ContentslistsavailableatScienceDirect
International
Journal
of
Surgery
Case
Reports
j o ur na l h o m e p a g e :w w w . c a s e r e p o r t s . c o m
Right
ectopic
paraesophageal
parathyroid
adenoma
with
refractory
hypercalcemia
in
pregnancy:
A
case
report
and
review
of
the
literature
Abdelrahman
Abusabeib
a,
Harun
Bhat
b,
Walid
El
Ansari
c,d,e,∗,
Mohamed
S.
Al
Hassan
a,
Abdelrahman
Abdelaal
aaDepartmentofGeneralSurgery,HamadGeneralHospital,HamadMedicalCorporation,Doha,Qatar bWeillCornellMedicineinQatar,Doha,Qatar
cDepartmentofSurgery,HamadGeneralHospital,HamadMedicalCorporation,Doha,Qatar dCollegeofMedicine,QatarUniversity,Doha,Qatar
eSchoolofHealthandEducation,UniversityofSkovde,Skovde,Sweden
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received2October2020 Accepted20October2020 Availableonline28October2020
Keywords:
Ectopicparathyroidadenoma Paraesophageal
Pregnancy
Primaryhyperparathyroidisminpregnancy
a
b
s
t
r
a
c
t
INTRODUCTION:Ectopicparathyroidadenomaisrareduringpregnancybutposesmultiplechallengesin treatment.Itpresentsasprimaryhyperparathyroidismwhichleadstosymptomsandcomplicationsof hypercalcemiainboththemotherandfetus.
PRESENTATIONOFCASE:A38-year-oldSudanesefemalepresentedwithdiffusebonepainandpolyuria. Laboratoryinvestigationsrevealedelevatedserumcalciumandparathyroidhormone.Ultrasoundofthe neckdidnotshowanyabnormallesion,however99mTc-sestamibiscanshowedarightsidedparathyroid adenoma,andanearlierCTscanshowedtheadenomatobeinanectopicparaesophagealposition. Focusedsurgicalneckexplorationwasdone,andtheectopicparathyroidadenomawasexcised. DISCUSSION:Preoperativelocalizationoftheectopicparathyroidadenomaallowsforafocusedsurgical procedure.Ultrasoundisthesafestduringpregnancy,but99mTc-sestamibiandCTscanmaybenecessary ifultrasoundorinitialbilateralneckexplorationdonotdetectanyadenoma.Mildelevationsinmaternal serumcalciumcanhavedetrimentaleffectsonthefetuswhichsuggeststhatasurgicalapproachmaybe necessaryinthemajorityofcases.
CONCLUSIONS:Ectopicparathyroidadenomaisrareduringpregnancyandisdetrimentaltoboththe motherandfetus.Preoperativelocalizationallowsforafocusedsurgerywhichisadefinitivetreatment andcansafelybeperformedduringthe2ndtrimesterofpregnancy.
©2020TheAuthor(s).PublishedbyElsevierLtdonbehalfofIJSPublishingGroupLtd.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Background
Theparathyroidglands(PG)arefoursmallglandsonthe poste-rioraspectofthelaterallobesofthethyroidgland.Thesuperiorand inferiorglandsareusuallysymmetrical;however,theiranatomical positionsvariesduetotheirlinesofembryologicaldescentfrom the4thand3rdbranchialpouchesrespectively[1].PGwhich devi-atefromnormalpositionsareectopic,andtheirlocationisrelated tothesameoriginsoftheparathyroid,thyroid,andthymictissue [2].Theprevalenceofectopicparathyroidgland(EPG)rangesfrom 28–42.8%(autopsyseries)to6.3–16%(smallerseriesstudies)[1]. Forinstance,othersreporteda7%incidenceofparaesophagealEPG [3,4].
AprimarypathologyofthePGisaparathyroidadenoma(PA) resultinginprimaryhyperparathyroidismwithrefractory
hyper-∗ Correspondingauthorat:DepartmentofSurgery,HamadGeneralHospital, HamadMedicalCorporation,Doha,Qatar.
