL-16, IL-10 and IL-13 were marginally increased in ADHD patients when compared to a non-ADHD control group [24]. Furthermore, T2DM patients had higher levels of IL-6, TNF-alpha and C-reactive protein (CRP) compared to the control group (without T2DM) [25]. Of note, adolescents and young adults with ADHD using atypical antipsychotic drugs exhibited an
increased risk of developing T2DM but studies assessing the prevalence of atypical antipsychotic drugs use in ADHD patients were limited and further studies are needed to specifically identify the number of ADHD patients using atypical antipsychotic drugs in order to have a more accurate representation.
Potential causal link mediated by obesity
Some biological mechanisms have been proposed as mediators to support a potential causal association such as obesity. A systematic review and meta-analysis of 42 studies reported a significant correlation between ADHD and obesity in both children (OR=1.20, 95% CI=1.05– 1.37) and adults (OR=1.55, 95% CI=1.32–1.81) [26]. It has been reported that both the impulsive and inattentive segments of ADHD could increase the risk of obesity, moreover, a deficiency in the inhibitory control which characterizes a large group of ADHD patients could underlay abnormal eating behaviors which in turn might lead to overweight and obesity. Reduced planning skills and inattention could lead to struggles in complying with regular and healthy
13 eating patterns [27]; in addition, inattention may be correlated with an inability to recognize the “right” amount of food intake.
The hyperactive part of ADHD, as motor overactivity, would naturally be considered to decrease the risk of overweight and obesity by increasing energy expenditure. However, the hyperactivity component is not constant but is regulated by context meaning that for instance it decreases while watching television [28] and it has been shown that children with an ADHD diagnosis tend to watch more television and to be less involved in physical activities than those of the same age without an ADHD diagnosis [29]. Craving immediate rewards and aberrant eating habits/patterns are thought to be caused by an insufficient dopamine related natural reinforcement which in turn is the main characteristic of a “reward deficiency syndrome” which interestingly has been seen in both obesity and ADHD [30]. In addition, an association between oxidative stress and ADHD has been established, not to mention that oxidative stress plays a key role in the pathophysiology underlying obesity [31]. Furthermore, using omega-3 fatty acids which are considered
antioxidants has been shown to reduce ADHD symptoms [32]. Of note, it has been shown that most T2DM patients are obese because T2DM is highly related to unhealthy lifestyle patterns such as diets involving unhealthy options and low physical activity/energy expenditure [33] [34], further, an increase in fat accumulation in the abdominal region is correlated to an increased risk of the metabolic syndrome and T2DM [35], it has also been established that central obesity is responsible for a twofold increased risk of developing T2DM through a number of secreted factors including TNF-alpha, resistin and adipocytokines which contribute to a general low-grade inflammation and a subsequent insulin resistance [36].
Causal link mediated by smoking
Another biological mechanism for the potential causal link has been suggested to underlay the association between ADHD and T2DM is smoking. Several studies indicate that smoking is more prevalent in ADHD diagnosed adults (41- 42%) when compared to non- ADHD adults (26%) [37]. It has been reported that ADHD is a risk factor for tobacco use after controlling for comorbid conduct disorder [38] which has been discussed to be the cause behind the
co-existence of ADHD and substance use disorder in general [39], moreover, it has been suggested that executive function deficits that are related to ADHD symptoms anticipate smoking [40]. Moreover, a linear correlation was found when examining 15,000 young adults in a population based study between the number of self-reported ADHD symptoms (retrospectively) and the life time risk of smoking [41]. Several genes have been discussed to be involved in the high
co-14 occurrence of smoking in ADHD subjects, polymorphism of the DRD4 and DAT which are involved in the monoamine regulation have been linked to a greater level of smoking in various studies [42] [43], in another study [44], subjects diagnosed with ADHD with six or more
hyperactivity-impulsivity symptoms bearing the DRD2/ANKK1(dopamine receptor D4/Ankyrin repeat and kinase domain containing 1) Taq1 A2/A2 allele were up to two times as likely to have a smoking history when compared to individuals with an A1 allele [45]. Additionally, A
correlation between active smoking and a heightened risk of developing T2DM has been observed in a systematic review and meta-analysis of 25 prospective cohort studies [46], of which 24 reported adjusted risk ratio (RR) higher than 1, the author found that the risk of
developing T2DM is higher in the heavy smoker group (more or equal to 20 cigarettes/ day than those in the lighter smokers group, the author also concluded that the risk for developing T2DM is lower for former smokers when compared to active smokers.