E-mailaddress:welansari9@gmail.com(W.ElAnsari).
calcemia. This is the third most common endocrine disorder worldwide[5], andfemales areaffected astwiceasmales. Pri-maryhyperparathyroidisminpregnancy,however, israre,with 0.15–1.4%prevalence[6].Theinitialpresentationofprimary hyper-parathyroidismincludesgeneralizedfatigue,proximalweakness andincreasedfrequencyofurination,allofwhichcanbemistaken tobepartofthenormaleffects ofpregnancy,thereforeleading toadelayeddiagnosis.Inaddition,maternalserumcalciummay notbesignificantlyelevatedduetothephysiologiceffectsof preg-nancythatincludedecreasedserumalbuminlevelsandincreased glomerularfiltrationrate[7].
Duringpregnancy,primaryhyperparathyroidismneedstobe diagnosedasearlyaspossibleinordertoavoidthehighly delete-riouseffectsofhypercalcemiaonthemotheranddevelopingfetus [8].Fromthematernalside,veryhighserumcalciumlevelsmay present as hyperemesis,nephrolithiasis, recurrenturinary tract infection,andpancreatitis;asforthebaby,therecouldbepreterm delivery,lowbirthweightandfetaldemise,aswellashypocalcemia
https://doi.org/10.1016/j.ijscr.2020.10.093
2210-2612/©2020TheAuthor(s).PublishedbyElsevierLtdonbehalfofIJSPublishingGroupLtd.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http://
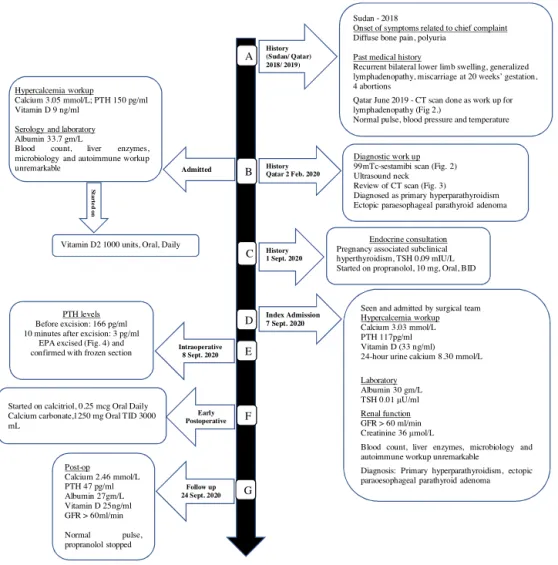
Fig.1.Timelineandsequenceofeventsover3years.
Normalvalues:Calcium(2.15–2.50mmol/L),PTH(10–65pg/mL),Albumin(35–50g/L),VitaminD(35–80ng/mL),GFR(>60mL/min),Creatinine(44–97mol/L),24-hurine
calcium(2.50–7.50mmol/Lper24h),TSH(0.4–4.0mIU/L).
andtetany(secondarytofetalparathyroidhormonesuppression) intheimmediateneonatalperiod[9,10].
Tothebestofourknowledge,thiscouldbetheseventhcase globally and the second reported case from the MENA region (MiddleEastandNorthAfrica)ofprimaryhyperparathyroidismin pregnancyduetoectopicparathyroidadenoma(EPA).Wereport thiscaseinlinewiththeupdatedconsensus-basedsurgicalcase report(SCARE)guidelines[11].Inaddition,weundertooka litera-turereviewofEPApresentingduringpregnancy.
2. Casepresentation
A38yearoldSudanesefemaleof15weeksgestation(gravida 9para4)cametoourThyroidSurgeryoutpatientclinicatHamad GeneralHospitalinDoha(largesttertiarycarefacilityinQatar), referredfromobstetrics,witha2yearhistoryofgeneralizedbone pain most prominent in the hands, palpitation, and increased frequencyofurination.Thesesymptomsgraduallyprogressedin severityandwereaffectingherqualityoflife.Shedeniedany nau-sea,vomiting,constipationorflankpain.
Pastmedicalhistory(Fig.1A)wassignificantforchronic gener-alizedlymphadenopathyandrecurrentlowerbilaterallowerlimb swelling(possiblelymphedema).Herlast5pregnanciesbeforethe current pregnancy resultedin 4 abortions anda miscarriage at 20-weekgestation,withnocleardiagnosis.Familyhistory,social history and review ofsystems wereunremarkable. Shedidnot
smoketobaccoandneverconsumedalcohol.Physicalexamination showedbilaterallowerlimbedema.Theremainderofthephysical examwasunremarkable.Onadmission,herpulse,bloodpressure andtemperaturewerewithinnormal.