Multiple causes behind this association were discussed, for instance several (but not all [47]) studies reported a theoretical possibility for causality in that smoking may lead to insulin resistance and/or deficient insulin secretion [48] [49]. Another plausible mechanism is that nicotine or other ingredients in cigarettes may influence the pancreatic beta cells responsible for insulin secretion [50]. Furthermore, multiple non casual explanations were suggested in order to unriddle the association between T2DM and smoking, for instance: smoking is generally
correlated to lower physical activity and unhealthy routines (consuming less fruits/vegetables, high intake of alcohol) that contribute to weight gain and/or DM [51]. Moreover, a weight cycling phenomenon has been observed in which smokers tend to gain weight when they quit smoking; the stronger the addiction the harder it is for them to quit smoking ending up with them relapsing and gaining weight in the process [52]. Lastly a higher risk of accumulating abdominal fat among smokers when compared to non-smokers has been reported [53] which in itself
increases the risk of T2DM, the exact mechanism behind the heightened risk of fat accumulation is not well understood, a possible mechanism is that smoking has an anti-estrogenic effect on the body which could lead to a hormonal imbalance [54] and a higher risk of developing central obesity which is a known risk factor for T2DM [55].
Association biased by confounders
The increased risk of T2DM in ADHD patients could also be explained by other factors such as potential confounders including geographic region, age and sex, genetics, early life factors and socioeconomic status; children living in families with low socioeconomic status were shown to be more likely to receive an ADHD diagnosis when compared to children living in families with
15 better socioeconomic status [56], further, lower income and education level was associated with a higher prevalence of T2DM [57]. Most of the included studies adjusted for the above
mentioned confounder in their statistical analysis except for socioeconomic status, genetics and early life factor. Of note, using the ICD-9 to diagnose ADHD and T2DM meant that the severity of ADHD and T2DM was not taken into account which may have affected the results. Lastly, although psychiatric comorbidities were taken into consideration in most of the studies, ADHD- symptoms might be severe in some patients that antipsychotic medications are prescribed which might have biased the results since the use of antipsychotic drugs have been suggested to
increase the risk of diabetes [58].
6. Strengths and Limitations
The strength of this systematic literature review is that it is based on studies with a relatively large sample size which contributes to a more accurate representation of the possible association between ADHD and T2DM, furthermore, this study extended the findings from a recent
systematic review [59] by presenting relevant biological factors that could explain the
mechanisms underlying the association between T2DM and ADHD. Possible limitations of this study could be the limited number of available studies on the ADHD and T2DM subject, additionally, only data from 2 countries was acquired in the selected studies which make it difficult for the results of this study to be generalized, moreover, the causal link could not be tested due to the lack of longitudinal studies.
7. Clinical Implication
An increase in the prevalence of T2DM in ADHD diagnosed subjects has been reported despite the low number of available studies. From a clinical point of view, managing diabetes can be adversely affected by ADHD symptoms because they require constant vigilance, understanding the concurrence of these traits is necessary to ensure that patients receive prompt and appropriate treatment, thus, health care providers should remain vigilant to metabolic problems especially T2DM in ADHD affected individuals even in the absence of typical T2DM risk factors.
8. Conclusion
Individuals with ADHD are at higher risk of T2DM compared to the non-ADHD population, but the potential mechanisms are still unclear given the limited evidence so far. Further researches and studies from various countries and settings with longitudinal design are needed to elucidate
16 the exact underlying genetic and biochemical mechanism underlying the potential link from ADHD to T2DM
9. References
[1] Cherkasova M, Sulla EM, Dalena KL, Pondé MP, Hechtman L. Developmental course of attention deficit hyperactivity disorder and its predictors. J Can Acad Child Adolesc Psychiatry. 2013 Feb;22(1):47-54.
[2] Ayano G, Yohannes K, Abraha M. Epidemiology of attention-deficit/hyperactivity disorder (ADHD) in children and adolescents in Africa: a systematic review and meta-analysis. Ann Gen Psychiatry. 2020;19:21.
3] Mahone EM, Denckla MB. Attention-Deficit/Hyperactivity Disorder: A Historical Neuropsychological Perspective. J Int Neuropsychol Soc. 2017 10;23(9-10):916-29.
[4] Ramtekkar UP, Reiersen AM, Todorov AA, Todd RD. Sex and age differences in attention-deficit/hyperactivity disorder symptoms and diagnoses: implications for DSM-V and ICD-11. J Am Acad Child Adolesc Psychiatry. 2010 Mar;49(3):217-28.e1-3.
[5] Sayal K, Prasad V, Daley D, Ford T, Coghill D. ADHD in children and young people: prevalence, care pathways, and service provision. Lancet Psychiatry. 2018 02;5(2):175-86.
[6] Polyzoi M, Ahnemark E, Medin E, Ginsberg Y. Estimated prevalence and incidence of diagnosed ADHD and health care utilization in adults in Sweden - a longitudinal population-based register study. Neuropsychiatr Dis Treat. 2018;14:1149-61.
[7] Chen HJ, Lee YJ, Yeh GC, Lin HC. Association of attention-deficit/hyperactivity disorder with diabetes: a population-based study. Pediatr Res. 2013 Apr;73(4 Pt 1):492-6.
[8] Biederman J. Attention-deficit/hyperactivity disorder: a selective overview. Biol Psychiatry. 2005 Jun 1;57(11):1215-20.
17 [9] Amiri S, Shafiee-Kandjani AR, Fakhari A, Abdi S, Golmirzaei J, Akbari Rafi Z, et al.
Psychiatric comorbidities in ADHD children: an Iranian study among primary school students. Arch Iran Med. 2013 Sep;16(9):513-7.
[10] Anker E, Bendiksen B, Heir T. Comorbid psychiatric disorders in a clinical sample of adults with ADHD, and associations with education, work and social characteristics: a cross-sectional study. BMJ Open. 2018 03 2;8(3):e019700.
[11] Ohnishi T, Kobayashi H, Yajima T, Koyama T, Noguchi K. Psychiatric Comorbidities in Adult Attention-deficit/Hyperactivity Disorder: Prevalence and Patterns in the Routine Clinical Setting. Innov Clin Neurosci. 2019 Sep 1;16(9-10):11-6.
[12] Instanes JT, Klungsøyr K, Halmøy A, Fasmer OB, Haavik J. Adult ADHD and Comorbid Somatic Disease: A Systematic Literature Review. J Atten Disord. 2018 02;22(3):203-28.
[13] Pliszka SR. Psychiatric comorbidities in children with attention deficit hyperactivity disorder: implications for management. Paediatr Drugs. 2003;5(11):741-50.
[14] Smushkin G, Vella A. What is type 2 diabetes. Medicine (Abingdon). 2010 Nov 1;38(11):597-601.
[15] Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of Type 2 Diabetes - Global Burden of Disease and Forecasted Trends. J Epidemiol Glob Health. 2020 03;10(1):107-11.
[16] Chen HJ, Lee YJ, Yeh GC, Lin HC. Association of attention-deficit/hyperactivity disorder with diabetes: a population-based study. Pediatr Res. 2013 Apr;73(4 Pt 1):492-6.
[17] Landau Z, Pinhas-Hamiel O. Attention Deficit/Hyperactivity, the Metabolic Syndrome, and Type 2 Diabetes. Curr Diab Rep. 2019 06 27;19(8):46.
[18] Chen HJ, Lee YJ, Yeh GC, Lin HC. Association of attention-deficit/hyperactivity disorder with diabetes: a population-based study. Pediatr Res. 2013 Apr;73(4 Pt 1):492-6.
18 [19] Chen MH, Pan TL, Hsu JW, Huang KL, Su TP, Li CT, et al. Risk of Type 2 Diabetes in Adolescents and Young Adults With Attention-Deficit/Hyperactivity Disorder: A Nationwide Longitudinal Study. J Clin Psychiatry. 2018 May/Jun;79(3):17m11607.
[20] Chen Q, Hartman CA, Haavik J, Harro J, Klungsøyr K, Hegvik TA, et al. Common psychiatric and metabolic comorbidity of adult attention-deficit/hyperactivity disorder: A population-based cross-sectional study. PLoS One. 2018;13(9):e0204516.