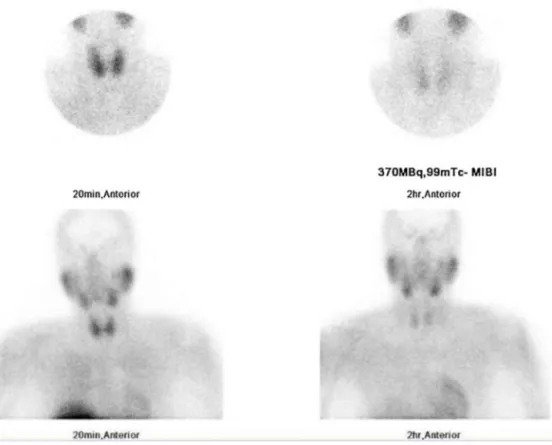
On initial admission to the medical team, a hypercalcemia workupwasdone(Fig.1B).Serologyandlaboratorytestsshowed elevatedcorrectedcalciumandintactparathyroidhormone(PTH), andlowvitaminD.Hercompletebloodcountandliverenzymes findingswerewithinnormal limitsandurinalysis,microbiology andautoimmuneworkupswereunremarkable.Adiagnosisof pri-maryhyperparathyroidismwasmadewhichwarrantedimaging ofthePG(Fig.1B).Ultrasound(US)oftheneckdidnotidentify parathyroidlesions; anearlier99mTc-sestamibiscan(sestamibi scan)undertakenbeforehercurrentpregnancy(Fig.2)revealed activityatthelowerpoleoftherightthyroidlobesuggestingaright inferiorPA;and,herCTscantakenayearearlier(Fig.3)asworkup forgeneralizedlymphadenopathyshowedanectopicrightinferior paraesophagealparathyroidlesion(7mmdiameter)impressiveof rightinferiorPA.
Shewasreferred urgentlytoourthyroid surgery clinic,and was18weekspregnantwithhypercalcemiaduetoprimary hyper-parathyroidismassociatedwithsubclinicalhyperthyroidismwhich wasmanagedwithbetablockeronly(Fig.1C).Thepatientwasthen seenandadmittedtooursurgicalteam(indexadmission,Fig.1D). ApartfromherhighserumcalciumandPTH,laboratorytestsand renalfunctionwerewithinnormal,andbasedontheprevious
ses-Fig.2. Earlyandlate99mTc-sestamibiscintigraphyparathyroidscanimagesofneckandmediastinumanteriorlyat20minand2hshowingincreasedfocaluptakesuggestive
ofrightinferiorparathyroidadenoma.
Fig.3. ACoronal,BaxialandCsagittalviewsCTscanoftheneckshowingtheectopicparathyroidadenoma(redarrow)locatedinaparaoesophagealposition,trachea(green
Fig.4. ExcisedparaesophagealPA.
tamibi scanandCT(Fig.1B,andFigs. 2and3),thediagnosisof primaryhyperparathyroidismduetoEPA(paraoesophageal)was confirmed.
The patient was admitted for urgent parathyroidectomy. Focusedneckexplorationbyanexperiencedseniorsurgeon con-firmedthatthePGwasnotatitsnormalanatomicalposition,and thatthePAwasectopic(paraesophageal),posteriortotherecurrent laryngealnerve.FrozensectionshistologicallyconfirmedPA,and intraoperativerapidPTHmonitoringbeforeexcisionand 10min after excisionofthe PA,showeda serumPTH decreaseby 98% (Fig.1E)confirmingtheremovalofthehypersecretinggland(Fig.4). Onthefirstpostoperativeday,thepatientdevelopedmild symp-tomsandsignsofhypocalcemia,thelaboratoryfindingsrevealed lowintactPTH(1pg/mL)andserumcalcium(1.9mmol/L),andshe wasgiventreatment(Fig.1F).Aweeklater,followupatour thy-roidsurgeryclinicrevealedthatthepatientdidnotcomplainofany ofthesymptomsofhypercalcemiaexperiencedpriortosurgery, orsymptomsofhypocalcemiathat developedintheearly post-operativeperiod,andshehadnormallaboratoryfindings(Fig.1G), andhistopathologyshowedfindingsconsistentwithhypercellular parathyroidtissue,compatiblewithPA(1.5×0.7×0.4cm) weight-ing0.1g.