[21] NEWCASTLE - OTTAWA QUALITY ASSESSMENT SCALE CASE CONTROL STUDIES [Internet]. Available from:
http://www.ohri.ca/programs/clinical_epidemiology/nosgen.pdf [cited 15 November 2020].
[22] S1 Text NEWCASTLE - OTTAWA QUALITY ASSESSMENT SCALE (adapted for cross sectional studies) [Internet]. Available from:
https://journals.plos.org/plosone/article/file?type=supplementary&id=info:doi/10.1371/journal.p one.0147601.s001 [cited 15 November 2020].
[23] Oades RD, Dauvermann MR, Schimmelmann BG, et al. Attention-deficit hyperactivity disorder (ADHD) and glial integrity: S100B, cytokines and kynurenine metabolism effects of medication. Behav Brain Funct. 2010;6(1):29.
[24] Anand D, Colpo GD, Zeni G, Zeni CP, Teixeira AL. Attention-Deficit/Hyperactivity Disorder And Inflammation: What Does Current Knowledge Tell Us? A Systematic Review. Front Psychiatry. 2017;8:228.
[25] Rajkovic N, Zamaklar M, Lalic K, et al. Relationship between obesity, adipocytokines and inflammatory markers in type 2 diabetes: relevance for cardiovascular risk prevention. Int J Environ Res Public Health. 2014;11(12):4049-4065.
[26] Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Peñalver C, Rohde LA, Faraone SV. Association Between ADHD and Obesity: A Systematic Review and Meta-Analysis. Am J Psychiatry. 2016 Jan;173(1):34-43.
19 [27] Cortese S, Castellanos FX: The relationship between ADHD and obesity: implications for therapy. Expert Rev Neurother 2014; 14: 473–479.
[28] Porrino LJ, Rapoport JL, Behar D, et al: A naturalistic assessment of the motor activity of hyperactive boys: I. Comparison with normal controls. Arch Gen Psychiatry 1983; 40:681–687.
[29] Kim J, Mutyala B, Agiovlasitis S, et al: Health behaviors and obesity among US children with attention deficit hyperactivity disorder by gender and medication use. Prev Med 2011; 52:218–222.
[30] Cortese S, Vincenzi B: Obesity and ADHD: clinical and neurobiological implications. Curr Top Behav Neurosci 2012; 9:199–218.
[31] Joseph N, Zhang-James Y, Perl A, et al: Oxidative stress and ADHD: a meta-analysis. J Atten Disord 2013 (Epub ahead of print, Nov 14, 2013).
[32] Bloch MH, Qawasmi A: Omega-3 fatty acid supplementation for the treatment of children with attention-deficit/hyperactivity disorder symptomatology: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry 2011; 50:991–1000.
[33] Sami W, Ansari T, Butt NS, Hamid MRA. Effect of diet on type 2 diabetes mellitus: A review. Int J Health Sci (Qassim). 2017 Apr-Jun;11(2):65-71.
[34] Diabetes and Obesity [Internet]. 2019. Available from:
https://www.diabetes.co.uk/diabetes-and-obesity.html#:~:text=Links%20between%20obesity%20and%20type%202%20diabetes&text=In %20fact%2C%20obesity%20is%20believed,BMI%20of%20less%20than%2022. [cited 11 November 2020].
[35] Björntorp P. Metabolic implications of body fat distribution. Diabetes Care 1991;14:1132– 1143.
20 [36] Freemantle N, Holmes J, Hockey A, Kumar S. How strong is the association between
abdominal obesity and the incidence of type 2 diabetes. Int J Clin Pract. 2008 Sep;62(9):1391-6.
[37] Pomerleau, O.F. et al. 1995. Cigarette smoking in adult patients diagnosed with attention deficit hyperactivity disorder. J. Subst. Abuse 7: 373– 378.
[38] Molina, B.S. & W.E. Pelham, Jr. 2003. Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. J. Abnorm. Psychol. 112: 497– 507.
[39] Biederman, J. et al. 1997. Is ADHD a risk factor for psychoactive substance use disorders? Findings from a four‐year prospective follow‐up study. J. Am. Acad. Child Adolesc.
Psychiatry 36: 21– 29.
[40]Burke, J.D. et al. 2001. Which aspects of ADHD are associated with tobacco use in early adolescence? J. Child Psychol. Psychiatry 42: 493– 502.
[41] Kollins, S.H. et al. 2005. Association between smoking and attention‐deficit/hyperactivity disorder symptoms in a population‐based sample of young adults. Arch. Gen.
Psychiatry 62: 1142– 1147.
[42] Gerra, G. et al. 2005. Association of the serotonin transporter promoter polymorphism with smoking behavior among adolescents. Am. J. Med. Genet. Part B: Neuropsychiatr.
Genet. 135: 73– 78.
[43] Hutchison, K.E. et al. 2002. The DRD4 VNTR polymorphism influences reactivity to smoking cues. J. Abnorm. Psychol. 111: 134– 143.
[44] McClernon, F.J. et al. 2008. Interactions between genotype and retrospective ADHD symptoms predict lifetime smoking risk in a sample of young adults. Nicotine Tob. Res. 10: 117– 127.
[45] Hutchison, K.E. et al. 2002. The DRD4 VNTR polymorphism influences reactivity to smoking cues. J. Abnorm. Psychol. 111: 134– 143.
21
[46] Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2007 Dec 12;298(22):2654-64.
[47] Wareham NJ, Ness EM, Byrne CD, Cox BD, Day NE, Hales CN. Cigarette smoking is not associated with hyperinsulinemia: evidence against a causal relationship between smoking and insulin resistance. Metabolism. 1996;45(12):1551-1556.
[48] Attvall S, Fowelin J, Lager I, Von Schenck H, Smith U. Smoking induces insulin
resistance–a potential link with the insulin resistance syndrome. J Intern Med. 1993;233(4):327-332.
[49] Facchini FS, Hollenbeck CB, Jeppesen J, Chen YD, Reaven GM. Insulin resistance and cigarette smoking. Lancet. 1992;339(8802):1128-1130.
[50] Talamini G, Bassi C, Falconi M, et al. Alcohol and smoking as risk factors in chronic pancreatitis and pancreatic cancer. Dig Dis Sci. 1999;44(7):1303-1311.
[51] Chiolero A, Wietlisbach V, Ruffieux C, Paccaud F, Cornuz J. Clustering of risk behaviors with cigarette consumption: a population-based survey. Prev Med. 2006;42(5):348-353.
[52] Ockene JK, Emmons KM, Mermelstein RJ, et al. Relapse and maintenance issues for smoking cessation. Health Psychol. 2000;19(1)(suppl):17-31.
[53] Simon JA, Seeley DG, Lipschutz RC, et al. The relation of smoking to waist-to-hip ratio and diabetes mellitus among elderly women. Prev Med. 1997; 26(5 pt 1):639-644.
[54] Ohlson LO, Larsson B, Svardsudd K, et al. The influence of body fat distribution on the incidence of diabetes mellitus: 13.5 years of follow-up of the participants in the study of men born in 1913. Diabetes. 1985;34(10):1055-1058.
[55] Windham GC, Mitchell P, Anderson M, et al. Cigarette smoking and effects on hormone function in premenopausal women. Environ Health Perspect. 2005; 113(10):1285-1290.
22
[56] Russell AE, Ford T, Williams R, Russell G. The Association Between Socioeconomic Disadvantage and Attention Deficit/Hyperactivity Disorder (ADHD): A Systematic Review. Child Psychiatry Hum Dev. 2016 06;47(3):440-58.
[57] Hwang J, Shon C. Relationship between socioeconomic status and type 2 diabetes: results from Korea National Health and Nutrition Examination Survey (KNHANES) 2010-2012. BMJ Open. 2014 Aug 19;4(8):e005710.
[58] Andrade SE, Lo JC, Roblin D, et al. Antipsychotic medication use among children and risk of diabetes mellitus. Pediatrics 2011;128:1135–41.
[59] Landau Z, Pinhas-Hamiel O. Attention Deficit/Hyperactivity, the Metabolic Syndrome, and Type 2 Diabetes. Curr Diab Rep. 2019 06 27;19(8):46.
![Table 3: Quality assessment by using the Newcastle-Ottawa Scale (NOS) [21] [22]](https://thumb-eu.123doks.com/thumbv2/5dokorg/5527777.144221/10.893.134.657.160.747/table-quality-assessment-using-newcastle-ottawa-scale-nos.webp)