3. Discussion
Calciumhomeostasisduringpregnancyavoidshypercalcemia and itscomplicationsinthemotherandfetus.Wereporta rare case ofapregnantfemalewithectopic rightparaesophageal PA leadingtohyperparathyroidismandhypercalcemia.Such hyper-calcemia mighthavebeenpossiblyresponsibleforherprevious foursuccessiveabortionsandonemiscarriageintheperiodprior tohercurrentpregnancy.FetalPGdevelopafterthefirsttrimester, hencematernalserumcalciumlevelsdictatecalciumhomeostasis in thefetusduringthistime [12].Elevatedmaternalserum cal-ciumresultsinfetalhypercalcemia[13],andasfetalPGdevelop, fetalhypercalcemiasuppressesthefetalPGthatpredisposesthe fetustopostpartumhypocalcemiaoncecalciumdeliveryfromthe motherceasesafterbirthandthefetusisunabletomobilizecalcium fromthebones[14].Ourcasedemonstratesdysregulatedcalcium homeostasis evidenced by themother’s symptomatic presenta-tionandpreviousabortionsandmiscarriage,possiblyasaresult ofhypercalcemia.
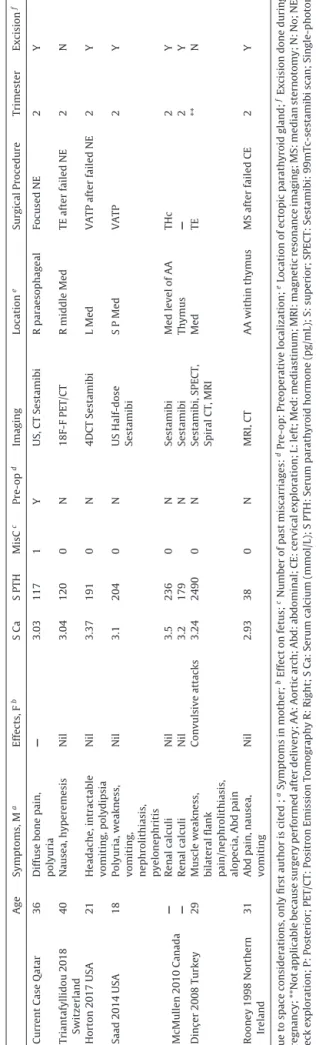
Table 1 shows that ourpatient’s presentation withpolyuria agrees withcasesidentified in theliteraturereview we under-took[15],butshehadnorenalcomplicationse.g.,nephrolithiasis andpyelonephritis,contrarytootherreports[6,15,16].Her com-plaint of bone pain was alsonot commonly reported by other Table
1 Comparison of current case with other similar cases of ectopic parathyroid adenomas presenting in pregnancy identified in the literature review. Age Symptoms, M a Effects, F b S Ca S PTH MisC c Pre-op d Imaging Location e Surgical Procedure Trimester Excision f Current Case Qatar 36 Diffuse bone pain, polyuria — 3.03 117 1 Y US, CT Sestamibi R paraesophageal Focused NE 2 Y Triantafyllidou 2018 Switzerland 40 Nausea, hyperemesis Nil 3.04 120 0 N 18F-F PET/CT R middle Med TE after failed NE 2 N Horton 2017 USA 21 Headache, intractable vomiting, polydipsia Nil 3.37 191 0 N 4DCT Sestamibi L Med VATP after failed NE 2 Y Saad 2014 USA 18 Polyuria, weakness,
vomiting, nephrolithiasis, pyelonephritis
Nil 3.1 204 0 N US Half-dose Sestamibi S P Med VATP 2 Y McMullen 2010 Canada — Renal calculi Nil 3.5 236 0 N Sestamibi Med level of AA THc 2 Y — Renal calculi Nil 3.2 179 N Sestamibi Thymus — 2 Y Dinc ¸ er 2008 Turkey 29 Muscle weakness, bilateral flank pain/nephrolithiasis, alopecia, Abd pain Convulsive attacks 3.24 2490 0 N Sestamibi, SPECT, Spiral CT, MRI Med TE ** N Rooney 1998 Northern Ireland 31 Abd pain, nausea, vomiting Nil 2.93 38 0 N MRI, CT AA within thymus MS after failed CE 2 Y Due to space considerations, only first author is cited ; aSymptoms in mother; bEffect on fetus; cNumber of past miscarriages: dPre-op: Preoperative localization; eLocation of ectopic parathyroid gland; fExcision done during pregnancy; **Not applicable because surgery performed after delivery; AA: Aortic arch; Abd: abdominal; CE: cervical exploration; L: left; Med: mediastinum; MRI: magnetic resonance imaging; MS: median sternotomy; N: No; NE: Neck exploration; P: Posterior; PET/CT: Positron Emission Tomography R: Right; S Ca: Serum calcium (mmol/L); S PTH: Serum parathyroid hormone (pg/mL); S: superior; SPECT: Sestamibi: 99mTc-sestamibi scan; Single-photon emission computed tomography; TE: thoracoscopic exploration; THc: Thoracotomy; Trimester: Trimester of pregnancy when surgery was performed; US: ultrasound; VATP: video assisted thoracoscopic parathyroidectomy; Y: Yes; – Computed Tomography; 18F-F: 18F-fluorocholine; — not reported.
authors(Table1).About67%ofwomenwithprimary hyperparathy-roidismhave symptomsofhypercalcemia,e.g.nausea,vomiting andconstipation,whicharenormalcomplaintsduringpregnancy [14,17]. In primary hyperparathyroidism duringpregnancy, the early mild hypercalcemia can be difficultto diagnose due two reasons: symptomscanbeoverlooked; and,normalphysiologic responses(increasedintravascularvolumeandglomerular filtra-tionthatleadtohemodilutionandgestationalhypoalbuminemia, hypercalciuria,and decreasedtotal bodycalcium) canmaskthe hypercalcemia[14,18,19].Despitesuchphysiologicresponses,our patienthadhighlevelofserumcalcium(3.03mmol/L).Asforthe investigations, ourcase demonstratestheimportance of identi-fyingEPApriortosurgeryinordertopreventunsuccessfulneck exploration and prolonged time of surgery. Preoperative local-ization ofEPAavoidsreoperationin>95%ofcases[20].CTand sestamibiareharmfultothefetus,butourpatienthadtheCTas aworkupforherlymphadenopathyandhadthesestamibiduring herinitialhypercalcemiaworkup,bothbeforepregnancy.USissafe duringpregnancybutisoperatordependent(possiblefalse nega-tivefindings),with27–89%sensitivityforEPAdetection[1].We encounteredsuchafalsenegativefinding(USdidnotdetectthe EPA),inagreementwithothers[12](Table1).LocalizationofEPA inpregnancyisdifficult,USistheimagingofchoice,butfurther imagingmayberequiredtolocalizetheEPA.Sestamibiscanis use-fulforpreoperativeidentificationofEPA(80–99%sensitivity)[21], anditsuccessfullyidentifiedourpatient’sPAbutdidnotlocalizeits ectopicposition.Inpregnancy,lowdosesestamibiscanisunlikely tobedetrimental[22];andCTiscontraindicatedinpregnancybut maybeusedwithappropriateabdominalshielding[6,23](Table1). Combinedimaging(sestamibiandCT)enhancethediagnosis, detectingthemostabnormalglands[6]. Suchcombinationafter failedneckexplorationcanensuresuccessofthesecondsurgery [6].18F-fluorocholinePET/CTmaylocalizeEPAinpregnancyafter negative/equivocalUSand/orscintigraphy/single-photonemission computedtomography(SPECT)[24].Amultidisciplinaryteamcan select theappropriateimaging withtheleastharmtoboth the motherandfetus[25].
The’true’EPAprevalenceremainsunconfirmed.Insmall stud-ies of patientsundergoing neckre-exploration, prevalencewas 29–45%[1].EPAcanlocatewithinthemediastinumasobserved inTable1[6,12,15,16,24]orthymus[23].
Nephrolithiasis, bone disease, and pancreatitis complicate hypercalcemia due to primary hyperparathyroidism [17]. Post-delivery,themothernolongerprovidesthefetus,whichexposes her to veryhigh calciumlevels (lifethreatening hypercalcemic crisis)[9,26].Postpartumfetalhypocalcemia(convulsiveattacks) withmaternal bilateralnephrolithiasis havebeenreported[16] (Table 1). Fetal complications include fetal demise, low birth weight,pretermdelivery,anddepressedfetalparathyroidleading topostpartumneonatalhypocalcemia/tetany[9,14,27].Ourcase had no complications:diagnosiswasdoneat theindex admis-sion,and withintwo weeks,urgent surgery(EPAexcision)was undertakeninthesecondtrimesterandfollowupbyobstetrician confirmeduneventfulpost-operativeperiodformotherandfetus. Thisisinsupportoftheimportanceofearlysuspicionand diagno-sispriortoseverepresentations,increasedmorbidityandmortality [8].
As for miscarriage, hyperparathyroidism is associated with 3.5 timesincreaseinmiscarriage[8].Roughly>50%of primary hyperparathyroidisminpregnancyisundiagnosed;72%of preg-nantwomenhadhypercalcemiaatmiscarriage,suggestingdelayed diagnosis; and serumcalciumas lowas 10.7mg/dL ledto mis-carriage [8]. This warrants thorough investigations in order to excludePHA-primaryhyperparathyroidism.Duetoourpatient’s history of overlap ofpreviousabortions/miscarriageand symp-toms ofhypercalcemia,it is possiblethat thepatient’s primary
hyperparathyroidism(undiagnosedatthattime)couldhavebeen responsibleforhermiscarriageinSudanbeforeweencountered herinQatar.Weareunabletoconfirmsuchspeculationasthedata isnotavailable.
Asformanagement,surgicalproceduresdependontheEPA’s location(Table1).WelocalizedtheEPAbeforesurgery,and under-tookrightsidedfocusedparathyroidectomy,whichisaseffective asbilateralneckdissection,butassociatedwithbetterscarsand patientsatisfaction,andshorteroperativetimeandhospitalstay [28].Othertechniquesincludemediansternotomyformediastinal EPA[23],andless invasivevideoassistedthoracoscopic surgery [16].
Apregnantpatientraisesconcernsaboutthesafetyofgeneral anesthesiaandsurgery.Theargumentagainstparathyroidectomy duetoteratogeniceffectsofgeneralanesthesiamaybe overex-aggerated[6] as modern-day anesthesia can be used safely in pregnancy[29,30].Inaddition,surgery(parathyroidectomy)has much lower neonatal complications compared to conservative therapy[17,31].Parathyroidectomyis safewhencarried outby experiencedsurgeons[8],andsurgeryprovidesacurative treat-mentwhichremovestherisksofmaternalandfetalhypercalcemia as well as post-partum fetal hypocalcemia [31]. Conservative management(oralhydrationandbisphosphonates)issometimes recommended,althoughevenmildhypercalcemiacanleadto sig-nificantmaternal complicationsand neonataltetany[8,31]. The lackofatightlydefinedrelationshipbetweenserumcalciumlevel andtheabilitytopredictmaternalorfetalcomplicationssuggests thatmildhypercalcemiamaystillrequiredefinitivesurgical man-agement[6].
Thecurrentcasedemonstratedasuccessfulfocusedneck explo-rationundertaken duringthe2ndtrimester whichis anagreed optimal time for surgery [32]. For women diagnosed with PA andareplanningtogetpregnant,informationshouldbeprovided regardingthedifficultyandrisksassociatedwiththemanagement ofprimaryhyperparathyroidismduringpregnancy[33].
4. Conclusion
EPAinpregnancyisrare,withchallengesindiagnosisand man-agement.A highindex ofsuspicion is useful,andas even mild elevationsof maternalserumcalciumcanexertpotential nega-tiveeffectsonthefetus,asurgicalapproachshouldbeconsidered overconservativetherapy.Amultidisciplinaryapproachisrequired inordertoselectthesafestimagingmodalitiesforpre-operative localizationoftheEPAinpregnancywhichwillallowforafocused, shorterandlessinvasivesurgicalprocedure.Theprocedureshould beperformedbyanexperiencedsurgeontakinginto considera-tiontheectopiclocationofthePAandthepotentialintraoperative technicaldifficultiesandmorbiditiesrelatedtoboththemother andfetus.
DeclarationofCompetingInterest
Theauthorsreportnodeclarationsofinterest.
Funding
Nothingtodeclare.
Ethicalapproval
ApprovedbyMedicalResearchCenter,HamadMedical Corpo-rationreferencenumber(MRC-04-20-859).
Consent
Writteninformedconsentwasobtainedfromthepatientfor publicationofthiscasereportandaccompanyingimages.Acopy ofthewrittenconsentisavailableforreviewbytheEditor-in-Chief ofthisjournalonrequest.
Registrationofresearchstudies
NotfirstinMan.
Guarantor
ProfDrWalidElAnsari.
Provenanceandpeerreview
Notcommissioned,externallypeer-reviewed.
CRediTauthorshipcontributionstatement
Abdelrahman Abusabeib: Investigation,Writing - review &
editing.HarunBhat:Investigation,Writing-originaldraft, Writ-ing-review&editing.WalidElAnsari:Investigation,Supervision, Projectadministration,Writing-originaldraft,Writing-review &editing.MohamedS.AlHassan:Investigation,Project admin-istration, Writing - review & editing. Abdelrahman Abdelaal:
Investigation,Projectadministration,Writing-review&editing.
References
[1]G.Noussios,Ectopicparathyroidglandsandtheiranatomical,clinicaland
surgicalimplications,Exp.Clin.Endocrinol.Diabetes120(2012)604–610.
[2]R.Bliss,P.Gauger,L.Delbridge,Surgeon’sapproachtothethyroidgland:
surgicalanatomyandtheimportanceoftechnique,WorldJ.Surg.24(2000)
891–897.
[3]R.Phitayakorn,C.R.McHenry,Incidenceandlocationofectopicabnormal
parathyroidglands,Am.J.Surg.191(2006)418–423.
[4]V.Mendoza,C.Ramírez,A.Espinoza,G.González,J.Pe ˜na,M.Ramírez,I.
Hernández,M.Mercado,Characteristicsofectopicparathyroidglandsin145
casesofprimaryhyperparathyroidism,Endocr.Pract.(2010)977–981.
[5]T.Madkhali,A.Alhefdhi,H.Chen,D.Elfenbein,Primaryhyperparathyroidism,
Ulus.TravmaAcilCerrahiDerg.32(2016)58–66.
[6]T.P.W.McMullen,D.L.Learoyd,D.C.Williams,Hyperparathyroidismin
pregnancy:optionsforlocalizationandsurgicaltherapy,WorldJ.Surg.34
(2010)1811–1816.
[7]C.Marcocci,F.Cetani,Clinicalpractice.Primaryhyperparathyroidism,N.Engl.
J.Med.365(2011)2389–2397.
[8]J.Norman,D.Politz,L.Politz,Hyperparathyroidismduringpregnancyandthe
effectofrisingcalciumonpregnancyloss:acallforearlierintervention,Clin.
Endocrinol.71(2009)104–109.
[9]K.C.Kort,H.J.Schiller,P.J.Numann,Hyperparathyroidismandpregnancy,Am.
J.Surg.177(1999)66–68.
[10]M.T.Truong,M.L.Lalakea,P.Robbins,M.Friduss,Primary
hyperparathyroidisminpregnancy:acaseseriesandreview,Laryngoscope
118(2008)1966–1969.
[11]R.A.Agha,M.R.Borrelli,R.Farwana,K.Koshy,A.Fowler,D.P.Orgill,Forthe
SCAREGroup,TheSCARE2018statement:updatingconsensusSurgical
CAseREport(SCARE)guidelines,Int.J.Surg.60(2018)132–136.
[12]W.B.Horton,M.M.Stumpf,J.D.Coppock,Gestationalprimary
hyperparathyroidismduetoectopicparathyroidadenoma:casereportand
literaturereview,J.Endocr.Soc.1(2017)1150–1155.
[13]D.J.Hosking,Calciumhomeostasisinpregnancy,Clin.Endocrinol.45(1996)
1–6.
[14]N.G.Mokrysheva,A.K.Eremkina,S.S.Mirnaya,Acaseofpregnancy
complicatedbyprimaryhyperparathyroidismduetoaparathyroidadenoma,
Am.J.CaseRep.20(2019)53–59.
[15]A.F.Saad,L.D.Pacheco,M.M.Costantine,Managementofectopicparathyroid
adenomainpregnancy,Obstet.Gynecol.124(2014)478–480.
[16]S.I.Dinc¸er,A.Demir,H.V.Kara,M.Z.Günlüoglu,Thoracoscopicremovalofa
maternalmediastinalectopicparathyroidadenomacausingneonatal
hypocalcemia:acasereport,Ann.Thorac.Cardiovasc.Surg.14(2008)
325–328.
[17]P.F.Schnatz,S.L.Curry,Primaryhyperparathyroidisminpregnancy:
evidence-basedmanagement,Obstet.Gynecol.Surv.57(2002)365–376.
[18]S.Malekar-Raikar,B.P.Sinnott,Primaryhyperparathyroidisminpregnancy—a
rarecauseoflife-threateninghypercalcemia:casereportandliterature
review,CaseRep.Endocrinol.2011(2011)516–520.
[19]T.Dahlman,H.E.Sjoberg,E.Bucht,Calciumhomeostasisinnormalpregnancy
andpuerperium.Alongitudinal6CaseReportsinEndocrinologystudy,Acta
Obstet.Gynecol.Scand.73(1994)393–398.
[20]W.Shen,M.Düren,E.Morita,Reoperationforpersistentorrecurrentprimary
hyperparathyroidism,Arch.Surg.131(1996)861–869.
[21]K.S.Norton,L.W.Johnson,F.D.Griffen,J.Burke,S.Kennedy,D.Aultman,Li.BD,
G.Zibari,Thesestamibiscanasapreoperativescreeningtool,Am.Surg.68
(2002)812–815.
[22]S.R.Moosvi,S.Smith,J.Hathorn,T.Groot-Wassink,Evaluationoftheradiation
doseexposureandassociatedcancerrisksinpatientshavingpreoperative
parathyroidlocalization,Ann.R.Coll.Surg.Engl.99(2017)363–368.
[23]D.P.Rooney,A.I.Traub,C.F.Russell,Cureofhyperparathyroidismin
pregnancybysternotomyandremovalofamediastinalparathyroidadenoma,
Postgrad.Med.J.74(1998)233–234.
[24]MariaTriantafyllidou,etal.,Localisationofectopicmediastinalparathyroid
adenomaby18F-fluorocholinePET/CT,BMJCaseRep.2018(2018),
bcr2017222089.
[25]E.Malheiro,N.Chabbert-Buffet,J.N.Talbot,S.Périé,Hyperparathyroidismin
pregnancyand99mTc-MIBIscintigraphy,Eur.Ann.Otorhinolaryngol.Head
NeckDis.136(2019)501–503.
[26]M.J.Carella,V.V.Gossain,Hyperparathyroidismandpregnancy:casereport
andreview,J.Gen.Intern.Med.4(1992)448–453.
[27]D.Hirsch,V.Kopel,V.Nadler,S.Levy,Y.Toledano,G.Tsvetov,Pregnancy
outcomesinwomenwithprimaryhyperparathyroidism,J.Clin.Endocrinol.
Metab.100(2015)2115–2122.
[28]J.Westerdahl,A.Bergenfelz,Unilateralversusbilateralneckexplorationfor
primaryhyperparathyroidism:five-yearfollow-upofarandomized
controlledtrial,Ann.Surg.246(2007)976–980.
[29]P.G.Duncan,Fetalriskofanesthesiaandsurgeryduringpregnancy,
Anesthesiology64(1986)790–794.
[30]B.C.Visser,R.E.Glasgow,K.K.Mulvihill,S.J.Mulvihill,Safetyandtimingof
nonobstetricabdominalsurgeryinpregnancy,Dig.Surg.18(2001)409–417.
[31]T.R.Kelly,Primaryhyperparathyroidismduringpregnancy,Surgery110
(1991)1028–1033.
[32]P.Pothiwala,S.Levine,Parathyroidsurgeryinpregnancy:reviewofthe
literatureandlocalizationbyaspirationforparathyroidhormonelevels,J.
Perinatol.29(2009)779–784.
[33]A.N.DiMarco,K.Meeran,I.Christakis,V.Sodhi,C.N.Piercy,N.S.Tolley,F.F.
Palazzo,Seventeencasesofprimaryhyperparathyroidisminpregnancy:acall
formanagementguidelines,J.Clin.Endocrinol.Metab.3(2019)1009–1021.
OpenAccess
ThisarticleispublishedOpenAccessatsciencedirect.com.ItisdistributedundertheIJSCRSupplementaltermsandconditions,which permitsunrestrictednoncommercialuse,distribution,andreproductioninanymedium,providedtheoriginalauthorsandsourceare credited.